Imagine having menstrual cramps so bad they stop you from working or doing everyday things. If this sounds like you, you might have endometriosis. This condition causes severe pain during your period. Understanding endometriosis can help you find relief and take back control of your health.
Endometriosis is a complex condition that affects many women worldwide. It happens when cells like the uterine lining grow outside the uterus. These cells can attach to other organs in the pelvic area, causing inflammation and scarring. This leads to extremely painful period cramps and other symptoms that can really affect your life.
Understanding Endometriosis: A Condition Beyond Painful Periods
Endometriosis is a complex condition that affects about 10% of women of reproductive age. It’s more than just painful periods. To really understand it, we need to know its causes and how it works.
What is Endometriosis and How Does It Cause Severe Menstrual Cramps?
Endometriosis happens when tissue like the uterine lining grows outside the uterus. This tissue can grow on ovaries, fallopian tubes, or other pelvic areas. When it builds up and breaks down during the menstrual cycle, it causes bleeding inside the body.
This bleeding leads to inflammatory response, causing pain and swelling. The scarring in the pelvic area is what makes menstrual cramps so severe for those with endometriosis.
The menstrual cycle and endometriosis are closely tied. Hormonal changes that control the uterine lining also affect the misplaced tissue. This cycle can cause a range of endometriosis symptoms, including painful periods and chronic lower back pain.
The exact causes of endometriosis are not known. But research points to genetic factors, immune system issues, and retrograde menstruation as possible causes. These factors can lead to endometrial tissue growth and pelvic inflammatory response, making symptoms worse.
The Hallmark Symptoms: Recognizing the Signs of Endometriosis
Knowing the symptoms of endometriosis is key to getting the right care. This condition has signs that can really affect a woman’s life. By learning about these symptoms, you can start managing this tough disorder.
Extremely painful period cramps are a big sign of endometriosis. These cramps can be so bad they stop you from doing daily things. Pelvic pain that lasts all month is another sign, feeling like a dull ache or sharp pain.
Endometriosis also causes painful intercourse, or dyspareunia. This makes sex hard and can hurt your feelings. Ovarian cysts, or endometriomas, are common too and add to pelvic pain.
| Endometriosis Symptom | Prevalence |
|---|---|
| Painful periods (dysmenorrhea) | 75-90% of women with endometriosis |
| Chronic pelvic pain | 70-90% of women with endometriosis |
| Painful intercourse (dyspareunia) | 50-90% of women with endometriosis |
| Ovarian cysts (endometriomas) | 17-44% of women with endometriosis |
| Infertility | 30-50% of women with endometriosis |
Not every woman with endometriosis has the same symptoms. But, knowing these signs and seeing a doctor fast can help manage it.
It’s vital to listen to your body and watch for any changes or pain. If you notice these symptoms, see a doctor who knows about endometriosis. They can help figure out what’s going on and how to treat it.
Extremely Painful Period Cramps: A Red Flag for Endometriosis
If your period pain is so bad it stops you from doing daily things, it might be endometriosis. Some pain during your period is okay, but really bad period cramps are not. They should stop you from working, going to school, or doing normal stuff. You should see a gynecologist about this.
Endometriosis is when tissue like the uterine lining grows outside the uterus. It can be on the ovaries, fallopian tubes, and even the bladder or intestines. This tissue thickens, breaks down, and bleeds with each period. But it can’t leave the body, causing inflammation, scarring, and adhesions. These can lead to extremely painful period cramps and other symptoms.
If you have painful menstruation due to endometriosis, you need to see a doctor. Your doctor can check your symptoms, do tests, and create a treatment plan. This plan will help with your excessive menstrual cramps and other endometriosis problems. Don’t wait until the period pain impacts your daily life too much. Act now to get the help and care you need.
When period pain interferes with daily activities, it’s time to seek medical attention.
About 1 in 10 people who menstruate have endometriosis, and it’s a big reason for infertility. If you have severe period cramps that mess up your life, talk to your gynecologist. With the right diagnosis and treatment, you can control your endometriosis symptoms and take back your health.
Chronic Pelvic Pain: More Than Just Menstrual Discomfort
Endometriosis causes more than just period pain. Many people with this condition also deal with chronic pelvic pain. This pain is due to inflammation and scarring from misplaced endometrial tissue outside the uterus.
The pelvic floor, which supports the bladder, bowel, and reproductive organs, can be affected by endometriosis. This leads to ongoing pain, muscle spasms, and discomfort. The pain can even spread to the legs or back. This mix of endometriosis-related pelvic pain and pelvic floor dysfunction makes the pain worse.
Chronic pelvic pain is more than just a nuisance. It can make daily life hard, causing missed work and a lower quality of life. Knowing how endometriosis and chronic pelvic pain are linked is key. It helps find the right treatments to ease this painful symptom.
| Condition | Prevalence |
|---|---|
| Chronic Pelvic Pain | Affects 1 in 7 women in the United States |
| Endometriosis | Estimated to occur in 4-16% of women |
| Endometriosis and Chronic Pelvic Pain | Almost 50% of women with endometriosis suffer from chronic pelvic pain |
Healthcare providers can tackle the connection between endometriosis and pelvic floor issues. This way, they can manage chronic pelvic pain better. It helps improve the lives of those with this tough condition.

Endometriosis and Dyspareunia: The Link Between Painful Intercourse and Pelvic Pain
Painful intercourse, or dyspareunia, is a lesser-known symptom of endometriosis. It happens because of inflammation and scar tissue from misplaced endometrial tissue. This pain is so severe that many people with endometriosis avoid sex altogether.
The pain from dyspareunia can be sharp in certain areas or spread throughout the pelvis. It affects a person’s sexual function and overall life quality. Research shows that painful sex is a top symptom, showing the need for better awareness and treatment.
It’s important to address endometriosis-related sexual dysfunction because it can cause emotional pain and strain relationships. Talking openly with doctors and partners is key. It helps find new ways to be intimate and find relief.
Managing pelvic pain during intercourse due to endometriosis is challenging but not impossible. There are many treatments and strategies available. A plan made just for you can help you feel in control and improve your sexual health.
By focusing on the link between endometriosis and painful sex, we can help more people. Healthcare providers and the endometriosis community can work together. Together, we can help people get the support and care they need. With understanding and the right solutions, managing dyspareunia can be a big step in managing endometriosis.
Ovarian Cysts and Endometriosis: A Complicated Relationship
Endometriosis affects about 10% of women worldwide. It often leads to the growth of ovarian cysts, called endometriomas. These cysts form when endometrial tissue grows on the ovaries. Knowing how endometriosis and these cysts are linked is key. They can cause pelvic pain and other symptoms in those with endometriosis.
Endometriomas: A Common Complication of Endometriosis
Between 17 to 44% of women with endometriosis will get an endometrioma. About 28% will have cysts on both ovaries. Also, 17% of women trying to get pregnant will have endometriomas. These cysts can grow big and hurt, needing surgery to fix.
| Statistic | Percentage |
|---|---|
| Women with endometriosis who will experience an endometrioma | 17% to 44% |
| Women with endometriosis who will have bilateral endometriomas | 28% |
| Women in the subfertility population found to have endometriomas | 17% |

The growth of endometriomas is similar to endometriosis. It involves hormonal changes, inflammation, and tissue growth. These cysts can make pelvic pain, heavy periods, and irregular cycles worse. Treating both endometriosis and endometriosis-related ovarian cysts is vital for better health.
The Silent Struggle: Endometriosis and Infertility
Women with endometriosis face a tough journey to conceive. This condition, where tissue grows outside the uterus, affects 25-50% of women trying to get pregnant. It can harm the reproductive organs, making it hard to get pregnant.
Studies show endometriosis impacts fertility in many ways. A study by Verkauf BS found differences in symptoms between fertile and infertile women. Hughes EG et al. highlighted the challenges of conceiving with endometriosis. Akande VA et al. found that women with minor endometriosis take longer to conceive than those with unexplained infertility.
Brosens I looked at how endometriosis affects IVF success. Giudice LC and Kao LC discussed the condition’s prevalence and fertility impact. Taylor HS and Bagot C found genetic factors in endometriosis, affecting fertility.
For those with endometriosis, getting pregnant is hard. But, early treatment, like excision surgery, can help. Getting support from healthcare and understanding partners is also key.
| Key Endometriosis-Related Infertility Statistics | Findings |
|---|---|
| Incidence of endometriosis in infertile women | 25-50% |
| Relationship between endometriosis and IVF outcomes | Potential difficulties in achieving successful fertility treatments |
| Unexplained infertility vs. minor endometriosis | Differences in time to natural conception |
| Asymptomatic endometriosis in infertile women | 20-25% of cases |
| Endometriosis as a symptom of infertility | 6th fundamental symptom, according to the Endometriosis Foundation of America |
Endometriosis-related infertility is a big challenge for many women. Understanding its impact and seeking early medical help can help. With support and healthcare progress, starting a family becomes more possible for those with endometriosis and infertility.
Diagnostic Approaches: Confirming the Presence of Endometriosis
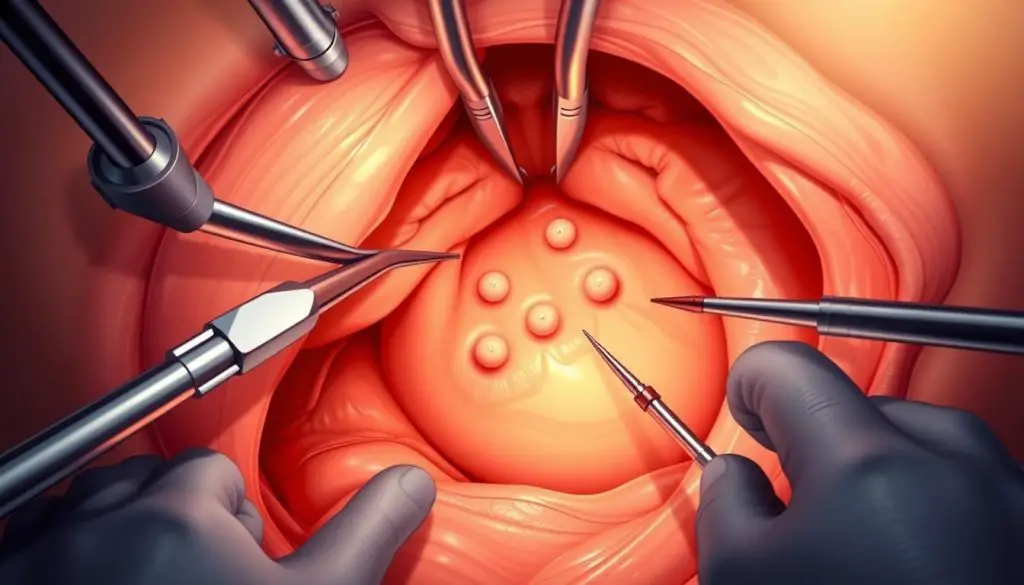
Endometriosis is a complex condition that can only be definitively diagnosed through a surgical procedure called laparoscopy. This minimally invasive procedure allows surgeons to visually inspect the pelvic organs and identify any endometrial-like tissue growth. During the laparoscopy, a small sample of the tissue may also be removed and examined under a microscope to confirm the presence of endometriosis.
Laparoscopy is considered the gold standard for diagnosing endometriosis, as it enables both the identification and potentially the treatment of the condition. The procedure involves making small incisions in the abdomen and inserting a thin, lighted camera to assess the extent and location of the endometrial implants.
Laparoscopic Diagnosis of Endometriosis
Endometriosis can manifest in various ways, and laparoscopy allows the surgeon to recognize different types of lesions, including:
- Peritoneal implants – Endometrial-like tissue growing on the lining of the pelvic cavity
- Peritoneal windows – Areas where the peritoneum appears thinned or perforated
- Endometriomas – Cysts filled with old blood, also known as “chocolate cysts”
- Deep infiltrating nodules – Endometrial tissue that has penetrated deeply into the pelvic organs or surrounding structures
The laparoscopic diagnosis of endometriosis can be further complemented by other diagnostic tests, such as magnetic resonance imaging (MRI) or ultrasound, to provide a complete assessment of the condition.
While laparoscopy is considered the gold standard for diagnosing endometriosis, it’s important to note that the condition can also be present in women with normal pelvic examinations. In such cases, a high index of suspicion and a thorough diagnostic workup are essential to confirm the presence of endometriosis and provide appropriate treatment.
Treatment Options: Managing Endometriosis and Alleviating Symptoms
If you’re dealing with endometriosis pain, you’re not alone. There are many ways to manage your symptoms and improve your life. First, your doctor might suggest pain meds like ibuprofen. They might also recommend hormone therapy to control estrogen and progesterone levels.
Studies show that 80 to 90% of endometriosis patients also have adenomyosis. This condition makes the endometrial tissue grow into the uterine muscle. While most endometriosis is not visible on tests, some cases can be seen on ultrasound or MRI if it grows into organs.
If these treatments don’t work, surgery might be next. Laparoscopy is a minimally invasive surgery that can show how big and where the endometriosis is. It can treat the problem in one surgery. But, remember, endometriosis can come back, with about 20 out of 100 women seeing regrowth within five years.
If surgery doesn’t help, or if you want more ways to manage your symptoms, there are other options. You can try:
- Hormonal Therapy: Medications like progestins and LNG-IUS can help with pain and symptoms after surgery, sometimes better than surgery alone.
- Lifestyle Modifications: Changing your diet, exercise, and stress management can also help with pain.
- Pain Management: Over-the-counter pain relievers like ibuprofen or naproxen sodium can help with menstrual cramps.
The main goal of treating endometriosis is to reduce pain and improve your life. Work with your doctor to find the best treatments for you.
Hormonal Therapy: Regulating the Menstrual Cycle for Relief
If you’re dealing with endometriosis, hormonal therapy could change your life. Birth control pills and GnRH agonists and antagonists can help. They stop your menstrual cycle and control estrogen and progesterone levels.
This method can reduce the growth of endometrial tissue. It also lowers inflammation and pain. Hormonal therapy is often the first treatment for endometriosis. It helps manage symptoms and control your menstrual cycle.
The hormonal treatment for endometriosis makes your body act like it’s in menopause. This helps the endometrial tissue shrink and pain decrease. Birth control for endometriosis and GnRH agonists and antagonists for endometriosis are common treatments. They help manage your menstrual cycle and endometriosis symptoms.
| Medication | Mechanism of Action | Effectiveness |
|---|---|---|
| Combined Oral Contraceptives | Suppress ovulation and thin the endometrium | Effective in reducing pain and preventing disease progression |
| Progestin-only Pills | Thin the endometrium and inhibit ovulation | Can be effective in managing endometriosis symptoms |
| GnRH Agonists and Antagonists | Suppresses the production of estrogen and progesterone | Highly effective in reducing pain and shrinking endometrial lesions |
Finding the right hormonal therapy might take some time. But with your healthcare provider’s help, you can find a treatment that works for you. This way, you can manage your endometriosis and live a more comfortable life.

Surgical Intervention: When Conservative Treatments Fail
If treatments like medications and lifestyle changes don’t help, surgery might be needed. The most common surgery is a laparoscopic procedure. This uses a tiny camera and tools to remove misplaced endometrial tissue through an endometriosis excision surgery.
This minimally invasive endometriosis treatment can ease pain, improve fertility, and stop endometriosis from coming back. It’s less invasive than other methods, leading to faster recovery, less pain, and fewer complications.
Exploring Surgical Options for Endometriosis
The goal of endometriosis surgery is to remove all visible endometriosis lesions and adhesions. This laparoscopic endometriosis removal is the best way to treat endometriosis and give long-term pain relief. A skilled surgeon is key to success, as most gynecologists don’t get enough training in endometriosis management.
| Surgical Approach | Description | Potential Benefits |
|---|---|---|
| Laparoscopic Excision | The surgeon uses specialized tools to carefully cut out and remove all visible endometriosis lesions. |
|
| Laparoscopic Ablation | The surgeon uses heat or energy to destroy the endometriosis lesions on the surface. |
|
Choosing the right endometriosis surgery options is critical for success. While ablation is quicker, excision surgery is more effective in removing tissue and reducing recurrence risk.
Working with an experienced endometriosis specialist is important for the best results. With the right surgery and care, you can find relief from endometriosis symptoms.
Lifestyle Modifications: Complementary Approaches to Endometriosis Management
Living with endometriosis can be tough. But, there are many lifestyle changes and therapies that help. These natural remedies and changes can support medical treatments in managing the condition.
Natural Remedies for Endometriosis
One great natural remedy is using anti-inflammatory medications like ibuprofen. They help reduce inflammation and ease pain. Applying heat to the lower abdomen also helps by improving blood flow and relaxing muscles.
Dietary Changes for Endometriosis
Making dietary changes can help manage symptoms. Eating foods rich in omega-3 fatty acids, like fatty fish and walnuts, may slow endometriosis growth. Some people find a gluten-free diet helps too.
Physical Activity and Endometriosis
Regular exercise is also helpful. Activities like yoga and Pilates can boost endorphins, easing pain and improving mood.
Stress-Reducing Techniques
Endometriosis affects mental health too. Stress-reducing techniques, like meditation, can help manage anxiety and depression. They offer emotional support.
While these therapies and lifestyle changes don’t cure endometriosis, they offer valuable support. It’s important to work with healthcare professionals to create a treatment plan. This plan should include both medical and natural approaches to manage the condition.
Endometriosis and Mental Health: Addressing the Emotional Impact
The chronic pain and infertility linked to endometriosis can deeply affect mental health. Women with endometriosis often face higher rates of endometriosis and depression and endometriosis and anxiety. This is true, even more so during their menstrual periods. The emotional toll of endometriosis can be overwhelming.
Getting a diagnosis can be hard, and managing symptoms is a constant struggle. These challenges add to the emotional burden. It’s important to seek mental health support for endometriosis.
Healthcare providers should work with mental health professionals. This approach helps patients find ways to cope and access needed resources. It’s a step towards managing the emotional challenges of endometriosis.
Having a strong support network is also key. Whether it’s through patient communities or loved ones, sharing experiences can help. It reduces feelings of isolation and offers a sense of community.
Remember, you’re not alone in this journey. By addressing the mental health impact of endometriosis and seeking support, you can improve your quality of life. It’s a step towards holistic healing.
| Statistic | Relevance |
|---|---|
| Women with endometriosis are at increased risk of developing major depression and anxiety disorders, as shown in a longitudinal follow-up study. | Highlights the strong link between endometriosis and mental health conditions like depression and anxiety. |
| Chronic pelvic pain in endometriosis is associated with mental disorders, sexual dysfunctions, and childhood maltreatment. | Demonstrates the complex interplay between physical symptoms, mental health, and life experiences in endometriosis. |
| Endometriosis significantly impacts the quality of life and mental health of patients, with pelvic pain being a differentiating factor. | Highlights the significant burden of endometriosis on overall well-being and the importance of addressing both physical and mental health aspects. |
Seeking Support: Finding a Community for Endometriosis Warriors
Living with endometriosis can feel very isolating. But, finding others who get it can change everything. Joining a support group, either in person or online, is a great way to share and learn. These groups are full of people who understand the challenges you face.
They offer a safe space to talk about treatments, coping, and how endometriosis affects your life. It helps you feel less alone. You can find comfort in knowing you’re not the only one going through this.
Online resources, like social media groups and forums, are key for connecting with others. They let you share experiences, get advice, and find support. By joining these communities, you can learn from others and feel supported.
Connecting with others who have endometriosis can be life-changing. Whether it’s in person or online, sharing your story and getting support is empowering. It gives you the strength to fight for your health and improve your life.
Source Links
- https://www.hopkinsmedicine.org/health/wellness-and-prevention/period-pain-could-it-be-endometriosis
- https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656
- https://www.webmd.com/women/endometriosis/understanding-endometriosis-symptoms
- https://www.topdoctors.co.uk/medical-articles/know-difference-between-regular-period-pain-endometriosis
- https://www.uptodate.com/contents/endometriosis-beyond-the-basics/print
- https://www.self.com/story/12-signs-of-endometriosis
- https://ormfertility.com/10-endometriosis-symptoms-and-signs/
- https://nyulangone.org/news/endometriosis-six-symptoms-you-should-never-ignore
- https://my.clevelandclinic.org/health/diseases/10857-endometriosis
- https://www.arobgyn.com/what-is-the-difference-between-period-pain-and-endometriosis/
- https://www.mayoclinic.org/diseases-conditions/chronic-pelvic-pain/symptoms-causes/syc-20354368
- https://www.ncbi.nlm.nih.gov/books/NBK554585/
- https://www.ohsu.edu/womens-health/severe-menstrual-pain-not-normal
- https://www.endofound.org/painful-sex-dyspareunia
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9967948/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3096669/
- https://www.ncbi.nlm.nih.gov/books/NBK559230/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3538128/
- https://www.atlobgyn.com/blog/6-signs-you-may-have-endometriosis
- https://www.everydayhealth.com/endometriosis/silent-endometriosis-explained/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2880548/
- https://www.aafp.org/pubs/afp/issues/1999/1015/p1753.html
- https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661
- https://www.ncbi.nlm.nih.gov/books/NBK279498/
- https://www.ncbi.nlm.nih.gov/books/NBK279293/
- https://www.ncbi.nlm.nih.gov/books/NBK592411/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1459624/
- https://drseckin.com/unsuccessful-endometriosis-surgery/
- https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/12/dysmenorrhea-and-endometriosis-in-the-adolescent
- https://www.thewomens.org.au/health-information/periods/endometriosis/treating-endometriosis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7263080/
- https://www.medicalnewstoday.com/articles/321402
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10299570/
- https://www.drdanielkushner.com/blog/how-does-endometriosis-impact-mental-health
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10465859/
- https://www.endofound.org/painful-periods
- https://myoovi.co.uk/blogs/my-conditions/endo-pain-how-to-advocate-for-yourself
- https://www.endowarriorsaotearoa.com/about
