
Fibromyalgia Basics
All You Need to Know
Some days, I watch my wife carry an ache the world can’t see, and I remember why this fibromyalgia basics page exists. If fibromyalgia has been stealing your sleep, your plans, or your sense of self, you’re not alone.
I’m Lucjan, a husband who had to learn the language of invisible pain: pacing, flare days, brain fog, gentleness. Fibromyalgia Basics is a calm starting point – for women living with fibro and for partners who want to show up better. You’ll find plain-English explanations, practical support for fatigue and pain, and partner-aware ideas you can use tonight.
This is the main guide to fibromyalgia, filled with all of the essentials in one place. It also links to deeper articles on symptoms, assessment and diagnosis, pain science, sleep and fatigue, gentle movement, pacing and flare planning, mental health, intimacy and relationships, work/education, comorbidities (like CFS, IBS, endometriosis, migraines, or temporomandibular joint disorder), nutrition basics, and everyday coping, so you can dive into the details when you’re ready…
While I aim for accuracy and reference reputable sources, this is not medical advice! It’s a safe place to breathe, learn, and feel seen, written from a partner’s perspective, especially a man who loves someone living with fibro.
- Fibromyalgia Basics
- Definition of Fibromyalgia
- Prevalence of Fibromyalgia
- Symptoms of Fibromyalgia
- Causes & Theories for Fibromyalgia
- Diagnosis of Fibromyalgia
- Treatment of Fibromyalgia
- Impact of Fibromyalgia
- Comorbidities of Fibromyalgia
- Flares & Triggers for Fibromyalgia
- Lifestyle & Self-Management of Fibromyalgia
- Awareness & Advocacy for Fibromyalgia
- Research & Future of Fibromyalgia
- Fibromyalgia Infographic
- My Wife's Fibromyalgia
- My Fibromyalgia eBook
Fibromyalgia Basics
Fibromyalgia isn’t just “aches everywhere”. It’s a nervous system that keeps the volume turned up, even on quiet days. In this guide, we start with a clear definition, then ask: how prevalent is fibro really, and why are so many stories still hidden? We’ll map symptoms beyond pain, fatigue, sleep issues, fibro fog, sensitivities, and explore why they ebb and flow.
What’s happening under the hood, like causes & theories like central sensitization, neurotransmitters, genetics, and the triggers that flip the switch.
When tests come back “normal”, how is fibro diagnosed, and what do the Widespread Pain Index and Symptom Severity Scale actually measure? Which treatments help most – medications, CBT, gentle movement, physio, and how do you combine them without burning out? We’ll talk impact too, like work, school, relationships, intimacy, and mental health no one sees.
Which comorbidities often travel with fibro (IBS, migraines, TMJ, POTS, endometriosis), and why does that matter for care? What sparks flares: weather, stress, hormones, overdoing it, and how do you build a plan before the crash? What lifestyle & self-management shifts are worth the limited energy: pacing, sleep hygiene, anti-inflammatory nutrition, support groups?
Finally, we’ll explore how can awareness & advocacy move the needle today, and what research is coming that might change tomorrow?
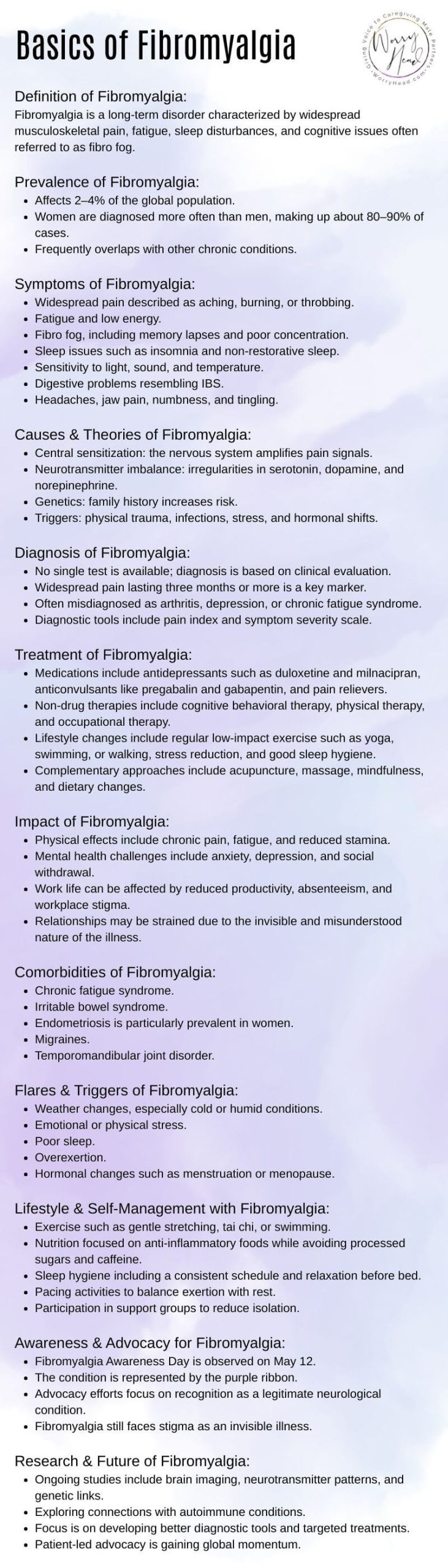
Definition of Fibromyalgia:
Fibromyalgia is a long-term disorder characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive issues often referred to as fibro fog.
Prevalence of Fibromyalgia:
- Affects 2–4% of the global population.
- Women are diagnosed more often than men, making up about 80–90% of cases.
- Frequently overlaps with other chronic conditions.
Symptoms of Fibromyalgia:
- Widespread pain is described as aching, burning, or throbbing.
- Fatigue and low energy.
- Fibro fog, including memory lapses and poor concentration.
- Sleep issues such as insomnia and non-restorative sleep.
- Sensitivity to light, sound, and temperature.
- Digestive problems resembling IBS.
- Headaches, jaw pain, numbness, and tingling.
Causes & Theories for Fibromyalgia:
- Central sensitization: the nervous system amplifies pain signals.
- Neurotransmitter imbalance: irregularities in serotonin, dopamine, and norepinephrine.
- Genetics: family history increases risk.
- Triggers: physical trauma, infections, stress, and hormonal shifts.
Diagnosis of Fibromyalgia:
- No single test is available; diagnosis is based on clinical evaluation.
- Widespread pain lasting three months or more is a key marker.
- Often misdiagnosed as arthritis, depression, or chronic fatigue syndrome.
- Diagnostic tools include the pain index and symptom severity scale.
Treatment of Fibromyalgia:
- Medications include antidepressants such as duloxetine and milnacipran, anticonvulsants like pregabalin and gabapentin, and pain relievers.
- Non-drug therapies include cognitive behavioral therapy, physical therapy, and occupational therapy.
- Lifestyle changes include regular low-impact exercise such as yoga, swimming, or walking, stress reduction, and good sleep hygiene.
- Complementary approaches include acupuncture, massage, mindfulness, and dietary changes.
Impact of Fibromyalgia:
- Physical effects include chronic pain, fatigue, and reduced stamina.
- Mental health challenges include anxiety, depression, and social withdrawal.
- Work life can be affected by reduced productivity, absenteeism, and workplace stigma.
- Relationships may be strained due to the invisible and misunderstood nature of the illness.
Comorbidities of Fibromyalgia:
- Chronic fatigue syndrome.
- Irritable bowel syndrome.
- Endometriosis is particularly prevalent in women.
- Migraines.
- Temporomandibular joint disorder.
Flares & Triggers for Fibromyalgia:
- Weather changes, especially cold or humid conditions.
- Emotional or physical stress.
- Poor sleep.
- Overexertion.
- Hormonal changes such as menstruation or menopause.
Lifestyle & Self-Management of Fibromyalgia:
- Exercise such as gentle stretching, tai chi, or swimming.
- Nutrition focused on anti-inflammatory foods while avoiding processed sugars and caffeine.
- Sleep hygiene including a consistent schedule and relaxation before bed.
- Pacing activities to balance exertion with rest.
- Participation in support groups to reduce isolation.
Awareness & Advocacy for Fibromyalgia:
- Fibromyalgia Awareness Day is observed on May 12.
- The condition is represented by the purple ribbon.
- Advocacy efforts focus on recognition as a legitimate neurological condition.
- Fibromyalgia still faces stigma as an invisible illness.
Research & Future of Fibromyalgia:
- Ongoing studies include brain imaging, neurotransmitter patterns, and genetic links.
- Exploring connections with autoimmune conditions.
- Focus is on developing better diagnostic tools and targeted treatments.
- Patient-led advocacy is gaining global momentum.
If someone you love is living with fibromyalgia, I have a gift for you: 3 FREE chapters of “Fibromyalgia for Caring Partners” eBook, a guide I wrote as a husband learning how to show up with gentleness, clarity, and courage. Inside, you’ll find simple scripts for tough appointments, pacing tips for flare days, and small acts that make a big difference.
When you subscribe, I’ll send personal emails with extra checklists, planning templates, and stories we don’t post publicly, plus printable freebies and subscriber-only discounts across my books. No fluff, no spam, just steady, practical support you can use tonight.
These 3 chapters alone explain how to accept the new normal, and understand fibromyalgia, and its diagnosis. They include:
- The new you.
- The new her.
- The new reality.
- Introduction to fibromyalgia.
- What is fibromyalgia?
- The early days.
- When you first realise something is wrong.
- Spotting the signs that something is wrong.
- Coming to terms with a chronic illness.
- The role of partner in fibromyalgia.
- The process of getting diagnosed.
Get Your 3 FREE Chapters!
Fibromyalgia for Caring Men
Definition of Fibromyalgia
Fibromyalgia is a long-term disorder marked by widespread musculoskeletal pain, deep fatigue, unrefreshing sleep, and cognitive difficulties often called “fibro fog.” The condition involves altered processing of pain and sensory signals in the nervous system, so aches and stimuli can feel amplified and persistent. People may notice tenderness at multiple sites, sensitivity to touch, sound, light, or temperature, and a pattern where poor sleep worsens pain and fog. Fibromyalgia is real and common, affecting daily function, mood, and relationships—and it deserves compassionate, evidence-informed care.
Prevalence of Fibromyalgia
Fibromyalgia affects an estimated 2–4% of the global population, across ages, cultures, and incomes. Women are diagnosed more often than men, roughly 80–90% of identified cases, though under-recognition in men likely exists. Many live with overlapping conditions like IBS, migraines, endometriosis, POTS, or TMJ, which complicate the picture and delay answers. Because routine tests can look “normal,” prevalence is often underestimated. Growing awareness in primary care and workplaces helps shorten the road to validation and appropriate support. Surveys note family clustering and uneven access to care across regions.
Symptoms of Fibromyalgia
Symptoms can shift day to day. Widespread aching, burning, or throbbing may move across regions. Profound fatigue and low stamina are common, along with fibro fog—memory slips, slowed processing, and trouble concentrating. Sleep is often unrefreshing or disrupted. Many report sensitivity to light, sound, temperature, and touch, headaches, jaw pain, tingling, numbness, and IBS-like digestion. Symptoms may flare after stress, overexertion, travel, or poor sleep. Tracking patterns with a simple log can reveal triggers and guide pacing, treatment tweaks, and kinder expectations. Recognizing early “warning signs” helps head off bigger flares.
Causes & Theories for Fibromyalgia
No single cause explains fibromyalgia. Several mechanisms likely interact. Central sensitization—an over-responsive alarm system in the brain and spinal cord—amplifies pain and sensory input. Neurotransmitter differences in serotonin, norepinephrine, dopamine, and glutamate may alter pain modulation, mood, and sleep. Genetics increase vulnerability, while triggers like infections, physical injuries, hormonal shifts, or prolonged stress can set symptoms in motion. Autonomic changes and small-fiber nerve findings are under study, pointing to complex interplay among brain, nerves, hormones, and immunity. Understanding mechanisms reduces shame and guides personalized care.
Diagnosis of Fibromyalgia
There is no definitive lab test; diagnosis relies on history, symptoms, and excluding other explanations. Clinicians look for widespread pain lasting three months or more, often using the Widespread Pain Index and Symptom Severity Scale. Misdiagnosis is common—people may be labeled with arthritis, depression, or chronic fatigue alone. Normal bloodwork does not invalidate pain. A thoughtful evaluation reviews thyroid, anemia, autoimmune clues, sleep, and medications, while listening carefully to how symptoms limit daily life. Documenting function on good days versus flares helps tailor plans and justify accommodations.
Treatment of Fibromyalgia
Management is personalized and multi-modal. Medications may include SNRIs such as duloxetine or milnacipran, pregabalin or gabapentin for neuropathic pain, and cautious use of analgesics. Non-drug care is equally vital: cognitive behavioral therapy, gentle graded movement, physiotherapy, and occupational therapy to simplify tasks. Foundations like sleep hygiene, stress regulation, heat, and mindfulness help reduce flare intensity. Some benefit from acupuncture, massage, or pacing tools. Education about pain science reduces fear, and blended programmes align treatment with your goals, with regular reviews to refine what works.
Impact of Fibromyalgia
Fibromyalgia touches body, mind, and livelihood. Persistent pain, stiffness, and exhaustion limit stamina and mobility. Anxiety, depression, grief, and the trauma of dismissal are common. Work and study can be disrupted by absenteeism and presenteeism, while finances strain under healthcare costs and reduced hours. Relationships feel the weight of invisible pain and unpredictability. None of this reflects weakness; it reflects a serious condition that deserves validation, accommodations, and coordinated care from supportive teams. Community can buffer isolation and offer pacing strategies and workplace scripts.
Comorbidities of Fibromyalgia
Fibromyalgia frequently overlaps with chronic fatigue syndrome/ME, irritable bowel syndrome, migraines, temporomandibular joint disorder, interstitial cystitis, POTS, pelvic floor dysfunction, and—among women—endometriosis or adenomyosis. These combinations heighten pain, sensory sensitivity, and fatigue, complicating diagnosis and treatment. A coordinated plan that includes gastroenterology, neurology, pain medicine, gynecology, sleep, and physiotherapy helps untangle symptoms and avoid tunnel vision, treating the person rather than isolated parts. Screening for trauma, sleep disorders, and autonomic symptoms provides a fuller picture and clearer priorities.
Flares & Triggers for Fibromyalgia
Flares often follow stress, illness, travel, overexertion, hormonal shifts, weather changes—especially cold, damp, or abrupt swings—and poor sleep. Sensory overload or conflict can add fuel. Prevention focuses on pacing, realistic schedules, and buffers: planned rests, warmth, hydration, and gentle movement. When a flare hits, shrink the day—simplify tasks, use heat, breathwork, and low-stimulation spaces. Partners can help with chores, meals, and advocacy, protecting energy for recovery. A brief written “flare plan” with priority tasks and comfort tools restores control.
Lifestyle & Self-Management of Fibromyalgia
Self-management doesn’t cure fibromyalgia, but it builds capacity. Many benefit from regular, gentle movement—walking, stretching, tai chi, aquatherapy—balanced with rest. Nutrition that favors whole foods, adequate protein, and anti-inflammatory patterns while limiting ultra-processed sugars and excess caffeine can steady energy. Sleep hygiene—consistent bedtimes, wind-down routines, and light/digital limits—supports recovery. Pacing prevents boom-and-bust cycles; support groups reduce isolation and share practical hacks. Light tracking of sleep, steps, stress, and pain guides adjustments without perfectionism.
Awareness & Advocacy for Fibromyalgia
Fibromyalgia Awareness Day is May 12, symbolized by the purple ribbon. As an invisible illness, it faces stigma and dismissal that delay diagnosis and accommodations. Advocacy educates families, employers, schools, and clinicians about central sensitization and flare-based disability. Sharing stories, symptom logs, and workplace scripts can unlock understanding and policy changes. Partners can attend appointments, document patterns, and amplify the patient’s voice with respect. HR teams and unions can champion flexible schedules, remote options, and planned rest breaks.
Research & Future of Fibromyalgia
Research maps brain networks tied to pain amplification and sensory processing, examines neurotransmitter patterns and genetic links, and explores connections with autoimmune features and dysautonomia. Scientists aim to refine diagnostic criteria, develop biomarkers, and test targeted therapies that calm pain pathways with fewer side effects. Digital tools and wearables may track sleep, activity, and flares to personalize care. Patient-led advocacy accelerates progress and keeps studies focused on outcomes that matter in daily life—function, clarity, and sustainable relief.
Fibromyalgia Infographic
(FREE for You to Download Below)
My Wife’s Fibromyalgia
As I sit here writing this, my heart feels heavy with the memories of my wife’s battle with fibromyalgia. It’s been a long road. She tried to take her own life and asked me to divorce her, but I have never once thought about giving up on the love of my life.
I remember the first time she was diagnosed with fibromyalgia. She was diagnosed with it one year after her endometriosis diagnosis. Two painful chronic conditions in one year? We were both scared and confused, not knowing what the future held for us. But we decided to face it together, and we have been doing so ever since.
There have been many difficult moments along the way. There have been times when my wife was in so much pain that she could barely move, times when she was so exhausted that she couldn’t even get out of bed, and times when she felt so alone and hopeless that it broke my heart.
But through it all, I have tried to be there for her in any way that I can. I have learned how to listen when she needs to talk, how to hold her when she needs to cry, and how to make her laugh when she needs to smile.
I have also learned how to help her manage her symptoms. I have researched the latest treatments and therapies, and I have encouraged her to try them. I have helped her make lifestyle changes that have helped to reduce her pain and increase her energy. My focus was always placed on endometriosis being her primary condition, but I added to this blog a lot of information about fibromyalgia.
Most importantly, I have learned how to love her unconditionally. I have seen her at her worst, and I have loved her even more for it. I have watched her fight through the pain and the exhaustion, and I have been amazed by her strength and her courage.
I know that my wife’s battle with fibromyalgia is far from over. But I also know that we will face it together, with love, compassion, and hope. And I hope that our story will inspire others to do the same.
My Fibromyalgia eBook
Imagine waking up every day feeling exhausted, in pain, and unable to do the things you used to enjoy. This is the reality for many people living with fibromyalgia. It’s a condition that can leave you feeling isolated and alone, as if no one understands what you’re going through. But it doesn’t have to be this way…
If you are a man who loves a woman with fibromyalgia, I know that you want to help her as much as you can. But sometimes, it can be difficult to understand what she is going through and how to best support her.
That’s why I wrote my eBook, specifically tailored for male partners of women with fibromyalgia. In it, I share my personal experiences and insights from my own journey with my partner’s fibromyalgia. I offer practical tips on how to communicate effectively, how to help manage symptoms, and how to take care of your own mental and emotional health.
But this eBook is more than just a practical guide. It’s a heartfelt expression of love and compassion for all those who are affected by fibromyalgia. I understand the pain and frustration that comes with seeing someone you love suffer, and I want to help you navigate this journey with as much grace and strength as possible.
I invite you to join me on this journey of love and support. Together, we can create a better future for those who live with fibromyalgia, and for those who love them.
“Fibromyalgia for Caring Partners”
Understanding what fibromyalgia is and how it affects your partner can help you better support and care for them. This book is perfect for men who want to learn about fibro, how to cope with their own struggles, and how to help their partner battle this condition.
It gives you an intimate view of the challenges and triumphs of living with fibromyalgia because caring for a partner with fibro can be very challenging, as this condition can cause chronic pain and fatigue, as well as other symptoms that can impact daily life.
“Fibromyalgia for Caring Partners” is a must-read for anyone to better understand this condition.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MORE