Acute vs chronic pain. All you need to know!
Acute vs chronic pain.
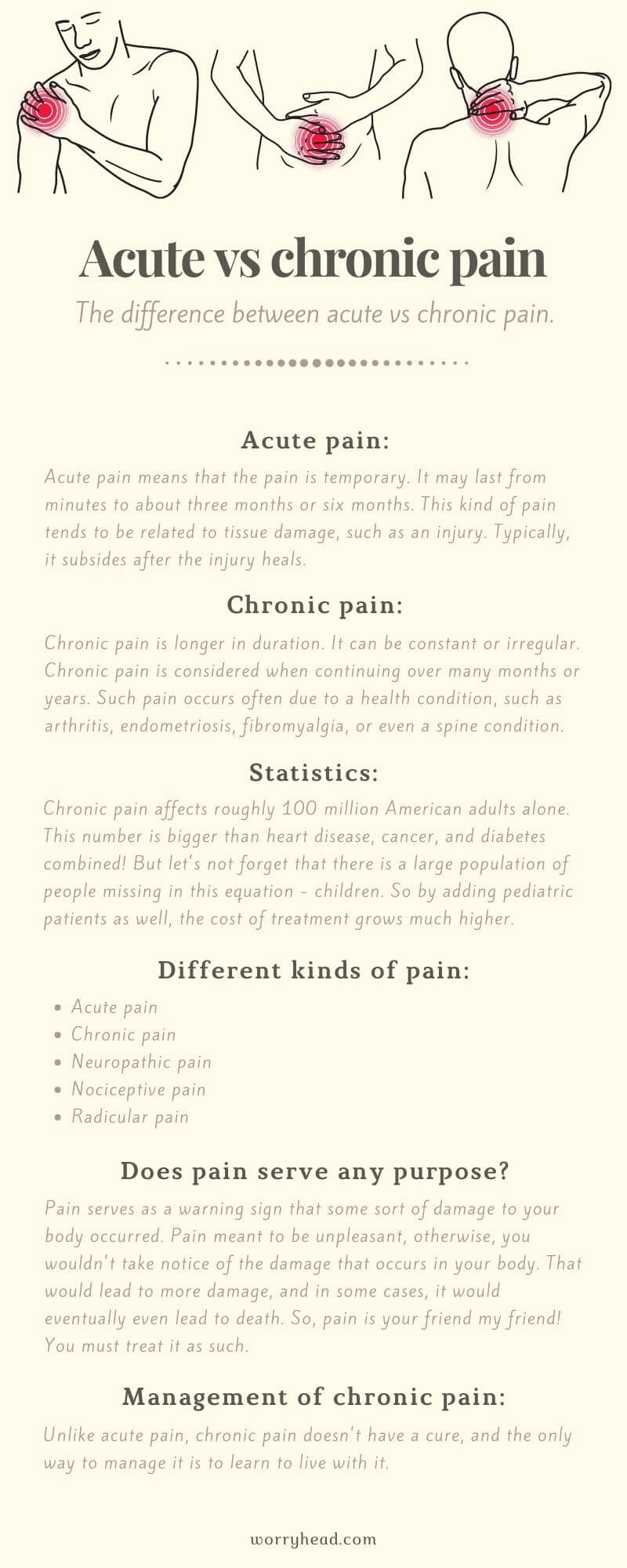
The difference between acute vs chronic pain is that after acute pain goes away, you can go on with life as usual. Chronic pain, however, is pain that is ongoing and usually lasts longer than six months.
Here are the main differences:
Acute pain means that the pain is temporary. It may last from minutes to about three months or six months.
This kind of pain tends to be related to tissue damage, such as an injury. Typically, it subsides after the injury heals.
Acute pain may in some cases evolve into chronic pain. It may happen, if the injury doesn’t heal correctly or if there is a pain signals problem.
Chronic pain is longer in duration. It can be constant or irregular, but it always comes back.
Chronic pain is considered when continuing over many months or years. Such pain occurs often due to a health condition, such as arthritis, endometriosis, fibromyalgia, or even a spine condition.
Statistics.
I want to focus on chronic pain because it is often one of the main symptoms of chronic illness.
Before we dive into the simplified science of chronic pain I’d like to explore some important statistics:
Chronic pain affects roughly 100 million American adults alone. This number is bigger than heart disease, cancer, and diabetes combined!
The estimated annual cost is of medical treatment is about $500-600 billion in the U.S. alone.
But let’s not forget that there is a large population of people missing in this equation – children. So by adding pediatric patients as well, the cost of treatment grows much higher.
So, pain is something that really needs to be addressed, especially because of the fact that your partner or yourself suffers from it.
Chronic illness…
My wife suffers from endometriosis and fibromyalgia. She used to experience daily, excruciating pain but never knew the reason behind it.
During the period of time, from experiencing her first symptoms until the day of endometriosis diagnosis, M experienced a lot of anxiety and even developed depression which almost cost her life.
Only thanks to her strong spirit and my unconditional support, did she manage to get off antidepressants and get out of depression. However, the physical pain persisted, leaving more questions than answers.
Fast forward to this day, my wife and I began to learn about the science behind the pain. M experienced it first hand, I had, however, a lot to learn…
The subject of chronic pain got me so interested because I wanted to help my wife by understanding what she was going through. I couldn’t support her fully without understanding how pain really works.
This article, “acute vs chronic pain”, aims to provide you with a better understanding of what your partner, or yourself, might be going through.

Different kinds of pain!
Medically speaking, pain is an uncomfortable sensation that usually signals an injury or illness, therefore the most known to people there are acute and chronic pain.
But that’s not all, there are 5 types of pain:
- Acute pain
- Chronic pain
- Neuropathic pain
- Nociceptive pain
- Radicular pain
Acute pain means that the pain is temporary. It may last from minutes to about three months or six months.
This kind of pain tends to be related to tissue damage, such as an injury. Typically, it subsides after the injury heals.
The difference between acute vs chronic pain is that acute pain may in some cases evolve into chronic pain. It may happen, if the injury doesn’t heal correctly or if there is a pain signals problem.
Chronic pain is longer in duration. It can be constant or irregular, but it always comes back.
Chronic pain is considered when continuing over many months or years. Such pain occurs often due to a health condition, such as arthritis, endometriosis, fibromyalgia, or even a spine condition.
Neuropathic pain is caused by damage to the nerves or other parts of the nervous system. It is often described as a shooting, stabbing, or burning sensation.
It may even feel like pins and needles. In illnesses like fibromyalgia, it can also affect sensitivity to touch and can make someone have difficulty feeling hot or cold sensations, therefore neuropathic pain is a common type of chronic pain.
Such pain can interfere with normal movement leading to mobility issues.
Nociceptive pain is a type of pain that is similar to acute pain because it is caused by damage to tissue.
However, people often describe it as sharp, achy, or throbbing. This type of pain is often experienced in your joints, muscles, skin, tendons, and bones. It can be also both, acute and chronic.
Radicular pain is a very specific type of pain that can occur when your spinal nerve gets compressed or inflamed. It often radiates from your back and hips into the legs.
Radicular pain may cause tingling, numbness, and even muscle weakness. Pain that radiates from the back and into the leg is commonly known as sciatica pain because of the sciatic nerve being affected.
This type of pain is felt deep in the leg. Movement such as walking or sitting and some other activities can make sciatica worse. Sciatica is one of the most common forms of radicular pain.
The title mentions acute vs chronic pain because those kinds of pains are often misunderstood, however, there isn’t much to acute pain more than its simple explanation provided above…
Does pain serve any purpose?
Pain serves as a warning sign that some sort of damage to your body occurred.
In other words – pain is your friend, not your enemy. And why do people react negatively to pain? Because it’s unpleasant.
Pain is meant to be unpleasant, otherwise, you wouldn’t take notice of the damage that occurs in your body. That would lead to more damage, and in some cases, it would eventually even lead to death.
So, pain is your friend my friend! You must treat it as such.
But there is a but! Is every pain a warning sign? No. Not all pain is the same, here’s why:
In the case of acute pain, the hurt that we experience is a sign of harm, therefore avoidance of doing something about this kind of pain will increase damage.
In the case of chronic pain, the hurt that the person experience is very real, however, hurt is not a sign of immediate harm.
This is one of the biggest differences in acute vs chronic pain. It is often difficult for people to wrap their minds around it because it looks like a false alarm.
You experience pain but there is no clear, visible damage, or it may have occurred but healed a while ago, yet the sensation of pain is still present.
But there are more differences than this, for example, the causes…
In the case of acute pain, there is a very clear pathway, and there is often a single cause. In the case of chronic pain, there are many unknowns, it is multifactorial. We don’t often understand why that is.
Also, in the case of chronic pain, even if we can give it the name, it still does not mean we understand why that pain is persistent. We may call it fibromyalgia, we may call it neuropathic pain. It means we give it a name but we don’t understand much detail of it.
This has a significant impact on the treatment…
let’s take endometriosis as an example because the pain caused by this chronic illness, gives women a lot of problems because it’s invisible and no one can see it.
The very fact that you cannot explain how you feel, or you’re simply fed up with endless repeating, make you feel stressed.
This was always the case for my wife, and that is the case for many women.
What to do?
In the case of acute pain, there is a clear end-point. Often immobilization is essential for recovery, and also, medication.
Medication is very good for pain. But it is good for trauma pain, such as acute one.
Medication is not good for chronic pain! It’s a powerful tool but comes with plenty of side effects, therefore needs are perfect for acute pain because it doesn’t require long-term medication.
So, in the case of chronic pain, it’s a completely different situation. For one thing, there is no ending point, immobilization may worsen the pain, but it doesn’t mean that we have to go to another extreme and move too much.
Medication in chronic pain needs to be used with caution!
People develop tolerance to pain wanting to increase the dosage every so often. That can be dangerous because they need more and more drugs to get the same effect. It may lead to addiction.
The problem is that when we develop tolerance to drugs, every time we increase the dosage, we increase the side effects. It can affect us not only physically but also mentally.
When the side effects become problematic, we look for other ways to deal with the pain, but alongside side effects, medication becomes also more costly.
Acute vs chronic pain is a subject of two completely separate pieces. Chronic pain conditions cannot be treated with an acute mentality.
Additionally, people may get their hopes up that there could be a new procedure, there could be a new medication, and that may result in emotional setbacks, stress, anxiety, and other mental health problems.
In order to help you manage your pain, the answer is in this very sentence – you need to manage it!
Management of chronic pain!
The management of chronic pain has the same approach as any other chronic condition which lacks a cure. It’s about improving the quality of life and functioning.
Chronic pain management requires:
- Medical optimization (CBD for example).
- Physical reconditioning (rehabilitation).
- Behavioral, lifestyle modification (pain psychologist).
Helping people become more aware of what these factors are, and how they influence pain, is a big part of behavioral and lifestyle modification.
People often think that they need to belong to only one of these categories, but in order to effectively treat chronic pain, we need to consider all the factors.
We really need to have a combination of all these factors and find the right balance between them, but we cannot focus on one. So, the idea is to help people understand how to live with chronic pain.
I can see you clenching and asking me a question – “what do you mean I have to live with chronic pain? That sounds horrible!” – unfortunately, that’s the only way.
When it comes to acute vs chronic pain, chronic pain doesn’t have a cure, and the only way to manage it is to learn to live with it.

How to learn to live with pain?
Pain affects many aspects of your life:
- Family, friends.
- Work, school.
- Sports, leisure.
- Self-care.
- Vacations, hobbies.
- Socializing, entertainment.
- Cooking, cleaning, errands.
In the beginning, as the one who suffers, you try to do all the things you used to, but you notice that pain may for instance impact the way you move. In my wife’s case, it was dancing…
M was a professional dancer who was struck by a chronic illness. The pain not only stopped her from doing something she loved but also affected her work, her income since she was a full-time dancer. Immediately it affected a few aspects of her life.
With time, it impacted her family and friends, including myself as her husband.
Naturally, pain impacted our sex life. There is no shame in it, it’s just the way it goes, and I have to be radically honest with you, it can be incredibly hard, but you mustn’t give up!
Not only pain stop my wife from doing simple chores like cleaning and cooking, but it also made her feel useless and like a burden, eventually costing her mental breakdown and thoughts, and attempts of suicide.
As you can see from my wife’s example, chronic pain can affect many aspects of your life and its management needs to be taken seriously.
Neglect of the management of chronic pain, or the wrong, acute approach, will impact you not only physically, but also mentally and financially.
There are no shortcuts, adjusting, and learning to live with pain takes time!
So, taking all this into account, how can you learn to live with pain?
It’s by addressing all of these factors of acute vs chronic pain, by addressing all aspects of your life.
No one said it’s easy. Many times, after trial and error, we both fell flat on our faces and we had to start all over again, trying to find another way, a different approach. It took time, but if we managed, you can manage too!
It is difficult to spot the difference between acute vs chronic pain.
It is not about fixing the pain, but about addressing one of the most important components here – your emotional state. I speak from the point of view of the supporter, but you must remember, it’s also hard on us.
In order to help your partner suffering from chronic illness and pain, you need to first think of yourself. If you cannot take care of your own mental well-being, you will not be able to take care of your partner. This is very important.
I am not talking about being selfish but about self-care.
Believe me, I fell into the trap of giving all my love and attention to my wife, and however it was undoubtedly vital in her struggles with suicidal thoughts, other times, I had to think of my own well-being. Otherwise, I would have a breakdown and both of us would be lost.
Pain can overshadow life. It’s not uncommon for chronically ill people to stop talking about family, hobbies, work. Instead, that person will talk about medication or the next procedure.
We have found with M, that many women suffering from endometriosis fall into the pattern of constant sharing on social media how they feel, and quite common, women take picture after picture of their bloated belly, posting it every 5 minutes.
My wife never wanted to be associated with that. To her, sharing photos of endometriosis bloated belly wasn’t the option. She doesn’t want people to feel sorry for her but treat her like they used to. She doesn’t want to fall into the selfie social media trap.
I personally feel that these women want to feel wanted, needed, and quite often the lack of understanding of their loved ones and friends leads to looking for understanding and appreciation elsewhere.
if you or your chronically ill partner feels trapped, the best thing you can do is to seek help from a CBT therapist specializing in chronic illness. My wife did just that, and it helped her immensely!
Her therapist understood how she felt and helped her focus on all the aspects of life affected by chronic pain. Ideally, as it was in the case of my M, physical therapy worked magic in combination with Cognitive-Behavioural Therapy.
Common components of psychological therapy are:
- Overview of pain.
- Pacing of activities.
- Pain & stress physiology.
- Relaxation training.
- Sleep hygiene.
- Identifying stressors.
- Stress management.
- Pain flare-ups management.

Stress and pain…
I can see a few worried heads nodding, “pain isn’t in my head”!
No, it isn’t, but what is important for you to recognize is the relationship between stress and pain.
What we all know about life is that it can be very stressful. Sometimes more often than we wished to. You can not get a pill for that. No pill will make stress go away, because stress often doesn’t come from you, but from the environment and actions of other people.
Stress is just a part of life!
It is important to know that stress can influence the way you experience pain. Stress greatly impacts chronic pain.
In order to understand how stress impacts chronic pain, you need to understand how the nervous system works!
The nervous system splits into two categories – central and peripheral.
The central nervous system affects the brain and spinal cord. The peripheral nervous system divides into somatic and autonomic. The autonomic system divides even further – into sympathetic and parasympathetic.
The sympathetic system activates your body to deal with stressful situations, the parasympathetic system helps your body return to a calmer state.
Let’s talk about the sympathetic system because it belongs to the automatic system, which as the name suggests, automatically controls your body.
The sympathetic system:
- Increases heart rate.
- Increases blood pressure.
- Increases muscle tension.
- Constricts blood vessels.
- Releases stress hormones.
- Changes in breathing patterns.
We can differentiate stress. For example, we can see the difference between being stressed by a barking dog, or by having an argument with a family member. But to the body stress is stress, and it will always activate the sympathetic system.
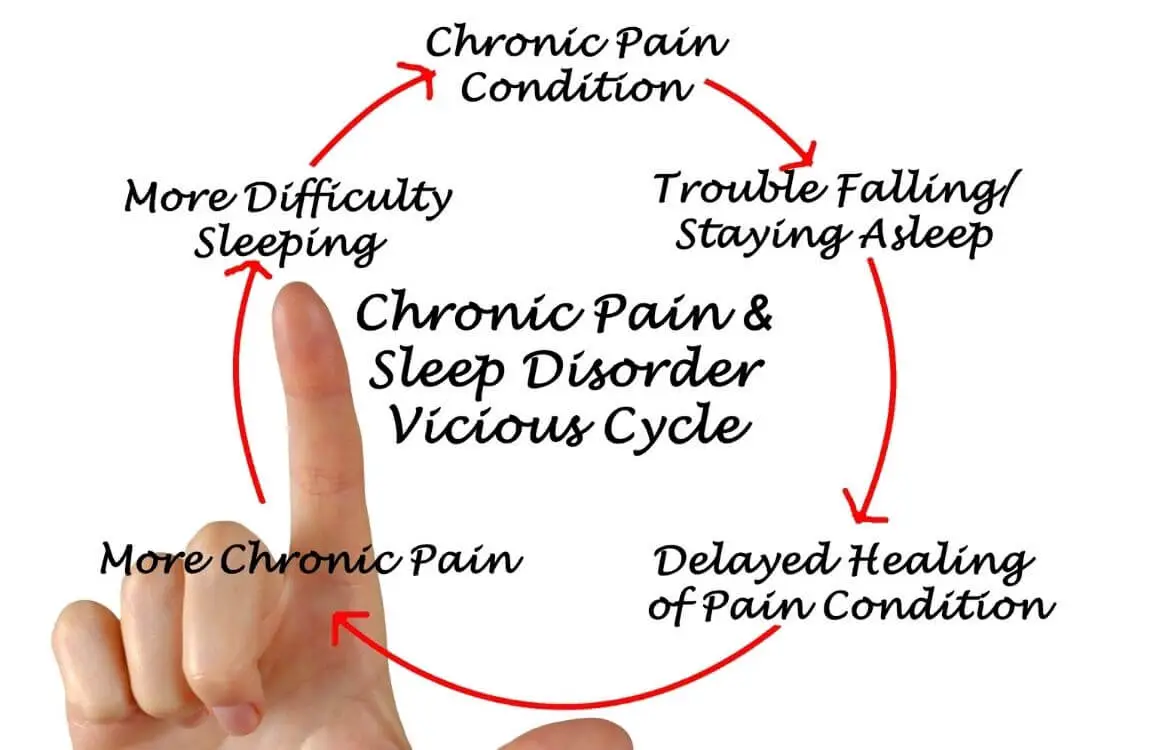
In the case of chronic pain, stress worsens its condition.
Pain is a physical stressor, and so it will always activate the sympathetic system. That sympathetic nervous system will cause different changes in your body, which can turn around and cause you to feel more pain. So, pain can feed off itself.
Even in the case of acute pain, the more you focus on your cut, headache, a broken bone, the more pain you’re going to feel!
As you can see, pain is more than just a physical experience, it is also an emotional one.
Chronic pain can cause you anxiety, it caused anxiety to my wife every time she experienced pain, because she began to worry about it in the future, and about the things she wouldn’t be able to do anymore, like dancing.
That anxiety is an emotional stressor. M also felt anger, sadness, guilt, therefore pain created plenty of emotional stressors. All that multiplied stress changed into more pain.
But this is just one aspect of pain – your own stressors. Let’s not forget about other stressors – your life, work, family, friends, finances, hobbies, etc… It all adds up causing poorer diet, lack of sleep, relationship issues.
This vicious cycle is very common. I’m sure your partner or yourself experienced that. Pain can easily get out of control!
You cannot get rid of chronic pain with medication or any other acute pain treatment, because chronic pain doesn’t have a cure. You have to learn how to break this vicious cycle.
How to break the pain-stressors cycle?
One of the ways of breaking such a cycle is relaxation training, and that includes breathing exercises.
The first thing you have to make sure of is that you breathe deeply. A lot of times we get exposed to stress which makes us breathe very fast and shallow, or we hold our breath altogether. My wife experienced that a lot during her panic attacks.
When your brain notices that you hold your breath, it will brace itself for more stress, more pain…
So, you have to learn to do more deep breathing – deep diaphragmatic breathing.
Our lungs are like balloons. When we breathe fast and shallow, we only use the top of our lungs. If we stop breathing altogether by holding our breath, the lungs don’t take oxygen at all.
When we breathe deeply, our entire lungs start to expand. When we breathe deeply, lungs press from above towards our belly, which begins to expand. This is actually a natural way of breathing. You should not breathe through your diaphragm.
What you need to do is to try and bring the natural, belly-breathing pattern.
You need to learn to breathe slow, not rapidly. Begin with trying to inhale naturally, but exhale 5 seconds longer, and that, without holding your breath. There may occur a pause before inhaling, but it should be natural, not forced.
Important is that you use your mind to control your breathing, don’t just breathe and go. This exercise is about focusing on your breathing because it allows your nervous system to calm down, therefore, lowering the pain that is experienced.
Why do these breathing exercises work?
They work on two levels – by activating the parasympathetic system, which helps your body get back to its natural calm state, and by distracting you from pain.
It is not just a psychological trigger that lowers your pain, breathing actually creates physiological changes in your body. Your heart rate slows down, blood vessels expand, any stress hormones stop being released to the body.
The element of distraction that breathing creates works as follows…
Your mind can actually pay attention to so many things at once. You focus on relaxing your body not the pain. It’s like falling asleep in pain (which often happens to my wife), when you wake up, the pain is gone.
The role of cognition!
How to break the cycle another way?
Our thought processes (cognitive processes) guide everything that we do…
We have situations in life, but each one of us interprets them in a different way. That leads to different reactions – behavior, physical, emotional.
The way we interpret situations plays a big role in how we feel, therefore, how it impacts chronic pain.
Sometimes our interpretations are automatic, we don’t stop and think about it, interpretations just happen.
Our thoughts are rooted in our perception of ourselves, and our role in the world, which is usually shaped in our childhood and early experiences.
M sometimes wakes up with pain. Naturally, she thinks that it happened again and this will never end, that her day is ruined, life is terrible, she’s depressed. These are the patterns of thoughts of my wife but you may relate to that.
Naturally, M experiences stress, anxiety over the unknown, sadness, but she may also snap at me, get angry easier than usual. All that activates the automatic nervous system.
These stress responses that kick in are the cause of pain, and the cycle continues…
You have to break the cycle by restructuring your cognition. But it’s not that simple. You cannot just change something negative into positive!
What is important that you must notice, is that anxiety creates exaggerated thoughts.
These extra thoughts aren’t helpful, and so in order to break this pattern, we have to target these thoughts.
I often remind my wife of simple facts:
- She doesn’t know the future, no one does.
- She can’t do anything about it today.
- Yes, life difficult, we have ups and downs in life.
- She’s safe, she’s with me, she’s not alone.
- No matter what happens, I’m here.
So, you need to modify anxious thoughts by revealing facts, not imaginary thoughts for which there is no evidence because they never even happened yet.
I often remind my wife that however terrible she feels in that moment, the pain flare-up will pass, anxiety will pass, nothing lasts, the day is not set.
That always lowers her anxiety, anger, sadness, because she knows the facts. Additionally, she knows that I’m by her side and I will not abandon her.
The way we perceive the world and situations shape our behavior. Remember, our thoughts are automatic.
So, in order to make some changes, you need to train your mind by repetition, you do this by repeatedly breaking the cycle of pain-stress and stress-pain.
You must remember that changes take time, you will not wake up the next morning and it will all be gone. Chronic illness doesn’t have a cure, chronic pain doesn’t have a cure. You must learn to live with it by targeting the areas of your life which are impacted by pain.
Again, it may be your partner, a family member, financial impact, work, social life, or else. You must take care of that, and your perception of the situations trigger your stress or pain.
These exercises target not only pain but are also effective against anxiety and depression.
Cognitive-Behavioural Therapy, commonly known as CBT, is the key to improving your quality of life with chronic pain.
But sometimes you may find that you have to wait in a cue for your therapy, or pay for it, which is often costly since you need to repeat your sessions in order to reach the desired effect.
My wife waited for her CBT for 9 months!
It wasn’t only torture for her, I couldn’t stand watching her struggle, not being able to help. I supported M throughout these months by learning the craft from various books. I became more aware of how she felt, I listened and talked.
I listed these books below because they helped me and my wife understand the whole process before she even got CBT sessions.
These books are very helpful in helping you understand your anxiety and helping you get out of the cycle.
You may access these books by clicking either on the links above or the book covers below…
My wife has read this book in a jiffy! It helped her during her dark times to find compassion and love for herself. For somebody like M, who suffered from severe depression, I noticed that the harshest critic of her was herself. It is never helpful to be told to pull ourselves together by others but saying it to ourselves leads us in only one direction – into a terrible despair.
I listed this book because M also suffered from anxiety at that time, it helped her mindset and depression. An obsessing, ruminating, and dwelling on things may or may not happen, but this book makes it simple to understand, how to manage your fear. Your brain is a very powerful tool, and the more you work to change your mindset, the better you’re going to feel.
This is another book that my wife reached for during her depression because it offered my wife a self-help program, written by one of the leading authorities in CBT. M also suffered at the time with OCD. A whole range of anxieties and fears are explained, from panic attacks and phobias to obsessive-compulsive disorder and anxiety. That really helped her!
A whole range of anxieties and fears are explained, from panic attacks and phobias to obsessive-compulsive disorder (OCD) and generalized anxiety. That really helped us!
Time passed, and the therapy was amazing. It helped my wife, however, it was targeted towards panic attacks which she suffered from at the time. Six months after, M had another therapy targeting general anxiety in relation to chronic pain.
Her second CBT was with a chronic illness specialist.
This therapist suffered from chronic pain herself and understood my wife better than anyone ever could. Additionally, my wife had a 3rd therapy, focusing on her OCD.
Anxiety takes many forms, it stays with you for life. The trick is about learning to live with it, and how to control your emotions.
Sometimes I was asked by my wife’s therapists to accompany her in her sessions. Additionally, I attended her mental health support group sessions and her monthly endometriosis support group meetings.
I’ve learned A LOT!
I wish you all good luck, all the very best, and I do hope that you have found the “acute vs chronic pain” article helpful. If so, please share to help others.
Cheerio!
The article “acute vs chronic pain” is based on our personal experience but also on education from various sources such as Stanford Healthcare.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…