Endometriosis and severe anemia: when food and supplements aren’t enough!
About endometriosis and severe anemia…
What can you do when endometriosis and severe anemia take over your life and every first-line treatment you tried isn’t working?
Iron deficiency anemia is typically treated with a diet rich in iron or iron pill supplements.
When the first-line approach doesn’t work and you develop severe anemia, you may be offered an iron infusion instead.
You may require an infusion if you:
- can’t take iron by mouth
- can’t absorb it through your gut
- can’t absorb enough iron due to blood loss
- need to increase it fast to avoid complications
Iron infusion is simply a procedure in which iron is delivered to your body by inserting a needle into your vein.
It looks like a typical drip and is also known as an intravenous (IV) infusion.
Does it sound like you?
Endometriosis causes you to feel crap and fatigued all the time. It’s not the constant pain or stress because you’ve learned to deal with them. But something still isn’t quite right…
You wake up tired. You’re not as focused and sharp as usual, you may even experience some dizzy spells.
Time goes by, and you think it’s temporary, maybe you have the flu, maybe it’s your sugar level is low, and you have to bite something…
Wait a minute, it didn’t work!
You check your period diary but you haven’t bled more than usual.
Eventually, you find that it affects your fitness, work, money, family, social life, and the list goes on…
You eat a well-balanced iron-rich diet with vitamin C for better absorption, and you tried iron pills and other supplements but all the above make you sick and constipated.
A doctor prescribes you Omeprazole for acid reflux, you get temporary relief. But your IBS gives you constipation.
Fart that! It’s constant, it’s tiring as if you weren’t tired enough!
You go to the doctor again and he blames it on stress and your periods that are “meant to hurt”!
Many women are treated for depression before they are found to have iron deficiency or severe anemia.
But iron is important for keeping you healthy. It gives you energy and helps you concentrate.
Low iron can put you at risk of brain fog, which is commonly associated with fibromyalgia, but also anxiety and inability to cope.
As a woman, there will be times when you are more at risk of not having enough iron. It could be due to endometriosis and severe anemia, or even heavy periods.
Additionally, during pregnancy and after giving birth. So, whatever part of your life, as a woman, you will need more iron.
Despite all the facts, doctors offer you antidepressants (really??)…
Luckily, you know better! You seek a second, even third opinion.
But as the story goes, history repeats itself.
Because doctors don’t really take notes, do they, and they don’t pass your history to another. So you start from scratch each time.
They don’t look at you as a person, you’re just a number in the health care system being treated the same as everyone else.
Because you’re not unique, you’re not an individual. You’re just a number in the system.
You realize that endometriosis and severe anemia drag you down for 6 years now… Your constant anxiety about the future caused you to feel depressed and suicidal…
Welcome to my wife’s life!
Before you read the post, if you are interested in finding more details about endometriosis, I wrote an “Endo-Tool, Endometriosis for Men” e-Book, where you get a FREE 1st chapter containing 20 pages filled with a lot of value, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
Get FREE “Endo-Tool”
Endometriosis for Men e-Book

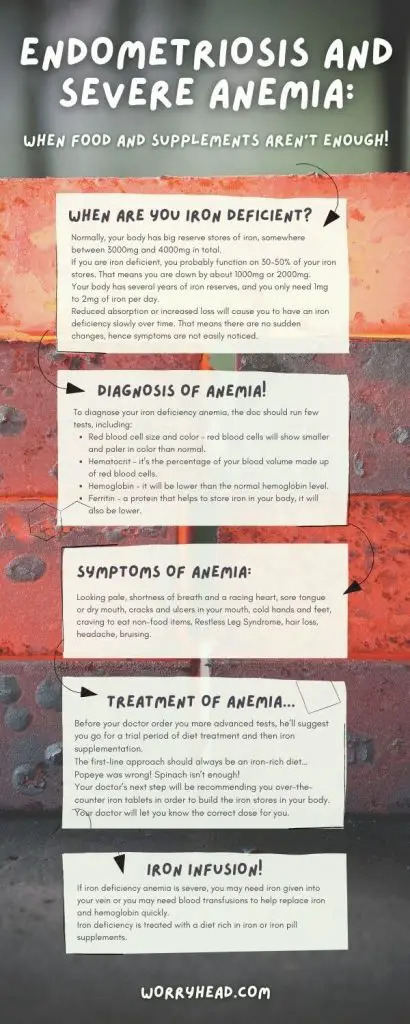
When are you iron deficient?
Normally, your body has big reserve stores of iron, somewhere between 3000mg and 4000mg in total.
If you are iron deficient, you probably function on 30-50% of your iron stores. That means you are down by about 1000mg or 2000mg.
Your body has several years of iron reserves, and you only need 1mg to 2mg of iron per day.
Reduced absorption or increased loss will cause you to have an iron deficiency slowly over time. That means there are no sudden changes, hence symptoms are not easily noticed.
Usually:
- Normal iron levels are +4000mg
- Normal Absorption is +2000mg
- Normal losses are -1000mg
During menstruation:
- Losses from normal periods are -250mg
- Losses from Heavy periods are -500mg
- Pregnancy is -1400mg
- Blood loss usually is -500mg to -1litre
Iron deficiency happens before you become anemic because, in order to become anemic, your body is so low on iron that it cannot perform the most vital function, which is making red blood cells.
By the time you have anemia, your body is empty of iron. You need to replace the loss with a minimum of 1000mg.
A bit of research…
If you’re reading this you probably already know a little bit about endometriosis or if you’re the one who supports your loved one, you seek information on how to help her.
Luckily for you, I put together this rather lengthy guide because my dear wife suffers from endometriosis and severe anemia herself.
Apart from stage IV deep infiltrating endometriosis, she sufferers from fibromyalgia.
I mentioned fibromyalgia here because this syndrome is usually caused by physical trauma and would be worth you looking into that.
The diagnosis of endometriosis and severe anemia was traumatic enough to cause my wife to develop fibromyalgia.
In regards to iron and endometriosis, there was a study done in 2002.
It stated that “the iron concentrations in the peritoneal fluid of the pelvic cavity of women with endometriosis were higher than of women without”.
Additionally, they noticed that these high concentrations of iron remain throughout each stage of endometriosis.
They were also found alongside the lesions.
Then there was another study in 2006. It proved that iron deposits and its overload were found within the pelvic cavity where endometriosis occurs and that it may contribute to the spread of the disease.
The study showed that “iron may contribute to the growth of the disease and the use of an iron chelator may be beneficial to help control iron levels in women with endometriosis.”
An iron chelator is a therapy that removes excess iron from your body with special drugs.
In 2008 there was another study was published.
This time it reviewed the potential consequences of iron overload in women with endometriosis.
The study showed that women with endo are unable to stabilize the amounts of iron in their bodies as easily as women who do not suffer from it.
The excess iron levels may contribute to inflammation or even aggravate the symptoms of your endometriosis.
Diagnosis of anemia!
To diagnose your iron deficiency anemia, the doc should run a few tests, including:
- Red blood cell size and color – red blood cells will show smaller and paler in color than normal.
- Hematocrit – it’s the percentage of your blood volume made up of red blood cells.
- Hemoglobin – it will be lower than the normal hemoglobin level.
- Ferritin – a protein that helps to store iron in your body, it will also be lower.
In some cases, your doctor may order additional tests to identify an underlying cause, because any diseases or other disorders may be the cause of anemia.
These tests are:
Endoscopy – to check for bleeding from a hernia, an ulcer, or your stomach.
They will insert a thin, lighted tube equipped with a video camera down your throat to your stomach.
This allows them to view the tube that runs from your mouth to your tummy and look for sources of bleeding.
Colonoscopy – to rule out the same sources of bleeding but in the lower intestine.
They will insert a thin, flexible tube, also equipped with a video camera into your rectum and guide it to your colon.
But don’t worry, you’re usually sedated during this test.
A colonoscopy allows them to view inside some or all of your colon and rectum to look for internal bleeding.
Ultrasound – women will also have a pelvic ultrasound done to look for the cause of excessive menstrual bleeding, including fibroids.
Symptoms of anemia.
Looking pale.
Hemoglobin is a red-colored pigment since you are iron deficient, there will be less hemoglobin in your blood which may make you look pale.
You will notice this mostly on your face, nails, inner mouth, and the lining of your eyes.
If you pull your lower eyelid down, the color of it will be pale, normally it should be a rich, red color.
If it’s very pale or yellow, this may indicate an iron deficiency or severe anemia.
Shortness of breath and a racing heart.
During exercise, you usually experience some shortness of breath and a racing heart because there is an increased demand for oxygen in your body.
However, if you are iron deficient or anemic, your blood will not contain enough oxygen for your muscles to do everyday activities such as walking.
Your legs are your biggest muscles and so they need the most oxygen to function when you walk.
Your body tries to make up for this by increasing your breathing rate to get more oxygen.
Increasing your heart rate it helps to move the oxygen around your body.
Sore tongue or dry mouth.
Believe it or not, iron deficiency can affect your tongue making it feel sore for no apparent reason.
Additionally, you may have a dry mouth even if you have been drinking plenty of water.
Cracks and ulcers in your mouth.
Iron deficiency can also cause you to have sore, red, and flaky cracks in your mouth.
Mouth ulcers are simply sore and white patches on the inside of your mouth.
There are many reasons why you might have them. Stress and being run down are usually the cause, but another reason could be iron deficiency.
Cold hands and feet.
If you feel easily cold or you often have cold hands or feet even when it’s warm, it may be because there is not enough oxygen being delivered to your hands and feet.
This is often a result of iron deficiency.
Craving to eat non-food items.
Craving certain foods from time to time is normal, however, if you have cravings to eat ice or even clay, dirt, or ash, this could be a sign of iron deficiency.
This is also called “Pica Disorder”.
Restless Leg Syndrome.
Restless Leg Syndrome is a need to move your legs when resting, especially if you are in bed or sitting.
This distressing feeling often goes away when you move your legs.
It is possible to have it but not be iron deficient, but if you are iron deficient you are nine times more likely to experience this syndrome.
Hair loss.
Bummer! No one likes that, however, It’s normal for some hair to fall out when you wash or comb it, but if you are losing clumps of hair, it could be caused by iron deficiency.
Headache.
Doesn’t seem obvious because headaches can occur for many reasons.
Repeated headaches though, could be a sign of iron deficiency.
Dizziness, irritability, and loss of concentration.
People can take this wrongly and accuse you of mental health problems, but feeling irritable, dizzy, or losing concentration quickly could be due to iron deficiency.
Iron helps your blood deliver oxygen in your body and feeling irritable or dizzy may be a sign of your brain not getting enough oxygen.
Bruising.
In anemia, the bone marrow is “starved of iron”.
Not being able to make enough red blood cells (anemia), there can also be a reduction in platelet production.
Platelets are the first step in your blood clotting, so a reduction in platelets leads to bruising.
First-line treatment.
Since we discuss endometriosis and severe anemia it’s worth explaining the basics for those who don’t suffer from this condition.
Simply put, endometriosis is characterized by the growth of endometrial tissue outside the uterus.
It affects roughly 200 million women worldwide between the ages of 15 and 55 years old.
Women with endometriosis experience severe pelvic and abdominal pain, but also infertility, and heavy or irregular bleeding.
Over time, heavy periods may result in the depletion of iron stores.
After my wife’s 4 years of ferritin deficiency, M developed anemia. For the following 2 years, she battled with doctors over having an iron infusion.
Only 6 years after her first serious fatigue they agreed to it.
Before that happened, my wife (like most women) went through a series of tests, trials, and errors.
Yes, endometriosis and severe anemia take over your life hell, but you are still expected to do baby steps towards recovery.
Doctors tell you to go through the first-line treatment despite your deterioration.
They begin with your doctor may ask you a number of questions, such as:
- When did you begin experiencing symptoms?
- How severe are they?
- Does anything improve them?
- What makes them worsen?
- Have you noticed unusual bleeding, such as heavy periods, hemorrhoids, or nosebleeds?
- Have you recently donated blood more than once?
- Are you a vegetarian?
It’s best to be ready to answer them quickly to save the time doctors don’t have. After all, you want to spend more time on solving the issue.
So what you can do is write down any symptoms that you experience, plus any major stresses or recent life changes if they occurred.
Make a list of all medications, vitamins, or supplements that you’re taking. Get prepared!
If you have any, write down your own questions to ask your doctor.
Your time with doctors is limited, so preparing a list of questions will help you make the most of your time together.
For instance, here are some basic questions to ask him about iron-deficiency anemia:
- Your question number one should be – I have endometriosis, could that be the issue?
- Apart from my condition, what’s the most likely cause of my symptoms?
- Are there other possible causes for them?
- Is it temporary or long-lasting?
- What treatment do you recommend?
- Are there any alternatives to the first-line
approach? - Are there any dietary restrictions that I need to follow?
But what’s next, how will you be diagnosed to confirm your invisible struggle?
Treatment of anemia…
Before your doctor order you more advanced tests, he’ll suggest you go for a trial period of diet treatment and then iron supplementation.
The first-line approach should always be an iron-rich diet…
Popeye was wrong! Spinach isn’t enough!
Choose iron-rich foods that are rich in iron:
- Red meat, pork, and poultry.
- Seafood.
- Beans, peas.
- Dark green leafy vegetables, like spinach.
- Dried fruit, such as raisins and apricots.
- Iron-fortified cereals, bread, and pasta.
Your body absorbs more iron from red meat. If you choose not to eat meat, or you cannot digest it, you may eat iron-rich, plant-based foods.
Choose foods that contain vitamin C, because it enhances your iron absorption. You can do it by drinking citrus juice or eating other foods rich in vitamin C at the same time as when you eat high-iron foods.
Vitamin C is also found in:
- Broccoli
- Grapefruit
- Kiwi
- Leafy greens
- Melons
- Oranges
- Peppers
- Strawberries
- Tangerines
- Tomatoes
All nice and dandy, but as it turns out, you may be in the same position as my wife – you cannot eat meat, dairy, and things like acidic fruits and juices. Your stomach simply cannot handle it.
What your doctor will offer you is Omeprazole or similar anti-acid pills. But they only make things worse, lower the absorption of iron that you struggle to take in as it is.
Additionally, you find out that you cannot have either calcium or caffeine during eating your meals containing iron.
They lower the absorption too. You can still have tea or coffee but you need to drink them 2 hours before or after your food.
What can you do next knowing that despite your best efforts and the dietary approach you feel crap and it doesn’t seem to work?
Severe anemia!
Your doctor’s next step will be recommending you over-the-counter iron tablets in order to build the iron stores in your body.
Your doctor will let you know the correct dose for you.
To improve the chances of iron absorption from the tablets, you may be instructed to take iron tablets on an empty stomach. However, quite often they will upset your stomach, and you may need to take your iron tablets with meals.
Don’t take iron with antacids like Omeprazole because they interfere with your absorption of iron. Take iron two hours before or four hours after you take antacids.
Take them with vitamin C to improve their absorption.
However, taking iron supplements can cause constipation and acid reflux.
It isn’t easy, so far nothing worked and your food and supplements aren’t enough!
Endometriosis and severe anemia don’t go away. There is no cure for endometriosis but surely, there must be some kind of solution to anemia.
But is there?
There may be some underlying cause of the iron deficiency.
Even if you could digest your iron supplements but still, they don’t increase your blood-iron levels, it’s likely that anemia is due to something else…
Your doctor will need to investigate and treat the source of any bleeding or an iron-absorption problem.
Depending on the cause, treatment of anemia may involve:
- Medications, such as oral contraceptives to lighten your periods.
- Antibiotics and other medications to treat peptic ulcers.
- Surgery, to remove a bleeding polyp, a tumor, a fibroid, or endometriosis.
Phew… you’ve done your best, I mean, really best and you feel like you cannot go on like this any longer.
So far everything failed and you feel like you wasted precious years battling doctors, diets, physical and emotional problems.
Is that really it?
Iron infusion for severe anemia!
If iron deficiency anemia is severe, you may need iron given intravenously or you may need blood transfusions to help replace iron and hemoglobin quickly.
But let’s not jump to blood transfusions, iron infusion really works. However, there are perks and side effects worth looking at first.
As we said already, iron deficiency is treated with a diet rich in iron or iron pill supplements.
Sometimes, however, the first-line approach doesn’t work and you develop severe anemia, you may be offered an iron infusion instead which simply is a procedure in which iron is delivered to your body by inserting a needle into your vein.
It is important for you to know that you will have to prepare yourself for an iron infusion.
Your doctor will give you specific instructions so you don’t have to worry about that. But there are some basic things you can do to prepare yourself for it, including:
- Eat your breakfast and lunch, as there is no need to fast for an iron infusion.
- Take regular medications that you usually take.
- Be prepared to have a small i.v. drip put in your arm or hand.
You will probably feel nervous about your iron infusion.
You can help reduce any anxieties by talking about the procedure with your doctor first. They can recommend ways to help you stay comfortable and relaxed during the infusion.
Here we have some tips for your comfort:
- Wear comfy, loose-fitting clothes.
- Have a bottle of water with you.
- Listen to music or watch something on a tablet or smartphone.
- You can always read a book or magazine.
The procedure…
You will probably want to know what happens during the iron infusion?
Let’s do just that!
An iron infusion takes place in the hospital or hemodialysis centers. Most likely you will have it at the hospital.
A doctor, a nurse will use a needle to insert a small tube into a vein. This small tube is known as a catheter.
A doctor or nurse will put the needle-catheter into the vein of your arm or hand (I recommend the arm as it’s more comfortable), after which will remove the needle, leaving only the catheter in your vein.
The catheter will be attached to a long tube, which is connected to an IV bag filled with the iron liquid.
The iron has been diluted with a saline solution which is either slowly pumped into your vein or simply hanging, using gravity to slowly drip down the tube and into your vein.
You may feel a slight pinch in your skin where the IV needle is inserted. Don’t we all..?!
Some people may also feel some pressure at the insertion site during the procedure but this is nothing to worry about, it’s normal.
The doctor or nurse performing the procedure will give you a test dose first to ensure you don’t have any adverse reactions from the iron. Yay! No need to worry anymore… If you have some reaction, they will simply stop the procedure.
How long does an iron infusion take?
An iron infusion can take roughly 30 minutes and you will be expected to be seated.
In some cases, the infusion can take a little longer but the good thing is that a slow infusion rate helps prevent complications.
It often takes several iron infusions to bring your iron to the appropriate levels.
You will receive iron infusions over the course of one or a few weeks for your treatments. Iron infusions take time and can be more expensive than other types of anemia treatments.
Luckily for some (my wife), there are free treatments on the NHS (United Kingdom).
Pros and cons!
Iron infusion benefits:
An iron infusion is a way to increase your body’s iron levels quickly. It’s much faster than supplements or dietary changes. It’s especially helpful in situations where anemia is severe.
The main physical benefits of an iron infusion are increased energy and easier breathing.
You can expect to start feeling these benefits a few weeks after your final infusion.
How long will they last?
It depends on the cause of your anemia and whether you’re using other therapies to increase your iron levels.
A regular blood loss during menstruation may lead to a chronic drop in iron levels. This is where endometriosis and severe anemia are connected.
Depending on your situation, the benefits of an iron infusion will last anywhere from several months to a few years.
If you continue with your iron-rich diet, you will definitely prolong the benefits!
Side effects and complications:
After your infusion, you can return to your normal activities straight away.
You should feel good enough because most people are even able to drive themselves home. You can even go back to work after if you feel up to it.
So far so good? Well…
You may have some side effects right after the procedure. Most of them are mild so you don’t need to worry.
These include:
- Temporary changes in the way you taste food and drinks.
- Headaches, therefore nausea and vomiting.
- Muscle and joint pain.
- Shortness of breath, mild and not life-threatening.
- Itchiness and rash.
Increased or decreased blood pressure or heart rate – mild. - Burning sensation at the site of the injection – common.
In rare cases, there might be serious side effects.
Again, they are rare but the most common complication would be iron toxicity.
The symptoms of iron toxicity may come on quickly, which can cause anaphylactic shock, however, you will be at the hospital, in the right place, and at the right time, so that’s settled.
When it comes to toxicity appearing slowly, it will develop over time, leading to too much iron in the body’s tissues.
The test dose and the slow infusion rate are both done to prevent these complications. This is why you sit in the chair for 30 minutes. The slower it goes, the safer it is!
The test dose is also important if you have a history of multiple drug allergies. But if you don’t, you should be fine.
Your doctor will use the test dose to monitor you for any reactions, so put your worries aside.
Your test will be your best friend!
The facts about side effects!
Anaphylaxis (shock) used to happen with the older iron dextrans and it used to be in the 1960s and 1970s.
These products are no longer used and you don’t have to worry about them.
Despite these facts, there is still a lot of fear of confusing everyone, both- doctors and patients.
With new preparations reactions are rare, but as with any treatment, there are:
Anxiety.
Anxiety is extremely common.
As I write this post, my wife experiences anxiety because she’s about to get her first iron infusion in a week’s time!
People with iron deficiency are anxious. This is a normal symptom of iron deficiency.
You have to take time to ensure that you are relaxed, well-hydrated, in a calm environment.
Flushing.
That’s pretty common 5 to 10 percent of people will have a flushing reaction. This is not an allergy!
As the iron enters your body a very small amount of free iron will cause flushing, nausea, or headache.
Remember, this is NOT an allergy so don’t worry about it.
Hypersensitivity.
This happens to about 1% of people. Your symptoms will be similar to flushing but can develop a rash and cough.
You’ll simply stop the infusion, be reassured with a single steroid injection (hydrocortisone).
Then after 5 or 10 minutes you will slowly restart and complete the infusion.
Allergies…
A true allergy happens to 1 in 10,000 people. An anaphylactic shock will usually respond to steroids and if that somehow doesn’t work, you will be given adrenaline.
Either way, you’ll be in a safe place, surrounded by professionals, so there is no need to worry.
Post infusion flu.
You should probably expect that. This is pretty common. Some aches and pains, maybe temperature and flu-like symptoms might develop the next day and last for 48 hours.
It’s so common that it’s regarded as normal.
Takeaways…
When food and supplements aren’t enough and endometriosis and severe anemia cause you to feel like a zombie, it’s worth visiting your doctor to seek help.
By the time you get the appointment, it’s best to prepare yourself for the visit.
Remember that doctors usually have 10-15 minutes to assess you. Write down your questions and worries. Be ready, it will speed up the process of diagnosis.
Remember what you’ve learned so far.
You may expect anemia yourself if you feel constantly the following symptoms:
- Shortness of breath while exerting.
- Fatigue, weakness, dizziness.
- An urge to eat ice (severe anemia).
- Headaches.
- Depression.
- Temperature sensitivity.
- A sore tongue.
- Restless Leg Syndrome.
- Poor muscle coordination.
Knowing that most of the above symptoms never go away, go to your doc and have a chat.
He’ll ask you a bunch of questions and order some blood tests.
Confirming the results, he’ll tell you about the iron-rich diet and iron supplementation in the form of pills or liquid.
When now of the first-line treatments work, you’ll be offered an iron infusion. If this doesn’t work – a blood transfusion.
I hope you found this post helpful.
Share your thoughts!
Tell us what you think, maybe you have a story to tell? Write to us HERE.
Take good care of yourself!


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…