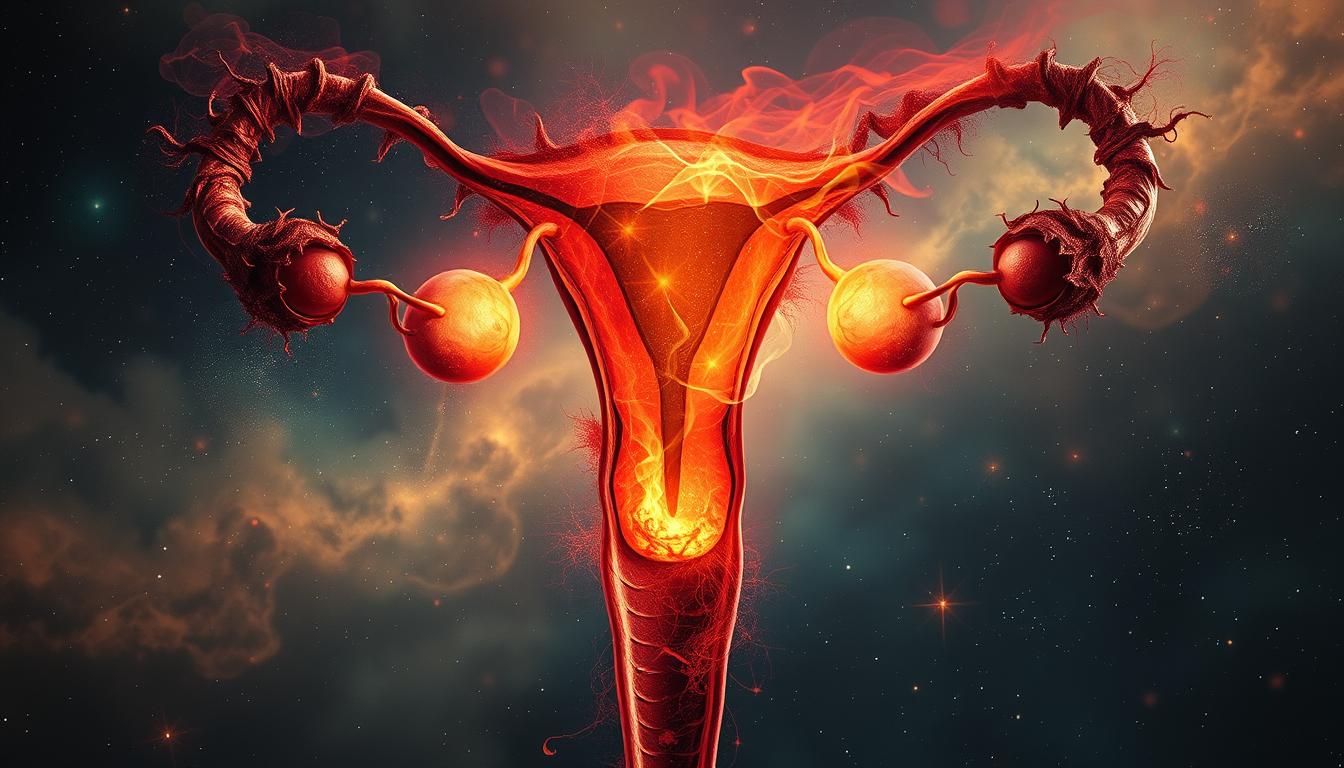
Are you one of the many women struggling with ovarian pain? The cause might be endometriosis. This complex disorder can cause a lot of pain in your pelvic area. But what causes this pain, and how can you feel better? Find out in this detailed guide.
Endometriosis happens when tissue like the uterine lining grows outside the uterus. This tissue can attach to the ovaries, fallopian tubes, and other pelvic areas. It leads to inflammation, scarring, and adhesions, causing severe pain.
The exact reason for endometriosis is not known. But studies point to hormonal imbalances, immune system issues, and genetics. Women who have never had a child, have short menstrual cycles, or have a family history are more likely to get it.
Understanding Endometriosis and Ovarian Pain
Endometriosis is a chronic condition where tissue like the uterus lining grows outside the uterus. It often appears on the ovaries, fallopian tubes, and other pelvic organs. This misplaced tissue reacts to the menstrual cycle, causing inflammation and scarring. It leads to severe pelvic pain, heavy bleeding, and sometimes infertility.
What is Endometriosis?
Endometriosis affects about 10% (190 million) of women and girls of reproductive age worldwide. It’s a complex disease where tissue like the uterus lining grows outside the uterus. This tissue can appear on the ovaries, fallopian tubes, and even the bladder or intestines.
Symptoms of Ovarian Endometriosis
The main symptom of ovarian endometriosis is a fixed or pulling sensation in the pelvis. It starts with ovulation and lasts until the menstrual period ends. Other symptoms include:
- Severe menstrual cramps
- Heavy or irregular bleeding
- Chronic pelvic pain
- Pain during sexual intercourse
- Fatigue, nausea, and digestive issues
It’s key to remember that symptom severity doesn’t always match disease extent. Some women with extensive endometriosis may not feel much pain or have other symptoms.
ovarian pain causes
Ovarian pain can be a complex issue with many causes. Endometriosis is a common cause. It happens when tissue like the uterine lining grows outside the uterus, often near the ovaries. This can cause inflammation, scarring, and adhesions, leading to pain.
Ovarian cysts are another cause of pain. These are fluid-filled sacs on the ovaries. While most are harmless, big cysts or ruptured ones can cause a lot of pain.
Pelvic inflammatory disease (PID) is also a common cause. It’s a bacterial infection of the reproductive organs. It can cause inflammation, swelling, pain, and other symptoms.
| Condition | Prevalence |
|---|---|
| Ovulation pain (Mittelschmerz) | Occurs in approximately 20% of women |
| Ovarian cysts | Present in around 8% of premenopausal women |
| Endometriosis | Affects approximately 10% of women of reproductive age |
| Pelvic inflammatory disease (PID) | Affects about 4.4% of sexually active women aged 18-44 |
Ovarian pain can also stem from other pelvic issues like uterine fibroids, ectopic pregnancies, and ovarian tumors. If you have persistent or severe pain, see a doctor. It could be a sign of a serious problem.
Endometriosis and Ovarian Cysts
Endometriosis is a chronic condition that often leads to ovarian cysts called endometriomas or “chocolate cysts.” These cysts are filled with dark, old blood that looks like chocolate. They are a key sign of ovarian endometriosis and can cause fertility issues, chronic pain, and inflammation.
Types of Ovarian Cysts in Endometriosis
Women with endometriosis may also get other ovarian cysts, like functional cysts. These cysts add to the pain and discomfort. Functional cysts are common and part of the menstrual cycle.
Pathological ovarian cysts, caused by abnormal cell growth, are less common but can happen in women with endometriosis. These cysts might be cancerous or not, and the risk of cancer goes up after menopause.
| Type of Ovarian Cyst | Description | Prevalence in Endometriosis |
|---|---|---|
| Endometriomas | Also known as “chocolate cysts,” these are filled with old, thick blood and are a hallmark of ovarian endometriosis. | Approximately 17 to 44% of women with endometriosis will develop an endometrioma. |
| Functional Cysts | These cysts develop as a normal part of the menstrual cycle and are the most common type of ovarian cysts. | Women with endometriosis may be more prone to developing functional cysts. |
| Pathological Cysts | These cysts form due to abnormal cell growth and can be cancerous or non-cancerous. | The risk of malignant ovarian cysts increases in women with endometriosis, specially after menopause. |
Endometriomas and other ovarian cysts in women with endometriosis can lead to fertility issues, chronic pain, and inflammation. Knowing about these cysts is key to managing and treating endometriosis effectively.
Diagnosing Ovarian Endometriosis
Finding ovarian endometriosis takes a detailed approach. This includes a pelvic exam, pelvic ultrasound, and sometimes laparoscopic surgery. The ultrasound can spot endometriomas, or “chocolate cysts,” which are key signs of ovarian endometriosis. But, only laparoscopic surgery can confirm it, by letting the surgeon see and biopsy any odd tissue.
To figure out if you have endometriosis, doctors use a few methods:
- Pelvic exam: Your doctor will feel your pelvic area to look for signs like cysts or scar tissue.
- Pelvic ultrasound: This test uses sound waves to show your pelvic organs. It can find endometriomas or other issues.
- Laparoscopy: This surgery lets your doctor see your organs up close and take a biopsy. It’s the best way to know for sure.
Using these tools, your doctor can find out if you have ovarian endometriosis. Then, they can plan the right treatment for you.

Risk Factors for Developing Endometriosis
Researchers have found several key risk factors for endometriosis. One major risk is family history of endometriosis. If a close female relative, like a mother or sister, has it, your risk goes up a lot.
Genetics also play a big part in endometriosis risk. The condition seems to run in families, with certain genes making you more likely to get it. Women with certain gene mutations or chromosomal issues are more at risk.
Other Endometriosis Risk Factors
Other factors can also raise your risk of endometriosis. These include:
- Early onset of menstruation (before age 12)
- Short menstrual cycles (27 days or fewer)
- Heavy, prolonged menstrual periods
- Never having given birth
- Certain physical characteristics, such as red hair, blue/green eyes, and freckles
- Immune system disorders and certain types of cancer
Some lifestyle choices might also affect your risk. For example, regular physical exercise and avoiding too much alcohol and caffeine might lower your risk.
Knowing these risk factors helps doctors better manage endometriosis. This can lead to better care and outcomes for those with this complex condition.
Endometriosis and Infertility
If you or your partner have been diagnosed with endometriosis, you might wonder how it affects your fertility. Endometriosis is a top reason for infertility in women. It happens when tissue like the lining of the uterus grows outside the uterus. This can make it hard for a sperm and egg to meet and implant.
Ovarian endometriosis can make it tough to get pregnant. It can press on the ovary, cause inflammation, and block the fallopian tubes. Treating endometriosis is key to improving fertility chances.
Studies show endometriosis is more common in women who can’t get pregnant. A 1987 study in The Journal of the Florida Medical Association found this. A 2004 study in Human Reproduction also showed differences in getting pregnant between women with and without endometriosis.
Many studies have looked at how endometriosis affects fertility. A 1993 study in Fertility and Sterility looked at this. Another study in 2004 in Fertility and Sterility examined IVF outcomes in women with endometriosis.
| Condition | Chance of Pregnancy per Month |
|---|---|
| No Endometriosis | 10-20% |
| Surgically Documented Endometriosis | 1-10% |
Endometriosis can affect fertility in many ways. It can change the immune system and hormone levels. It can also stop an embryo from implanting. If you’re dealing with infertility and endometriosis, talk to your doctor. They can help find the best treatment for you.

Treatment Options for Ovarian Endometriosis
If you’ve been diagnosed with ovarian endometriosis, there are several treatment options available. These options help manage your symptoms and address the underlying condition. The main treatments include hormonal therapy and surgical intervention.
Hormonal Therapy
Hormonal medications, like birth control pills or GnRH agonists, can help manage endometriosis symptoms. These treatments suppress or regulate hormones that contribute to the growth of endometriotic lesions. While they offer relief, they are not a cure, and symptoms may return after stopping treatment.
Surgical Treatment
For severe or persistent cases, surgical treatment is often needed. The most common method is laparoscopy. This involves a small camera to locate and remove endometriotic tissue. The goal is to remove affected tissue while keeping healthy ovarian tissue, to address chronic pain and improve fertility.
Choosing the right treatment plan is important. It depends on your individual needs. The decision to pursue a treatment option balances risks and quality of life impact.
Research on endometriosis is ongoing. Organizations like The Royal Women’s Hospital and the University of Melbourne are working to improve diagnosis and treatment options.
Managing Chronic Pelvic Pain
Chronic pelvic pain is a common problem for those with endometriosis. It can be tough to manage, but a mix of treatments can help. This includes medicine, physical therapy, and changes in lifestyle.
Medicines like aspirin or ibuprofen can ease the pain. Hormonal treatments can also help by controlling the menstrual cycle and reducing inflammation. If the pain is due to an infection, antibiotics might be needed.
Physical therapy, including pelvic floor therapy, can relax muscles and improve blood flow. This can help reduce pain. Acupuncture and trigger point injections may also offer relief for some.
Making lifestyle changes, like managing stress, is important too. Techniques like cognitive behavioral therapy and sex therapy can help with the emotional side of the condition. This can make the pain worse.
If the pain is severe or lasts a long time, a pain rehabilitation program might be needed. These programs use different treatments to help improve life quality.
It’s important to find the right mix of treatments and work with your healthcare provider. This way, you can manage chronic pelvic pain from endometriosis effectively.

Endometriosis and Ovarian Cancer Risk
Research has been ongoing to understand the link between endometriosis and ovarian cancer. Endometriosis is a chronic condition that causes pelvic pain and other symptoms. But, the risk of getting ovarian cancer is low for those with it.
Studies show women with endometriosis have more than 4 times the risk of ovarian cancer compared to those without it. Those with severe endometriosis, like deep infiltrating endometriosis and ovarian endometriomas, face a risk over 9 times higher.
Endometriosis is closely linked to certain ovarian cancers, like endometrioid and clear cell ovarian cancers. Women with endometriosis are 7.5 times more likely to get type I ovarian cancer. The risk is almost 19 times higher for those with severe endometriosis.
Even though these numbers seem scary, the actual risk of ovarian cancer from endometriosis is very low. It’s less than 1 in 10,000 cases. Regular check-ups with a healthcare provider are advised for those with endometriosis. But, most people with endometriosis do not develop ovarian cancer.
It’s important for those with endometriosis to know about the higher risk of ovarian cancer. But, it shouldn’t cause too much worry. By staying close to their healthcare providers and watching for health changes, people with endometriosis can manage their condition and lower their cancer risk.
Coping with Endometriosis and Ovarian Pain
Living with endometriosis and ovarian pain is tough. It affects both your body and mind. But, finding support and using resources can help manage it. Joining a support group, online or local, can connect you with others who get it.
Support Groups and Resources
Support groups are key for those with endometriosis. They provide a place to share, get advice, and feel less alone. Mental health experts also offer help with pain, fatigue, and the impact on your life.
- Try low-impact exercises like yoga, Pilates, or walking to manage pain and feel better.
- Look into alternative therapies like acupuncture, massage, or TENS to ease ovarian pain.
- Use stress management like meditation, deep breathing, or mindfulness to support your mental health.
- Eat a healthy, anti-inflammatory diet with lots of fruits, veggies, and whole grains to help symptoms.
Coping with endometriosis and ovarian pain is a journey. Finding the right mix of support, self-care, and medical help can greatly improve your life.

| Coping Strategies | Benefits |
|---|---|
| Support Groups | Provide a sense of community, emotional support, and shared experiences. |
| Mental Health Therapy | Help manage anxiety, depression, and the psychological impact of endometriosis. |
| Exercise and Alternative Therapies | Alleviate pain, improve physical and mental well-being. |
| Stress Management | Reduce the impact of stress on endometriosis symptoms and overall health. |
| Anti-Inflammatory Diet | Potentially ease symptoms and reduce inflammation. |
When to Seek Medical Attention
If you’re dealing with pelvic pain, heavy or irregular menstrual bleeding, painful intercourse, or trouble getting pregnant, see a doctor. These signs might point to endometriosis or other health issues.
Getting a diagnosis early and treating it can ease your symptoms, like ovarian pain. Talk to your healthcare provider about any health changes or concerns.
Some signs that mean you should visit the doctor include:
- Chronic or worsening pelvic pain that affects your daily life
- Abnormal menstrual bleeding, like heavy flow or irregular periods
- Painful intercourse or other pelvic discomfort
- Difficulty becoming pregnant or conceiving
Early treatment of endometriosis and related issues can greatly improve your life. Don’t wait to take care of your reproductive health.
| Symptom | Potential Cause | When to See a Doctor |
|---|---|---|
| Persistent or severe pelvic pain | Endometriosis, ovarian cysts, uterine fibroids | Seek medical attention if the pain is chronic or interferes with daily activities |
| Heavy or irregular menstrual bleeding | Endometriosis, uterine fibroids, hormonal imbalances | Consult a healthcare provider if bleeding is significantly heavier or more irregular than normal |
| Painful intercourse | Endometriosis, pelvic inflammatory disease, vaginal dryness | Discuss any persistent or worsening pain during sex with your doctor |
| Difficulty becoming pregnant | Endometriosis, polycystic ovary syndrome (PCOS), fallopian tube blockage | Seek evaluation if you have been trying to conceive for 12 months or more without success |
Early diagnosis and treatment of endometriosis and related conditions can greatly improve your quality of life. Don’t hesitate to advocate for your reproductive health and seek the care you deserve.
Endometriosis and Ovarian Health
If you have endometriosis, it affects your ovaries. Endometrial-like tissue can grow on or around your ovaries. This leads to cysts called endometriomas, or “chocolate cysts.”
These cysts can harm your ovarian tissue. This damage lowers your ovarian reserve and function. It makes it harder to get pregnant.
Endometriosis can also hurt your fertility. The inflammation and scarring it causes make it tough to stay fertile. It’s key to manage your endometriosis well to keep your ovaries healthy.
Knowing how endometriosis affects your ovaries helps you and your doctor. You can create a treatment plan that helps your symptoms and keeps your fertility goals in mind. With the right care, you can protect your ovarian function and stay fertile, even with this condition.
Source Links
- https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656
- https://endohealth.com.au/endometriosis/ovary/
- https://my.clevelandclinic.org/health/diseases/10857-endometriosis
- https://www.who.int/news-room/fact-sheets/detail/endometriosis
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/endometriosis
- https://www.ncbi.nlm.nih.gov/books/NBK567777/
- https://my.clevelandclinic.org/health/symptoms/24726-ovary-pain
- https://www.webmd.com/women/ovarian-pain-causes-diagnosis-treatments
- https://ocrahope.org/news/5-possible-causes-for-ovary-pain/
- https://www.ncbi.nlm.nih.gov/books/NBK559230/
- https://www.nhs.uk/conditions/ovarian-cyst/
- https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661
- https://www.verywellhealth.com/ovary-pain-causes-and-treatment-514437
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4114145/
- https://www.womenshealth.gov/a-z-topics/endometriosis
- https://www.webmd.com/women/endometriosis/endometriosis-causes-symptoms-treatment
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3538128/
- https://www.massgeneral.org/obgyn/fertility/news/endometriosis-and-its-impact-on-fertility
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2941592/
- https://www.thewomens.org.au/health-information/periods/endometriosis/treating-endometriosis
- https://www.brighamandwomens.org/obgyn/infertility-reproductive-surgery/endometriosis/endometriosis-pain-management-for-adult-women
- https://www.ncbi.nlm.nih.gov/books/NBK554585/
- https://www.mayoclinic.org/diseases-conditions/chronic-pelvic-pain/symptoms-causes/syc-20354368
- https://www.mayoclinic.org/diseases-conditions/chronic-pelvic-pain/diagnosis-treatment/drc-20354371
- https://www.nih.gov/news-events/nih-research-matters/endometriosis-types-ovarian-cancer-risk
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5563086/
- https://www.cancer.org/cancer/latest-news/endometriosis-may-increase-ovarian-cancer-risk.html
- https://www.webmd.com/women/endometriosis/ss/slideshow-unexpected-ways-to-ease-endometriosis-pain
- https://drseckin.com/what-are-endo-attacks-and-how-to-cope-with-them/
- https://unmhealth.org/stories/2023/02/ovarian-cysts-what-to-know-when-tosee-doctor.html
- https://www.mayoclinic.org/diseases-conditions/ovarian-cysts/symptoms-causes/syc-20353405
- https://www.healthline.com/health/womens-health/what-does-ovarian-cyst-pain-feel-like