Ever felt like your period is more than just a normal pain? It might be endometriosis, where tissue like the uterus grows outside it. This tissue reacts to hormones, causing inflammation and scarring. It leads to severe pelvic pain during your menstrual cycle.
Endometriosis affects about 176 million women and individuals assigned female at birth worldwide. The exact causes are not known, but several factors might play a role. Understanding these can help find the right treatment and support.
So, what causes the severe menstrual cramps and pelvic symptoms in endometriosis? Let’s explore the underlying factors that might be causing your pain.
Understanding Endometriosis: A Condition Beyond the Uterus
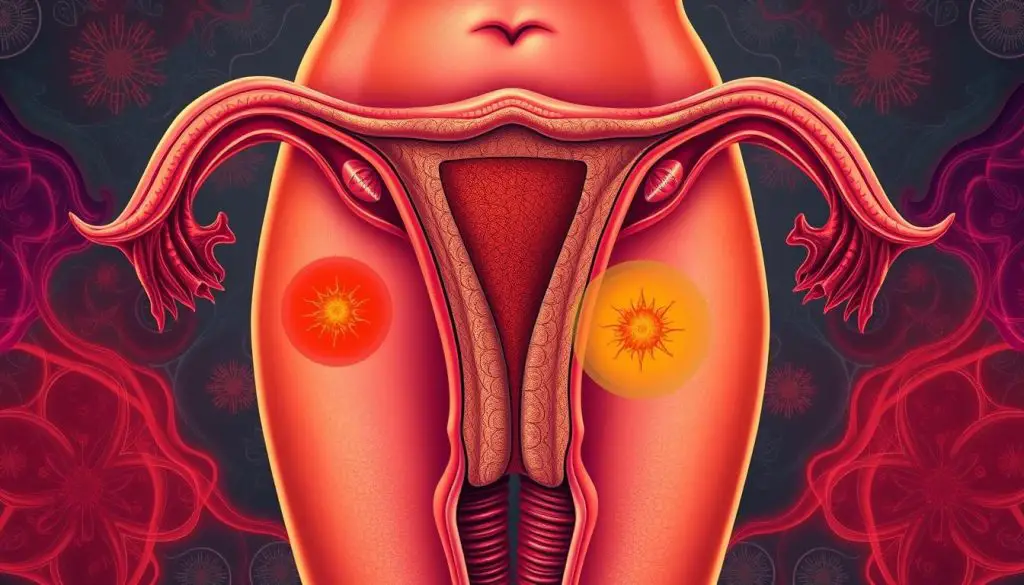
Endometriosis is a complex condition that affects more than just the uterus. It’s a disorder where tissue like the uterine lining, called the endometrium, grows outside the uterus. This tissue can grow on the ovaries, fallopian tubes, and even nearby organs like the bladder and bowel.
What is Endometriosis?
Endometriosis is a chronic and painful condition. The endometrial-like tissue, which normally lines the uterus, grows outside it. This tissue reacts to monthly hormonal changes, causing inflammation, scarring, and adhesions. These can lead to significant pain and other symptoms.
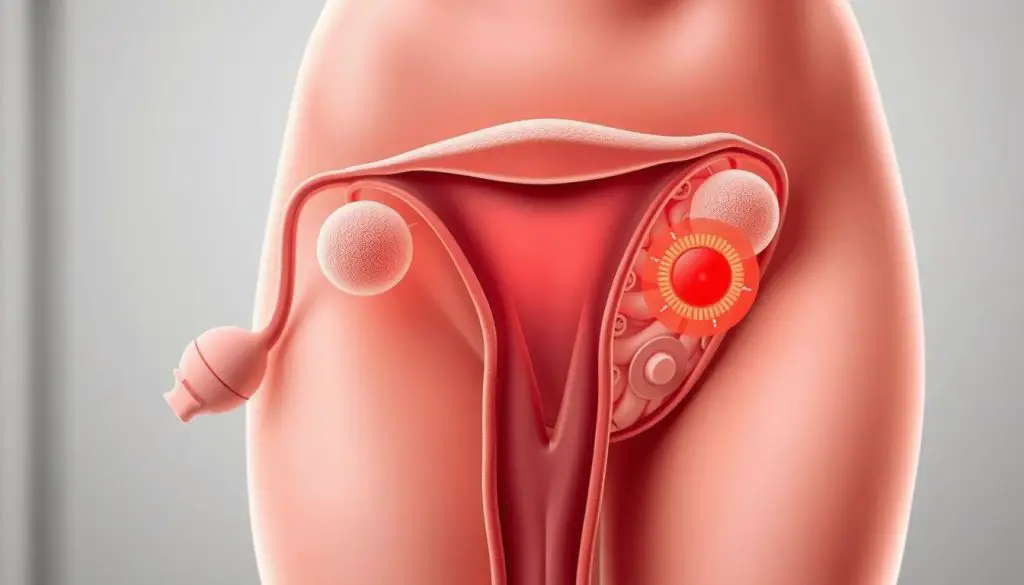
Where Does Endometrial Tissue Grow?
In endometriosis, the endometrial-like tissue grows in various places in the pelvic area. It can be found on the ovaries, fallopian tubes, outer surface of the uterus, and even on the bladder, intestines, and other nearby organs. This abnormal tissue growth causes adhesions, scarring, and cysts. These contribute to the painful symptoms of the condition.
https://www.youtube.com/watch?v=8viFSWE_t9Q
The misplaced tissue can also grow in distant locations, such as the diaphragm, lungs, and even the brain. Though this is less common. No matter where it grows, this tissue responds to hormonal changes. This leads to inflammation, pain, and other symptoms that can greatly affect a person’s quality of life.
Common Symptoms: Recognizing the Signs
Endometriosis can cause a range of painful symptoms that affect daily life. The most common symptom is pelvic pain. This pain can happen during or outside of the normal menstrual period. It’s often worse than usual menstrual cramps and can also cause lower back or abdominal pain.
Pelvic Pain During and Outside Periods
Pelvic pain from endometriosis can start before the period and last for days after. This secondary dysmenorrhea is due to endometrial tissue growing outside the uterus. It can cause bleeding, inflammation, and scarring.
Painful Intercourse and Bowel Movements
People with endometriosis may also find sex and bowel movements painful. These symptoms can really hurt and make everyday life hard. They can also affect personal relationships and daily activities.
Ovarian Cysts and Infertility
Endometriosis can cause ovarian cysts, leading to more pain. It can also make it hard to get pregnant. The growth of endometrial tissue can harm the reproductive organs.
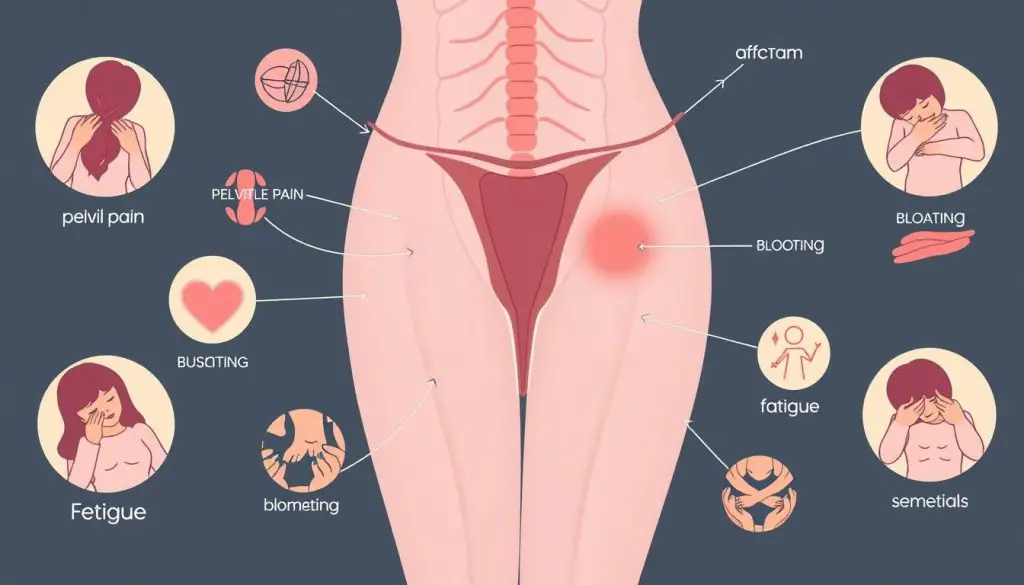
The pain from endometriosis can vary a lot. Some people might only feel a little discomfort, while others face severe pain. Getting medical help and working with doctors is key to managing symptoms and improving health.
Causes of Painful Periods: Exploring the Factors
The causes of painful periods, or dysmenorrhea, are varied and complex. Some women feel minor discomfort, while others face severe cramps and pain. A major cause is endometriosis.
In endometriosis, the uterine lining grows outside the uterus, often near the ovaries or under the uterus. This misplaced tissue builds up and breaks down during the cycle. It causes bleeding inside the pelvis, leading to inflammation, swelling, and scarring. This is why endometriosis causes such intense pain.
Other causes include uterine fibroids, pelvic inflammatory disease, and uterine defects like a bicornuate or septate uterus. These can disrupt the uterus’s normal function, causing severe cramps and discomfort.
| Condition | Potential Causes of Painful Periods |
|---|---|
| Endometriosis | Misplaced endometrial tissue growth outside the uterus, leading to inflammation and scarring |
| Uterine Fibroids | Noncancerous growths in the uterus that can disrupt normal uterine function |
| Pelvic Inflammatory Disease | Infection of the female reproductive organs, causing inflammation and pain |
| Structural Uterine Defects | Abnormal uterine shapes or divisions that can interfere with normal menstrual flow and cause cramps |
Knowing the causes of painful periods is key for women seeking relief. Working with a healthcare provider helps navigate menstrual health complexities. Together, they can find effective ways to manage symptoms.
Risk Factors: Who is Prone to Endometriosis?
Endometriosis is a complex condition. Certain factors can increase your risk of developing it. Knowing these risk factors can help you take care of your reproductive health.
Family History and Genetics
If you have a family member with endometriosis, like a mother, sister, or grandmother, you’re more likely to get it too. This shows that genetics play a role in the disease. Studies have found that those with a family history of endometriosis are at higher risk.
Early Menstrual Cycles and Heavy Bleeding
Endometriosis is linked to certain menstrual traits. Women with cycles under 27 days or periods over eight days are at higher risk. These traits can signal a higher chance of developing endometriosis.
Never Giving Birth
Women who have never given birth face a higher risk of endometriosis. Pregnancy and childbirth can sometimes ease symptoms. This might explain why nulliparous women are at higher risk.
Knowing these risk factors helps you work with your healthcare provider. This way, you can monitor your reproductive health closely. Early diagnosis and treatment are key to managing endometriosis and improving your life quality.
Diagnosing Endometriosis: The Path to Understanding
Finding out if you have endometriosis can take several steps. First, your doctor will talk to you about your symptoms. They will also do a pelvic exam. This exam checks for any problems in your reproductive organs.
Imaging Tests: Ultrasound and MRI
Your doctor might also use ultrasound or MRI to see inside your body. These tests can show if you have endometrial-like tissue or cysts. They help find signs of endometriosis.
Laparoscopy: Confirming the Diagnosis
The best way to know for sure is through laparoscopy. This surgery lets a doctor look inside your belly with a camera. They can see if you have endometrial implants and take a sample for a biopsy.
Getting a diagnosis for endometriosis can be tough. But with the right team and tools, you can get answers. Your doctor will work with you to find the cause of your symptoms. They will then create a treatment plan just for you.
| Diagnostic Method | Description |
|---|---|
| Pelvic Exam | A hands-on assessment of the reproductive organs to identify abnormalities or areas of concern. |
| Ultrasound | A non-invasive imaging test that can reveal the presence of endometrial-like tissue, cysts, or other indicators of endometriosis. |
| MRI | Another non-invasive imaging test that can provide a more detailed view of the internal structures, particularlly for endometriosis of the ovaries or severe cases. |
| Laparoscopy | A minimally invasive surgical procedure that allows the surgeon to visually inspect for endometrial implants and adhesions, as well as collect a tissue sample for biopsy to confirm the diagnosis. |
Treatment Options: Managing Endometriosis Symptoms
Endometriosis can be tough to manage, but there are many ways to ease the symptoms. First, doctors often use over-the-counter pain medication or hormone therapy to help manage pain.
Pain Medication and Hormone Therapy
NSAIDs like ibuprofen or naproxen can reduce inflammation and ease endometriosis-related pain. Hormonal birth control pills, patches, or rings can also help control hormonal changes that cause symptoms.
GnRH agonists and aromatase inhibitors are other hormone therapy options. These medications lower estrogen levels, which can slow down the growth of endometrial tissue.
Surgical Intervention for Severe Cases
If pain medication and hormone therapy don’t work, surgery might be needed. Laparoscopy, a minimally invasive technique, can remove or destroy the problematic tissue.
But, it’s key to know that endometriosis can come back in up to 20 out of 100 women within five years. Also, about 1 out of 100 women might face complications like organ injuries, infections, or heavy bleeding after surgery.
| Treatment Options | Effectiveness | Potential Risks |
|---|---|---|
| Pain Medication | Relieves pain and inflammation | Potential side effects, such as stomach irritation |
| Hormone Therapy | Suppresses endometrial growth and hormone fluctuations | Menopausal-like side effects, such as hot flashes and mood changes |
| Laparoscopic Surgery | Provides long-term relief for up to 70% of women | Organ injuries, infections, and heavy bleeding in 1% of cases |
| Hysterectomy and Oophorectomy | Achieves long-term cure in over 90% of women | Sudden early menopause and the need for hormone replacement therapy |
Choosing the right endometriosis treatment depends on your symptoms, fertility plans, and how severe it is. It’s vital to work with your healthcare provider to find a treatment plan that fits your needs.

Coping with Endometriosis: Finding Support
Living with endometriosis can be tough, both physically and emotionally. But, you’re not alone. Joining a support group can offer a sense of community and understanding. It also provides valuable tips on managing the condition.
Joining Support Groups
Support groups, both in-person and online, are safe spaces for women with endometriosis. They can share their stories and learn from each other. These groups are a great resource for [endometriosis coping], providing emotional support and practical advice.
Lifestyle Changes and Self-Care
- Stress Management: Stress-reducing techniques like meditation, yoga, or deep breathing can help with pain.
- Dietary Adjustments: Eating anti-inflammatory foods like leafy greens, fatty fish, and turmeric may help manage symptoms.
- Regular Exercise: Light to moderate physical activity, such as walking or swimming, can improve well-being and pain management.
By actively managing your condition through lifestyle changes and self-care, you can improve your life. This approach can help you better manage the challenges of endometriosis.
Endometriosis and Infertility: Understanding the Connection
Endometriosis is a chronic condition that often makes it hard to get pregnant. Studies show that 30-50% of people with endometriosis face fertility issues. The misplaced tissue can block sperm and egg movement, making it tough to conceive.
Endometriosis can also damage the fallopian tubes and ovaries. This damage can lead to scarring and inflammation. Research suggests that those with endometriosis have a 1-10% chance of getting pregnant each month. This is much lower than the 10-20% chance for those without it.
Endometriosis is a common reason for infertility. Doctors often use laparoscopy to diagnose it, if symptoms are severe. The study found that 7.4% of fertile women have endometriosis, but this number jumps to 40% for infertile women.
| Condition | Chance of Pregnancy per Month |
|---|---|
| No Endometriosis | 10-20% |
| Surgically Documented Endometriosis | 1-10% |
If you’re dealing with endometriosis and infertility, talk to a healthcare professional. They can offer tailored advice and explore treatment options to boost your chances of getting pregnant.
Seeking Professional Guidance: When to See a Specialist
If you’re dealing with severe symptoms like endometriosis symptoms, it’s time to see a doctor. Your primary gynecologist can start by checking you out. But, seeing an endometriosis specialist or pelvic pain specialist might help more. They can do more tests and create a treatment plan just for you.
These experts know a lot about endometriosis symptoms. They can do detailed exams and order tests like ultrasounds. They might even do surgery to check for endometriosis and see how bad it is.
An infertility specialist might also help if you’re having trouble getting pregnant. They can give treatments like hormones or surgery to help you conceive.
Seeing a specialist for endometriosis, pelvic pain, or infertility is smart. They can make sure you get the right care. This way, you can manage your symptoms better and live a better life.
| Reasons to See a Specialist | Benefits of Specialist Care |
|---|---|
|
|
Endometriosis: A Journey of Awareness and Empowerment
Endometriosis is a complex and often misunderstood condition. It affects about 176 million people worldwide. By raising awareness and advocating for better understanding, those with endometriosis can take charge of their health.
Connecting with support groups and staying updated on research can help. Working closely with healthcare providers is also key. This way, you can manage your symptoms and improve your well-being.
Despite its impact, many people don’t know about endometriosis. In the UK, over 62% of women aged 16 to 24 are unaware. By promoting empowerment and access to resources, you can advocate for your health.
Organizations like the ENPOWR Project are leading the way. They focus on educating adolescents about endometriosis and menstrual health. Their goal is to reduce the 10-year delay in diagnosis and empower people to recognize and manage symptoms.
By supporting these initiatives, you can help ensure no one faces this journey alone. Together, we can make a difference in raising awareness and empowerment.
Source Links
- https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656
- https://my.clevelandclinic.org/health/diseases/10857-endometriosis
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/endometriosis
- https://www.who.int/news-room/fact-sheets/detail/endometriosis
- https://medlineplus.gov/ency/article/000915.htm
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/dysmenorrhea
- https://utswmed.org/conditions-treatments/heavy-bleeding-and-painful-periods/
- https://www.mayoclinic.org/diseases-conditions/menstrual-cramps/symptoms-causes/syc-20374938
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8943241/
- https://www.everydayhealth.com/pictures/reasons-your-period-might-painful/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5737931/
- https://www.nichd.nih.gov/health/topics/endometri/conditioninfo/at-risk
- https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661
- https://nyulangone.org/conditions/endometriosis/diagnosis
- https://medicine.yale.edu/news/yale-medicine-magazine/article/endometriosis
- https://www.ncbi.nlm.nih.gov/books/NBK279498/
- https://www.thewomens.org.au/health-information/periods/endometriosis/treating-endometriosis
- https://www.newhopefertility.com/blog/coping-with-endometriosis/
- https://www.healthline.com/health/endometriosis
- https://www.massgeneral.org/obgyn/fertility/news/endometriosis-and-its-impact-on-fertility
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3538128/
- https://www.ncbi.nlm.nih.gov/books/NBK279324/
- https://www.healthdirect.gov.au/painful-periods
- https://www.nhsinform.scot/healthy-living/womens-health/girls-and-young-women-puberty-to-around-25/periods-and-menstrual-health/period-pain-dysmenorrhoea/
- https://www.ncbi.nlm.nih.gov/books/NBK565622/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10035241/
- https://www.endofound.org/enpowr
