Are you tired of feeling like your period cramps are unbearable? You might be dealing with endometriosis, a condition that affects many women. It’s important to understand why your cramps are so painful to find relief.
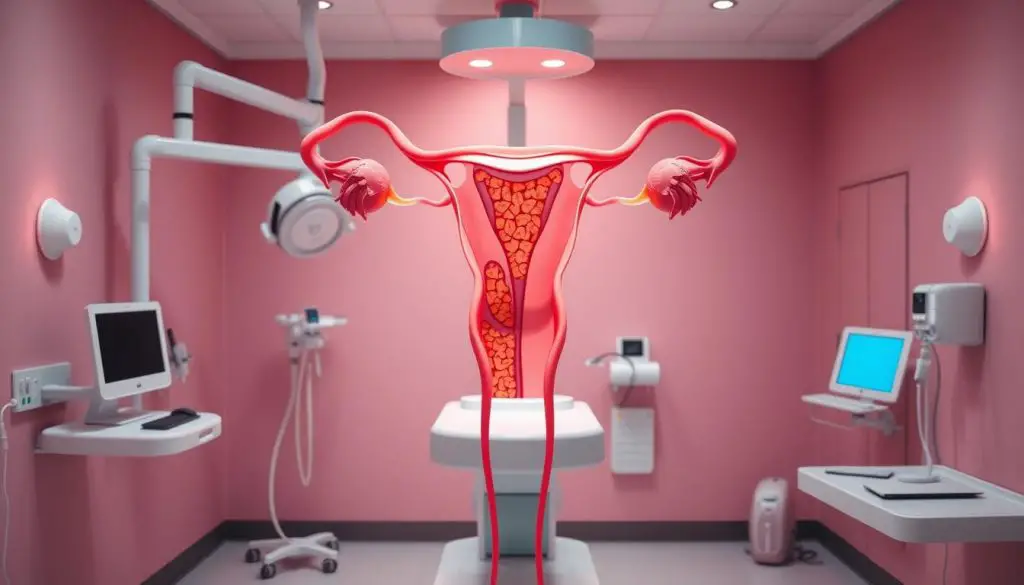
Endometriosis happens when tissue like the uterine lining grows outside the uterus. This tissue can grow on the ovaries, fallopian tubes, and other pelvic areas. When it responds to hormones, it causes inflammation, scarring, and adhesions.
These adhesions lead to severe pelvic pain and cramping. The pain is often worse than what most women experience during their periods.
Understanding Endometriosis: A Debilitating Condition
Endometriosis is a chronic and often debilitating condition. It affects about 10% (190 million) of women and girls of reproductive age worldwide. This condition happens when the endometrium, the tissue inside the uterus, grows outside the uterus. It can grow on other pelvic organs like the ovaries, fallopian tubes, and the outer surface of the uterus.
What is endometriosis?
During the menstrual cycle, this misplaced endometrial tissue thickens, breaks down, and bleeds. This is similar to what happens inside the uterus. But, this tissue can’t leave the body. It leads to inflammation, scarring, and adhesions. These can cause severe pain and other complications.
Risk factors and causes
The exact cause of endometriosis is not fully understood. But, some risk factors include genetic predisposition, early menstruation, and conditions that prevent menstrual blood flow. Studies also show it’s linked to heart disease and metabolic changes. This challenges old misconceptions about the condition.
Endometriosis is a complex and often misunderstood condition. It can have a big impact on a person’s health and quality of life. Knowing about this chronic disease and its causes is key. It helps in seeking the right medical care and managing symptoms.
Painful Periods: A Hallmark Symptom
Endometriosis often brings painful periods, or dysmenorrhea. Women with endometriosis face pain that’s worse than usual cramps. This pain can stop them from working, going to school, or doing everyday tasks.
The severe menstrual cramps endometriosis can start days before the period and last all month. This pain happens because tissue outside the uterus reacts to hormones and sheds, but can’t leave the body.
Studies show dysmenorrhea affects 50% to 90% of girls and women. About 70% of teens with this pain have endometriosis, found through laparoscopy.
Genetic factors, stress, and depression can increase the risk of endometriosis painful periods. Other factors include early menarche, long or heavy periods, smoking, and a family history of dysmenorrhea.
Managing endometriosis period pain is tough, but there are ways to help. Over-the-counter pain relievers, heat therapy, exercise, a healthy diet, and stress reduction can help. Sometimes, prescription meds or alternative therapies are needed. Getting medical help and support is key for those with severe menstrual pain.
Beyond Cramps: Other Endometriosis Symptoms
Painful periods are a key sign of endometriosis. But, this condition can also cause many other painful symptoms. The misplaced endometrial tissue can lead to chronic pelvic pain, not just during menstruation.
Another symptom is painful intercourse, or dyspareunia. This happens because of the endometrial implants in the pelvic area. These implants can get irritated during sex.
Endometriosis can also cause ovarian cysts, known as endometriomas. These cysts can be painful and affect fertility. Many women with endometriosis struggle with infertility because the condition can harm the fallopian tubes and affect egg quality.
| Endometriosis Symptom | Impact |
|---|---|
| Chronic pelvic pain | Severe, debilitating pain not just during menstruation, caused by inflammation and scarring from misplaced endometrial tissue |
| Painful intercourse | Pain during sexual activity due to endometrial implants in the pelvic area |
| Ovarian cysts | Painful endometriomas that can contribute to infertility |
| Infertility | Endometriosis can damage the fallopian tubes and affect egg quality, making it difficult to conceive |
While painful periods are a hallmark of endometriosis, this condition can have a far-reaching impact on a person’s quality of life. Understanding the full range of endometriosis symptoms, including chronic pelvic pain, painful intercourse, ovarian cysts, and infertility, is key. It’s important for seeking the right medical care and managing this complex condition.
Differentiating Endometriosis from Normal Period Pain
Many women feel some discomfort during their periods. But, endometriosis pain is usually much worse. Knowing the difference is key to getting the right treatment and managing it well.
Pattern and Severity of Pain
Endometriosis pain starts a few days before the period and lasts all cycle. Normal period cramps are usually more bearable and happen only during bleeding days. Endometriosis pain is so bad it can stop a woman from working, going to school, or doing everyday things. Normal cramps, while uncomfortable, shouldn’t stop you from living your life.
Impact on Daily Activities
Endometriosis pain is much more than just discomfort. It can make it hard for women to go to work, school, or even do simple tasks. Regular menstrual cramps are annoying but shouldn’t get in the way of your daily life.
| Characteristic | Endometriosis | Normal Period Pain |
|---|---|---|
| Timing of Pain | Starts several days before period, lasts throughout cycle | Concentrated around days of bleeding |
| Severity of Pain | Severe, debilitating, disrupts daily life | Uncomfortable, but does not significantly interfere with daily activities |
| Impact on Daily Life | Causes missed work/school, cancelled plans, difficulty completing tasks | Should not significantly impact normal daily routine |

It’s important to know the difference between endometriosis and regular period pain. If you’re experiencing severe or persistent symptoms, see a doctor. They can help you get the right treatment and manage your condition.
Painful Periods Cramps: When to Seek Medical Attention
Period cramps are normal for many women. But if yours are severe and much more painful than usual, you should see a doctor. If these cramps stop you from doing daily activities, work, or school, it might be a sign of endometriosis or another issue.
If you’re worried about your abnormal period pain, don’t wait. Make an appointment with your gynecologist or a specialist. Early treatment can greatly improve your life.
Here are some signs you should see a doctor for when to see a doctor for period cramps:
- Menstrual cramps that disrupt your daily activities every month
- Symptoms that worsen progressively over time
- Severe cramps appearing for the first time after age 25
Your doctor will look at your pain level, cycle length, blood flow, and other symptoms. They’ll check if your cramps might be from severe period cramps endometriosis. They might suggest hormonal birth control, medication, or surgery, based on your situation.
Don’t suffer through bad period cramps. If they’re really affecting your life, get medical help. You deserve to find relief and manage your condition.
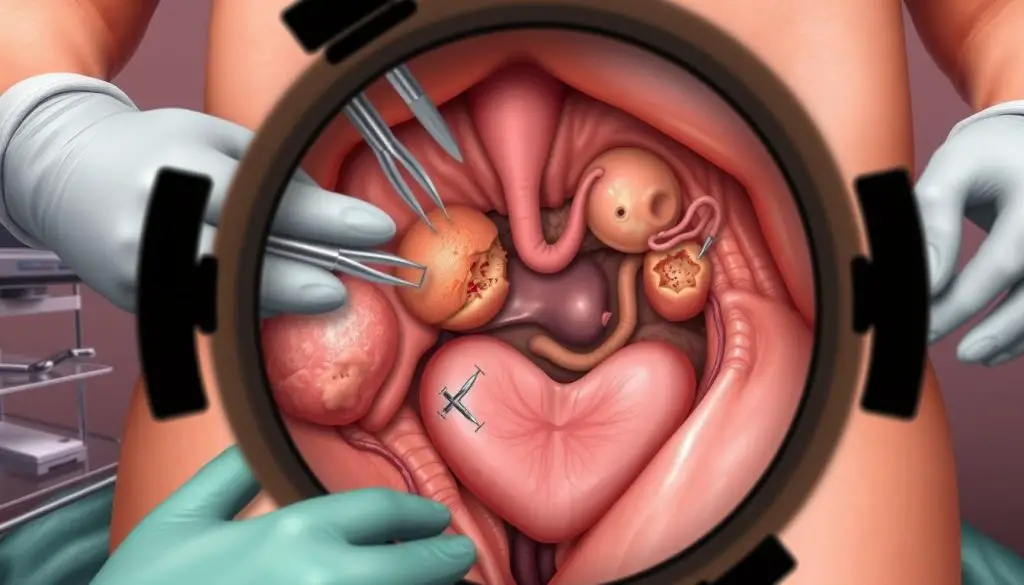
Diagnosing Endometriosis: Laparoscopy and Imaging Tests
Finding endometriosis can be tricky because its symptoms are similar to other gynecological issues. The first steps usually include a pelvic exam and imaging tests like ultrasound or MRI. These can spot endometrial implants or cysts. But, the only sure way to find endometriosis is through laparoscopy, a surgical method.
Pelvic Exam and Ultrasound
Your doctor will check your reproductive organs during a pelvic exam for signs of endometrial tissue. A transvaginal ultrasound uses sound waves to show images of the pelvic area. It can spot endometrial implants or cysts linked to endometriosis.
MRI and Blood Tests
MRI scans give detailed views of the pelvis, showing endometrial tissue growth. Blood tests, like the CA-125 test, offer more clues. Yet, they alone can’t confirm diagnosing endometriosis.
Laparoscopic Surgery
The only sure way to diagnose endometriosis is through laparoscopy. This surgery uses a small camera through a tiny cut in the abdomen. It lets doctors see the pelvic organs and find endometrial tissue. A biopsy might also be taken to make the diagnosis clear.
| Diagnostic Test | Purpose |
|---|---|
| Pelvic Exam | Physical examination of reproductive organs for signs of endometrial tissue growth |
| Transvaginal Ultrasound | Imaging technique using sound waves to detect endometrial implants or cysts |
| MRI | Detailed imaging of the pelvis to reveal areas of endometrial tissue growth |
| CA-125 Blood Test | Provides additional information but not definitive for endometriosis diagnosis |
| Laparoscopy | Minimally invasive surgical procedure to directly visualize and confirm endometriosis |
Managing Endometriosis: Treatment Options
If you’ve been diagnosed with endometriosis, you might wonder about treatment options. The main goals are to manage symptoms, stop the condition from getting worse, and keep fertility if you want. Your doctor will create a plan just for you, based on your symptoms, fertility goals, and health.
Pain Medications and Hormone Therapy
For mild to moderate endometriosis, your doctor might suggest pain medications like NSAIDs. These help with cramps and pelvic pain. Hormone therapy, like birth control pills or patches, can also help by controlling hormone levels and stopping endometrial growth.
Surgical Intervention
For severe cases or when meds don’t work, surgery might be needed. Laparoscopic surgery is often used to remove implants, adhesions, and cysts. Sometimes, removing the uterus or ovaries is necessary, mainly for women who don’t plan to have more kids.
It’s key to work closely with your doctor to find the best endometriosis treatment options for you. You can discuss medications for endometriosis and endometriosis surgery to manage symptoms and improve your life.
Endometriosis and Fertility Challenges
Endometriosis is a chronic condition that can greatly affect a woman’s ability to get pregnant. Studies show that 25-50% of women with infertility also have endometriosis according to research. The misplaced tissue in endometriosis can lead to scarring and damage to the reproductive organs.
This damage can lower egg quality and block the fallopian tubes. It makes it hard for the egg to be fertilized or to implant in the uterus.
Women with endometriosis might need help getting pregnant, like IVF. Getting diagnosed early and starting the right treatment is key to keeping fertility and boosting pregnancy chances.
- About 5 million American women suffer from endometriosis, which accounts for roughly three percent of the female population.
- Endometriosis can lead to infertility, with scarring potentially causing difficulties in becoming pregnant.
- An estimated 6.5 million women in the United States, which accounts for about one in 10 women, are affected by endometriosis.
- Approximately one in two women dealing with infertility may have endometriosis.
If you have ongoing or severe menstrual pain, see a doctor. It could mean you have endometriosis. Early treatment can help manage the condition and boost your chances of getting pregnant.

Coping with Endometriosis: Support and Self-Care
Living with endometriosis can be tough on your body and mind. But, there are ways to cope and improve your life. Self-care and support groups can help manage the condition.
Using pain meds like ibuprofen can ease cramps and discomfort. Heat from a pad or a warm bath can also help. Relaxation techniques, such as deep breathing or yoga, can reduce stress and pain.
Staying active and eating well is key to managing symptoms. Research shows that exercise can lessen pain and boost mood. Eating foods that fight inflammation, like fish and berries, can also help.
Being part of a support group is very helpful. These groups offer a place to share and find support. Mental health services, like therapy, can also help with the emotional side of endometriosis.
Every person’s journey with endometriosis is unique. Finding the right self-care and support can greatly improve your life.
Seeking Specialized Care for Endometriosis
If you’re dealing with the tough symptoms of endometriosis, finding the right doctor is key. Endometriosis specialists, like gynecologists or reproductive endocrinologists, know the latest ways to diagnose and treat it.
These experts will help you create a plan that covers both your physical and emotional health. They can guide you in finding the best doctor and treatment centers for endometriosis.
It’s okay to ask for a second opinion if you’re not feeling heard. With the right care, you can manage your endometriosis and live better.
| Key Reasons to Seek Specialized Care for Endometriosis |
|---|
|
You deserve to find relief from endometriosis symptoms. By finding the right endometriosis specialists, you’re taking a big step towards better health.
The Impact of Endometriosis on Quality of Life
Endometriosis is a chronic and debilitating condition that deeply affects a woman’s quality of life. It causes severe physical symptoms and impacts her emotional, social, and mental well-being. Studies have shown that it significantly impairs her health-related quality of life. This makes it hard for her to work, attend school, maintain relationships, and do daily activities.
The hallmark symptom of endometriosis – pelvic pain – can be so severe. It interferes with a woman’s daily routine. In fact, 92.5% of women with moderate-to-severe endometriosis-associated pain reported experiencing pelvic pain. Other symptoms like dyspareunia (painful intercourse) and heavy bleeding add to the physical and emotional toll.
The impact of endometriosis goes beyond physical symptoms. It leads to decreased mental health, increased anxiety, and feelings of isolation. The chronic nature of the condition and lack of understanding from others make it hard for women to cope. This negatively affects their overall quality of life.
To improve the quality of life for women with endometriosis, we need to address all aspects of the condition. This includes physical symptoms, emotional well-being, and social impact. By raising awareness, advocating for better healthcare, and empowering women to manage their symptoms, we can work towards a future. A future where endometriosis no longer robs women of their quality of life.
Raising Awareness: Endometriosis Is Not Just Painful Periods
Endometriosis is more than just bad menstrual cramps. It affects about 1 in 10 women globally. Symptoms include chronic pelvic pain, painful sex, and infertility.
Many women are not taken seriously when they talk about their pain. People often say it’s just part of being a woman. This can lead to delayed diagnosis, with some women waiting up to 10 years for a correct diagnosis.
It’s important to understand endometriosis fully. This includes its complex symptoms, not just period pain. By educating everyone, we can help women get the care they deserve. This way, we can improve their lives and reduce the disease’s impact.
Source Links
- https://www.hopkinsmedicine.org/health/wellness-and-prevention/period-pain-could-it-be-endometriosis
- https://www.topdoctors.co.uk/medical-articles/know-difference-between-regular-period-pain-endometriosis
- https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656
- https://www.who.int/news-room/fact-sheets/detail/endometriosis
- https://www.webmd.com/women/endometriosis/understanding-endometriosis-symptoms
- https://www.endofound.org/painful-periods
- https://en.wikipedia.org/wiki/Dysmenorrhea
- https://www.everydayhealth.com/treatment/womens-health/ways-to-relieve-period-cramps/
- https://www.toplinemd.com/jaime-a-mercado-md/dysmenorrhea-a-complete-guide-to-painful-menstruation-for-women/
- https://nyulangone.org/news/endometriosis-six-symptoms-you-should-never-ignore
- https://www.ohsu.edu/womens-health/severe-menstrual-pain-not-normal
- https://www.womenshealthofaugusta.com/when-its-not-just-cramps-uncommon-symptoms-of-endometriosis/
- https://www.obgynassociatesmarietta.com/blog/normal-menstrual-cramps-or-endometriosis-how-to-tell-the-difference
- https://www.orlandohealth.com/services-and-specialties/orlando-health-womens-institute/content-hub/learn-the-difference-between-painful-periods-endometriosis-and-ibs/
- https://www.drtahery.com/endometriosis-vs-menstrual-cramps-whats-the-difference
- https://www.mayoclinic.org/diseases-conditions/menstrual-cramps/symptoms-causes/syc-20374938
- https://www.healthpartners.com/blog/when-to-see-a-doctor-for-menstrual-cramps/
- https://my.clevelandclinic.org/health/diseases/10857-endometriosis
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/endometriosis
- https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661
- https://www.medicalnewstoday.com/articles/321402
- https://www.webmd.com/women/endometriosis/ss/slideshow-unexpected-ways-to-ease-endometriosis-pain
- https://parkavefertility.com/infertility-causes/endometriosis/
- https://atriumhealth.org/dailydose/2024/03/05/story-about-endometriosis
- https://www.cloudninefertility.com/blog/painful-periods-exposed-how-menstrual-cramps-can-be-a-clue-to-infertility
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4568158/
- https://www.sylacaugaobgyn.com/how-to-cope-with-endometriosis-self-care-strategies-for-thriving/
- https://www.thewomens.org.au/health-information/periods/endometriosis/treating-endometriosis
- https://uvahealth.com/services/womens-health/endometriosis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8780646/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10241351/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7561574/
- https://academic.oup.com/humupd/article/19/6/625/839568
- https://uthealthaustin.org/blog/endometriosis-is-not-just-painful-periods
- https://unric.org/en/lets-stop-normalizing-painful-periods/
