As a woman, you might know about PCOS and endometriosis. These health issues can really affect your life. PCOS and endometriosis both cause pelvic pain, but the reasons and types of pain are different. Knowing how PCOS and endometriosis pain differ is key to finding the right treatment.
First, let’s look at what makes each pain unique. Endometriosis happens when tissue that should be inside the uterus grows outside. This tissue can cause inflammation and scarring, leading to severe pain during menstruation and sex.
PCOS, on the other hand, is a hormonal imbalance that can cause cysts on the ovaries. Symptoms include irregular periods, too much hair, acne, and pelvic pain. PCOS pain is usually a dull ache that gets worse around ovulation or menstruation.
The main difference is where the pain is felt. Endometriosis pain is mainly in the lower abdomen and pelvis. PCOS pain can also be in the lower back or upper abdomen. Also, endometriosis pain gets worse with activities like sex or bowel movements, while PCOS pain is more tied to the menstrual cycle.
The pain’s severity also varies. Endometriosis pain is often very severe and can really limit daily activities. PCOS pain is significant but might be easier to manage for some women.
Understanding the difference between PCOS and endometriosis pain is important. It helps doctors diagnose and treat you better. By knowing these differences, you can work with your doctor to find the best way to manage your symptoms.
Understanding Polycystic Ovarian Syndrome (PCOS)
Polycystic ovarian syndrome (PCOS) is a common endocrine disorder in women of childbearing age. It happens when the ovaries make too much of a male hormone called androgens. This hormone imbalance messes with ovulation and causes symptoms.
What is PCOS?
PCOS affects about 5 to 10 percent of women. It’s marked by many small cysts on the ovaries. These cysts can lead to irregular periods, too much hair, acne, and more.
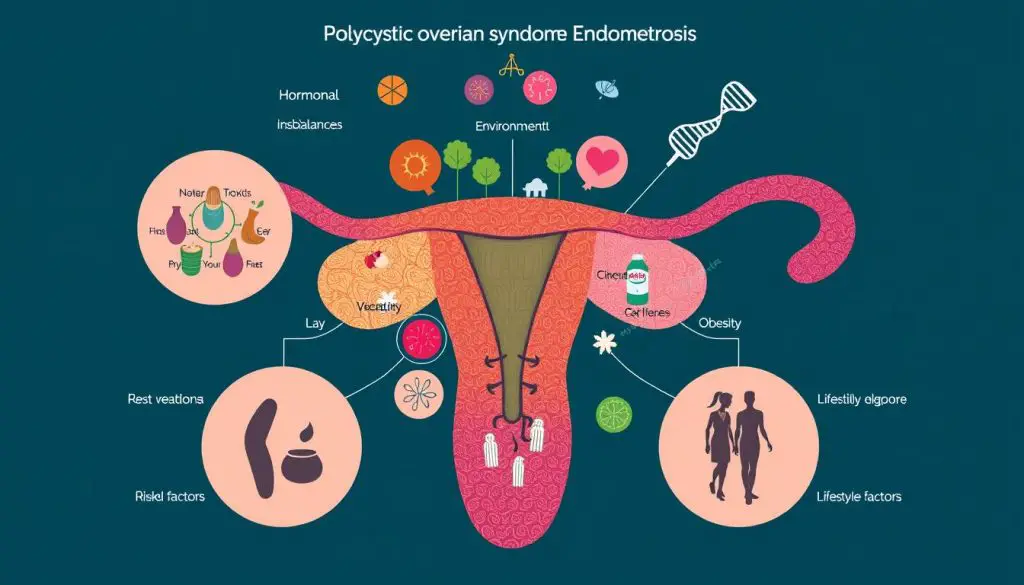
Causes of PCOS
The exact cause of PCOS is not known, but genetics, insulin resistance, and inflammation play a part. Insulin resistance makes cells less responsive to insulin. This can increase androgens, worsening the hormonal imbalance.
Other things that might contribute to PCOS include:
- Obesity, which can make insulin resistance worse and increase polycystic ovarian syndrome pain
- Genetics, as PCOS often runs in families
- Androgen excess, which can mess with ovary function
- Low-grade inflammation, which might help cause PCOS
Knowing what causes PCOS is key to managing it. It helps doctors create care plans that meet each patient’s needs.
Symptoms of Polycystic Ovarian Syndrome Pain
Polycystic Ovarian Syndrome (PCOS) is a common hormonal disorder in women of childbearing age. It often causes pain in different ways. Women with PCOS may have missed or irregular periods, a key sign of the condition.
PCOS can also cause too much androgen, leading to hirsutism (excessive hair growth), acne, and weight gain. These hormonal imbalances add to the discomfort and pain women with PCOS feel.
The pain from PCOS is different from endometriosis pain. Endometriosis pain is sharp and stabbing. PCOS pain is dull and aching, spreading through the pelvic area.
- Irregular or missed periods
- Excess hair growth (hirsutism)
- Acne
- Weight gain
- Pelvic pain
Not all women with PCOS feel the same pain. The severity and type of symptoms can vary a lot. If you’re dealing with persistent or concerning symptoms, see a healthcare professional for help.
https://www.youtube.com/watch?v=Az9lWdqebaU
Understanding Endometriosis
Endometriosis is a complex condition that affects millions worldwide. It involves the growth of tissue like the uterus lining outside the uterus. This tissue can be found on ovaries, fallopian tubes, and even the bladder or intestines.
What is Endometriosis?
Endometriosis is a chronic condition that causes severe pelvic pain and irregular periods. The tissue outside the uterus thickens and bleeds with each cycle. Unlike the uterine lining, it can’t exit the body, leading to inflammation and scarring.
Causes of Endometriosis
The exact cause of endometriosis is not known. But several theories exist:
- Retrograde menstruation, where menstrual blood and tissue flows back through the fallopian tubes and implants on the pelvic organs
- Metaplasia, a process where cells change into a different cell type
- Immune system dysfunction, which may allow the endometrial tissue to grow and persist outside the uterus
- Genetic factors, as endometriosis appears to run in families
Understanding endometriosis is key to providing the right treatment and support. With ongoing research, there’s hope for better management and recognition of this condition in the future.
Symptoms of Endometriosis Pain
Endometriosis is a chronic condition where tissue like the uterine lining grows outside the uterus. This misplaced tissue can cause severe pain, often during menstrual periods. If you have endometriosis, you may face various symptoms that can greatly affect your life.
Painful periods (dysmenorrhea) are a common symptom. The cramps from endometriosis are usually more severe and last longer than usual. These can be accompanied by nausea, fatigue, and diarrhea.
Endometriosis can also lead to pain during or after sexual intercourse (dyspareunia). The misplaced tissue can get irritated and inflamed during sex, causing discomfort.
Another symptom is chronic pelvic pain. This pain can be felt in the lower abdomen, back, or even the rectum. It can last throughout the menstrual cycle, not just during periods.
Heavy or irregular bleeding is also common. Some may have longer or heavier periods, while others may bleed between periods.
The severity of symptoms doesn’t always match the extent of endometriosis. Some with minimal endometriosis may have severe pain, while others with more advanced endometriosis may have little to no symptoms. If you’re experiencing these symptoms, it’s important to see a doctor for a proper diagnosis and treatment.

Polycystic Ovarian Syndrome Pain vs Endometriosis Pain
Both Polycystic Ovarian Syndrome (PCOS) and endometriosis can cause painful cramps and fertility issues. But, the pain they cause is different. Women with PCOS might feel pelvic pain, but it’s not as bad as the pain from endometriosis.
Endometriosis pain gets worse during menstrual cycles and can include nausea, fatigue, and diarrhea. On the other hand, PCOS pain doesn’t get worse during periods. It’s also less severe and only in one area, unlike endometriosis which causes widespread pain.
| Symptom | PCOS Pain | Endometriosis Pain |
|---|---|---|
| Pelvic Pain | Milder and less localized | Severe and debilitating |
| Menstrual Cramps | May not significantly worsen during periods | Typically worse during menstruation |
| Additional Symptoms | Nausea, fatigue, and diarrhea not as common | Nausea, fatigue, and diarrhea often present |
Getting an early diagnosis and treatment is key for both PCOS and endometriosis. It’s important for your quality of life. Always talk to a healthcare professional for the right diagnosis and treatment.
Risk Factors for PCOS and Endometriosis
Polycystic Ovarian Syndrome (PCOS) and endometriosis are two health issues that can share some risk factors. Knowing what increases the chance of getting each condition is key. This helps in catching them early and managing them well.
PCOS Risk Factors
The main risk factors for PCOS are:
- Genetics: Studies show that PCOS often runs in families, pointing to a genetic link.
- Insulin Resistance: This is a big part of PCOS. It can lead to the condition.
- Obesity: Being overweight or obese is common in women with PCOS, affecting up to 80%.
Endometriosis Risk Factors
The main risk factors for endometriosis are:
- Family History: Having a close relative with endometriosis raises your risk.
- Early Onset of Periods: Starting periods before 12 increases your risk of endometriosis.
- Longer or More Frequent Menstrual Cycles: Women with longer or more frequent cycles are more likely to have endometriosis.
Both PCOS and endometriosis can lead to other health issues, like diabetes and infertility. Spotting these risk factors early and managing them well is vital for reproductive health.
Diagnosing PCOS and Endometriosis
Getting a correct diagnosis is key for managing PCOS and endometriosis. These conditions share some symptoms, but each has its own diagnostic process.
Diagnosing PCOS
To diagnose PCOS, doctors use a pelvic exam, ultrasound, and blood tests. The pelvic exam looks for signs like extra hair or big ovaries. An ultrasound checks for polycystic ovaries. Blood tests measure hormones and glucose to confirm PCOS.
Diagnosing Endometriosis
Diagnosing endometriosis is harder because it needs a laparoscopic procedure to see endometrial tissue outside the uterus. Doctors might also use an ultrasound or MRI to spot endometriosis. Your symptoms and medical history are also reviewed to confirm endometriosis.
Getting a proper diagnosis for PCOS or endometriosis quickly is important. It lets you start treatment to manage symptoms and feel better.
Can You Have Both PCOS and Endometriosis?
Yes, a woman can have both Polycystic Ovarian Syndrome (PCOS) and endometriosis. This is not very common. Research shows that about 7-8% of women with PCOS also have endometriosis. The endometriosis in these cases is usually mild.
Why some women have both conditions is not fully understood. But studies have given us some clues:
- A 2015 study found that women with PCOS were more likely to have endometriosis.
- A 2011 study suggested that high androgens and insulin in PCOS might raise estradiol levels. This could increase the risk of endometriosis.
PCOS and endometriosis share some symptoms. These include fertility issues, heavy periods, irregular bleeding, and long periods. This makes it hard to tell the two conditions apart.
Women with PCOS should watch for signs of endometriosis. Seeing a healthcare provider regularly is key. This helps get a diagnosis and treatment early, improving life quality for those with both conditions.
| Statistic | Value |
|---|---|
| Overlap prevalence of endometriosis and PCOS | 2% to 5% |
| Estimated incidence of PCOS in the UK | Approximately 1 in 10 women |
| Average time to receive an endometriosis diagnosis | 8 years |
| Probability of subfertility with both conditions | 10-fold higher |
| Increased pelvic pain in patients with both conditions | Reported |
Treating Polycystic Ovarian Syndrome Pain
Living with polycystic ovarian syndrome (PCOS) can be tough. But, there are ways to manage the pain and symptoms. While there’s no cure, a mix of treatments can ease your discomfort and lower the risk of future problems.
Birth control pills are a key treatment for PCOS. They help control your menstrual cycle, reduce unwanted hair, and improve how your body uses insulin. Medications like metformin can also be used to control blood sugar and manage symptoms.
Managing your weight is also key. Eating well and exercising regularly can make a big difference. Losing just 5% of your body weight can improve PCOS symptoms. Keeping your Body Mass Index (BMI) between 18.5 and 24.9 can also help reduce PCOS’s effects and lower health risks.
If diet and medication aren’t enough, your doctor might suggest other treatments. This could include laparoscopic ovarian drilling or in vitro fertilization (IVF) for fertility issues. These treatments can help balance hormones and improve reproductive health.
Remember, treating PCOS effectively means a plan that fits you. Work with your healthcare team to create a treatment plan that tackles your pain and supports your overall health.
| Treatment | Description | Benefits |
|---|---|---|
| Birth control pills | Hormonal contraceptives that regulate menstrual cycles and reduce excessive hair growth | Helps manage PCOS symptoms, improve insulin sensitivity |
| Insulin-regulating medications | Drugs like metformin that lower blood sugar levels and improve insulin resistance | Reduces PCOS-related symptoms, supports weight management |
| Weight management | Maintaining a healthy BMI through a balanced diet and regular exercise | Significantly improves PCOS symptoms and reduces long-term health risks |
| Laparoscopic ovarian drilling | Surgical procedure that corrects hormone imbalances and restores normal ovarian function | Helps improve fertility and regulate menstrual cycles in women with PCOS |
| In vitro fertilization (IVF) | Assisted reproductive technology to help women with PCOS conceive | Increases the chances of successful pregnancy for those struggling with PCOS-related infertility |
Treating Endometriosis Pain
There’s no cure for endometriosis, but symptoms can be managed. Treatments include pain medication, hormone therapy, and surgical interventions. The right treatment depends on how severe the endometriosis is and what the person wants to achieve.
Pain medication is often the first choice for treating endometriosis. Over-the-counter NSAIDs like ibuprofen or naproxen can help with cramps. For more severe pain, doctors might prescribe stronger pain relievers.
Hormone therapy is also common. Hormonal birth control can help control the menstrual cycle and reduce endometrial growth. Sometimes, GnRH agonists or antagonists are used to stop menstruation and lessen pain.
For those with severe endometriosis, surgical treatment might be needed. Laparoscopic surgery can remove lesions and scar tissue. In extreme cases, a hysterectomy might be considered. These surgeries can help with pain, but they don’t cure endometriosis.
Managing endometriosis often requires a mix of medical, surgical, and lifestyle changes. It’s important to work with a healthcare provider to create a treatment plan. This helps manage symptoms and improve life quality for those with this chronic condition.

| Endometriosis Treatment Options | Description |
|---|---|
| Pain Medication | Over-the-counter NSAIDs, prescription pain relievers |
| Hormone Therapy | Hormonal birth control, GnRH agonists/antagonists |
| Surgery | Laparoscopy, hysterectomy |
Long-term Effects of Untreated PCOS and Endometriosis
Untreated PCOS and endometriosis can deeply affect a woman’s health and happiness. These conditions can harm fertility, raise the risk of chronic diseases, and lower quality of life.
PCOS, affecting 8-13% of women of childbearing age, is a common hormonal disorder. Up to 70% of women with PCOS go undiagnosed globally. Without treatment, PCOS can increase the risk of type 2 diabetes, high blood pressure, and uterine cancer. It also makes it harder for women to get pregnant due to anovulation.
Endometriosis, a chronic and painful condition, can also have severe effects if not treated. It can cause severe pelvic pain, heavy bleeding, and infertility. Over time, it can lead to scar tissue and adhesions, worsening pain and fertility issues.
| Condition | Long-term Effects |
|---|---|
| PCOS |
|
| Endometriosis |
|
Untreated, PCOS and endometriosis can greatly affect a woman’s life and health. It’s vital for those with symptoms to get medical help and follow a treatment plan. This can help manage the condition and prevent long-term problems.
Lifestyle Changes to Manage PCOS and Endometriosis
Medical treatments are just the start for managing PCOS and endometriosis. Making lifestyle changes is also key. A healthy diet, regular exercise, and stress management can help. These steps can ease pain, balance hormones, and boost your overall health.
Women with PCOS should eat foods high in fiber. This includes whole grains, fruits, and veggies. Aim for 21 to 25 grams of fiber daily. Foods like leafy greens, fatty fish, and olive oil can also fight inflammation. Plus, exercising vigorously for 120 minutes a week can help with symptoms and fertility.
Those with endometriosis might find relief in a gluten-free diet and A2 casein-based dairy. Stress-reducing activities like yoga, meditation, and mindfulness are also beneficial. And, don’t forget about the benefits of moderate exercise for pain relief and well-being.
Source Links
- https://www.kofinasfertility.com/patient-info/pcos-and-endometriosis
- https://www.hackensackmeridianhealth.org/en/healthu/2021/08/10/pcos-vs-endometriosis-whats-the-difference
- https://www.ncbi.nlm.nih.gov/books/NBK459251/
- https://www.uptodate.com/contents/polycystic-ovary-syndrome-pcos-beyond-the-basics/print
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/polycystic-ovary-syndrome-pcos
- https://www.webmd.com/women/what-is-pcos
- https://www.whria.com.au/for-patients/hormones/polycystic-ovarian-syndrome/
- https://www.healthline.com/health/womens-health/endometriosis-vs-pcos
- https://drseckin.com/endometriosis-and-pcos/
- https://www.verywellhealth.com/endometriosis-and-pcos-5295536
- https://www.charlotteradiology.com/blog/endometriosis-pcos-uterine-fibroids/
- https://www.who.int/news-room/fact-sheets/detail/endometriosis
- https://www.livi.co.uk/your-health/severe-period-pain-endometriosis-or-pcos-how-can-you-tell-the-difference/
- https://www.aucmed.edu/about/blog/endometriosis-vs-pcos-explained
- https://www.medicalnewstoday.com/articles/endometriosis-vs-pcos
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9361725/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10472311/
- https://www.endonews.com/the-overlap-of-endometriosis-and-polycystic-ovarian-syndrome
- https://www.mariongluckclinic.com/blog/can-you-have-pcos-and-endometriosis.html
- https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/treatment/
- https://www.ncbi.nlm.nih.gov/books/NBK278959/
- https://graceprivate.com.au/eating-to-manage-endometriosis-and-pcos/
- https://doctorconnor.com/coping-with-endometriosis-and-polycystic-ovary-syndrome-pcos/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2683463/
- https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome
- https://www.aafp.org/pubs/afp/issues/2000/0901/p1079.html/1000
- https://www.webmd.com/women/what-to-know-about-lifestyle-changes-for-pcos
- https://www.healthline.com/health/pcos-diet
- https://progyny.com/education/female-infertility/what-do-you-eat-if-you-have-pcos-or-endo-find-out/
