Prevalence of Endometriosis
What is the prevalence of endometriosis worldwide today?
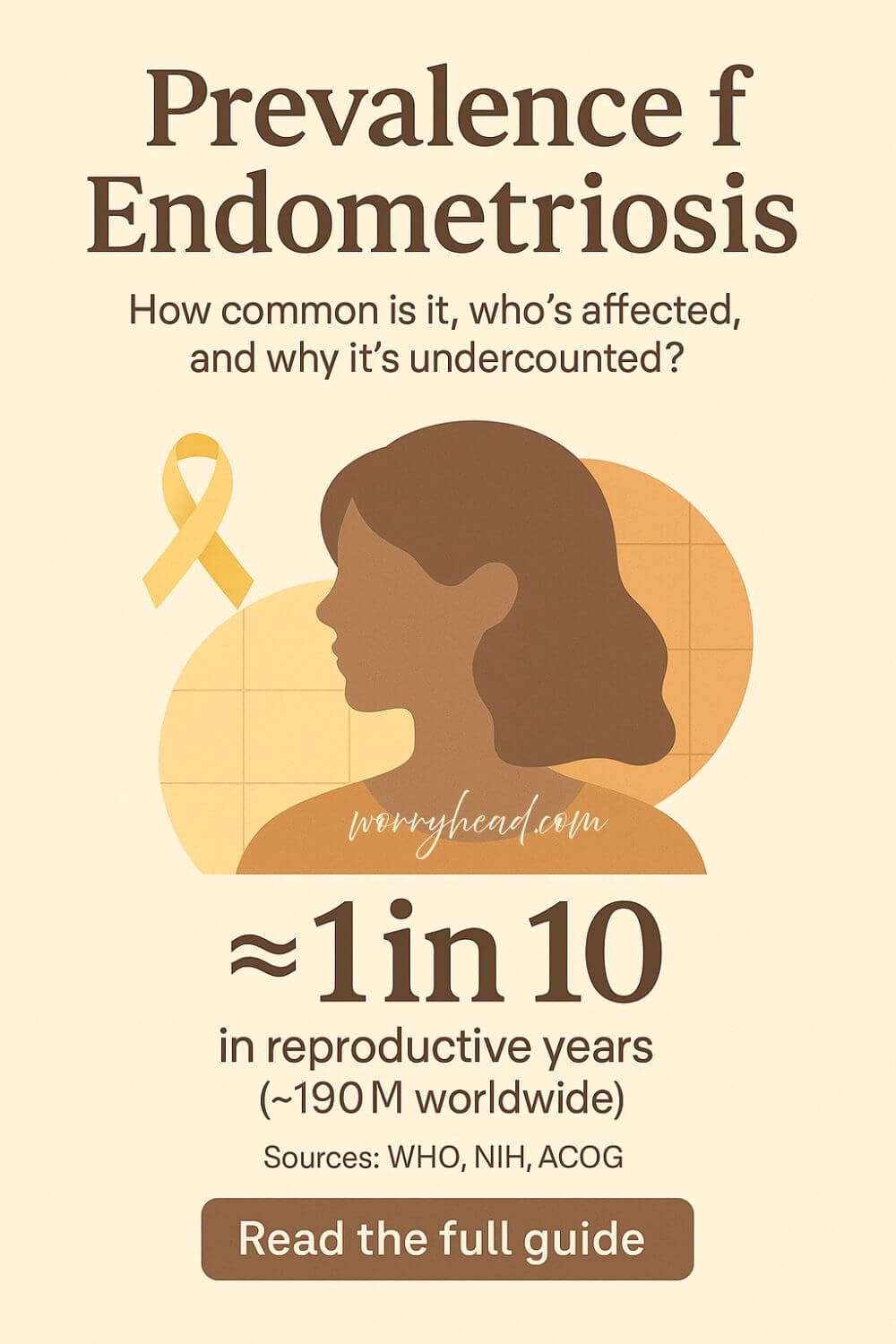
About 10% of women and others assigned female at birth in their reproductive years live with endometriosis, roughly 190 million people worldwide. Prevalence is higher in those with infertility or chronic pelvic pain, but exact figures vary because diagnosis is delayed and estimates differ by method.
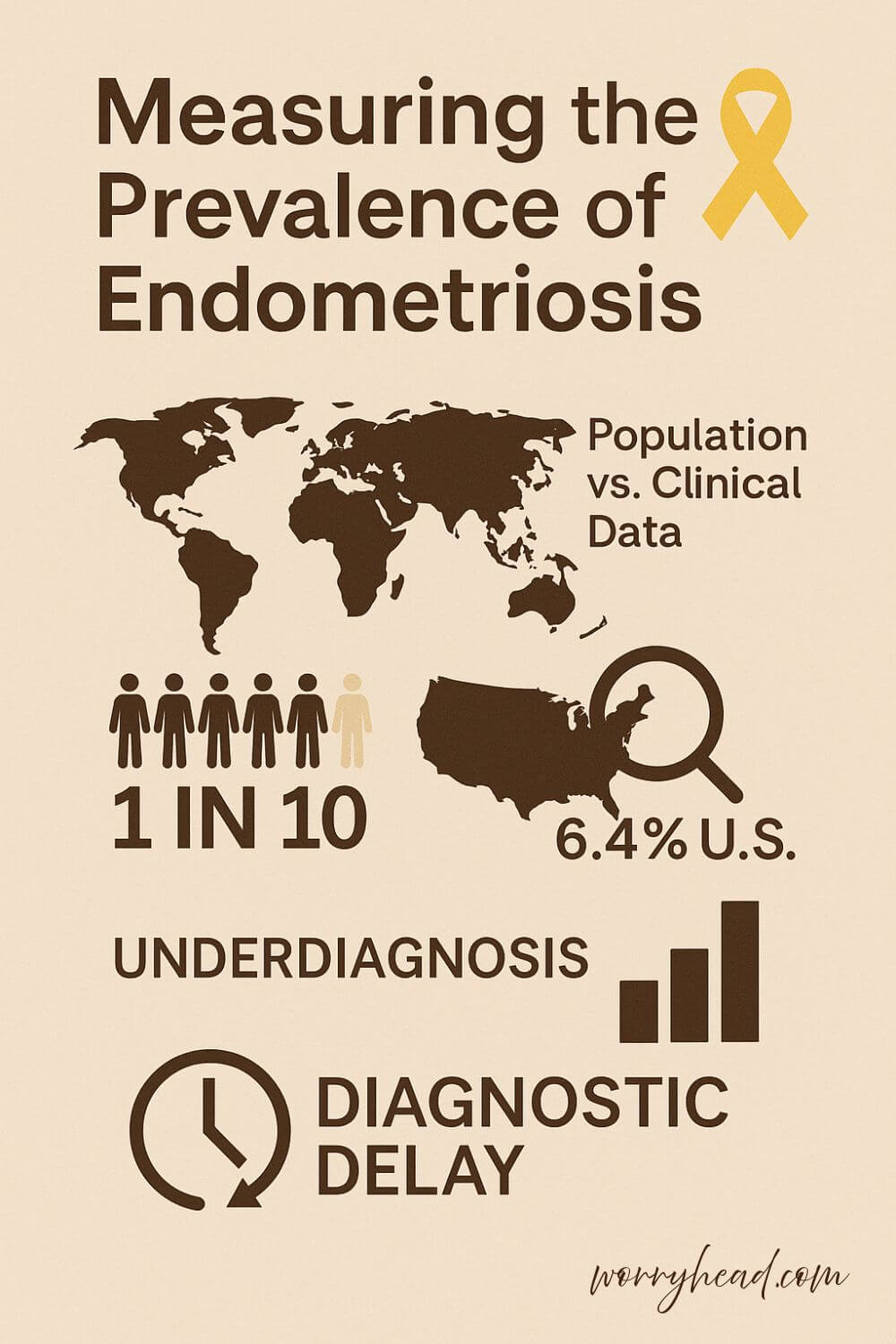
Measuring how widespread this disease is tricky because confirmation has long relied on laparoscopy or high-level imaging, and many people remain undiagnosed for years. Among adolescents with persistent pelvic pain, a large share are found to have the disease at surgery. In population data, estimates range: a recent U.S. analysis reported 6.4% nationally, while global snapshots commonly cite ~10%, reflecting differences in study methods and under-recognition.
When my wife’s pain first began, we had no idea we were stepping into a maze that so many quietly navigate. Seeing how long it took to be believed changed how I read every statistic because each number is someone’s life on pause.
If endometriosis is part of your story, you can grab a FREE chapter of my “Endo-Tool: Endometriosis for Men.” By joining, you’ll also become part of our community where I share more freebies, big discounts on all our books, and practical, compassionate emails to help couples adjust to the new normal this illness can bring.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis, and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men

- Measuring the Prevalence of Endometriosis
- Track Symptoms and Cycles Clearly
- Ask for a Specialist Referral Sooner
- Understand Laparoscopy’s Diagnostic Role
- Prepare for Targeted Pelvic Imaging
- Document Family History and Risks
- Advocate Confidently in GP Appointments
- Learn Guideline Basics Before Visits
- Seek Counselling for Anxiety and Pain
- Build an Everyday Self-Care Plan
- What Does the Prevalence of Endometriosis Mean for Your Life?
- Prevalence of Endometriosis and Us
- Final Word on the Prevalence of Endometriosis
- Prevalence of Endometriosis FAQ
- Prevalence of Endometriosis References
Measuring the Prevalence of Endometriosis
Counting how many people have this disease sounds simple, but it is anything but. Many are never diagnosed, and those who are often wait years, so the numbers you see depend on how a study defines a case and who can access care. Globally, health agencies still cite about 1 in 10 of those in their reproductive years, which translates to roughly 190 million people.
In clinics that see persistent pelvic pain or infertility, the share is much higher than in the general population.
Among adolescents who undergo laparoscopy for stubborn pelvic pain, surgical studies report strikingly high rates. This gap between population estimates and specialty findings is a reminder that method matters as much as medicine.
In the United States, diagnosed prevalence in large datasets ranges widely because it reflects who gets coded, not everyone who suffers. One national analysis reported 6.4% across 2011–2019, while other cohorts built from health records or insurance claims have shown lower figures, underscoring how underrecognition skews statistics.
Who is most likely to be counted also depends on risk. Earlier menarche, shorter cycles, family history, and certain congenital anomalies raise the odds, and many patients also face anxiety and other comorbid burdens that complicate daily life. These realities affect who seeks help and who gets missed in the data.
Access also shapes the numbers. In low and middle-income settings, limited specialist services and surgical capacity depress diagnoses, so national tallies can trail lived reality by years. Even where services exist, average diagnostic delay is still measured in years, not months.
When professional bodies explain how common it is, they echo that 1-in-10 headline while stressing that rates climb in groups with infertility and chronic pelvic pain. That message helps normalize symptoms without minimizing them, yet many readers still wonder if their pain “qualifies,” which is part of the undercount.
Adolescents deserve special attention. Studies of teens referred for laparoscopy show a substantial proportion with visible disease, which means school absence and sport drop-off may be warning signs long before an official label appears in a record. Families need to know that early attention is not overreacting.
All of this is why a single figure cannot carry the whole truth. The prevalence of endometriosis you see in headlines captures diagnosed cases; the reality underneath includes those still searching for names, care, and relief. Counting better is not academic nitpicking. It is how budgeting, training, and wait-lists get set.
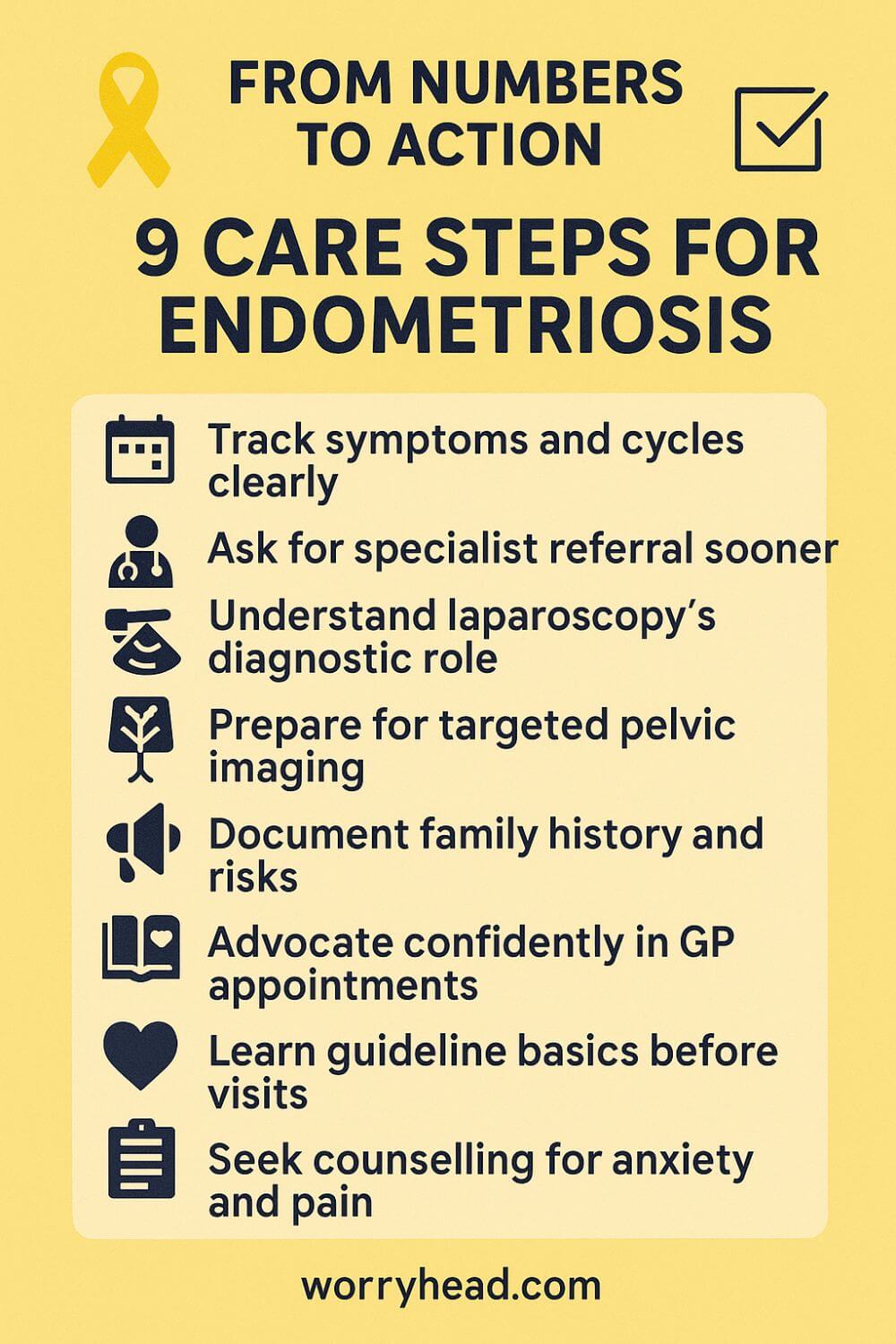
When my wife and I finally sat in front of the right specialist, years had already slipped away. Statistics felt cold until I realized each percentage point is a queue of women living their lives around pain, cancelled plans, and whispered fears. Before we dive into practical steps, here are gentle, grounded ways to move forward from numbers to action:
- Track symptoms and cycles clearly
- Ask for a specialist referral sooner
- Understand laparoscopy’s diagnostic role
- Prepare for targeted pelvic imaging
- Document family history and risks
- Advocate confidently in GP appointments
- Learn guideline basics before visits
- Seek counselling for anxiety and pain
- Build an everyday self-care plan
Track Symptoms and Cycles Clearly
Write it all down like you’re building a map back to yourself. Note pain days, flow, spotting, bowel or bladder changes, fatigue spikes, and the moments anxiety claws in. Patterns reveal themselves when you can see two or three months at a glance.
Use language that is specific, not “bad day” but “left-sided stabbing pain after ovulation, pain score 7.” Add what helped or didn’t: heat, gentle walk, NSAIDs, rest. Bring this to appointments so the conversation starts with data, not doubt. It shortens the delay in diagnosis of endometriosis and shows you’re an expert on your own body.
Ask for a Specialist Referral Sooner
If primary care stalls or suggests “watch and wait,” you’re allowed to ask for a gynecology referral. You’re not being difficult; you’re being thorough. Persistent pelvic pain, painful periods that stop life, pain with sex, or GI flares around the cycle are red flags that justify escalation.
Say, “Given my symptom history and impact on function, I’d like a referral to a specialist with endometriosis experience.” Name it. The sooner you reach someone who sees this daily, the faster you move from coping to clarity. Early access changes the natural course of endometriosis.
Understand Laparoscopy’s Diagnostic Role
Imaging can suggest disease, but laparoscopy remains the definitive way to confirm and stage lesions. Remember that this does not mean that everyone must rush to surgery today. It means that you should understand where it fits and what questions to ask if it’s recommended.
Ask about the surgeon’s experience, excision versus ablation, and how findings might shape treatment. Clarify recovery, risks, and realistic goals. A good team will talk through options, including when conservative management makes sense. Knowing this reduces fear and helps you make choices from knowledge, not panic.
Prepare for Targeted Pelvic Imaging
Specialized pelvic ultrasound or MRI in experienced hands can spot deep disease, endometriomas, and bowel or bladder involvement. Not every scanner or reader is the same. If possible, ask for centers with endometriosis protocols.
Before the scan, list symptoms and suspected sites: painful bowel movements, shoulder tip pain, urinary urgency. This context helps radiologists look with purpose. Imaging won’t find every lesion, but it can guide planning, spare surprises in surgery, and validate what you’ve been feeling for years.
Document Family History and Risks
If your mother, sister, or aunt suffered from endometriosis or adenomyosis, write it down. Early menarche, shorter cycles, heavy bleeding, and autoimmune patterns also matter. These aren’t verdicts; they’re clues.
Bring a simple family tree to appointments. Highlight fertility struggles, miscarriages, or severe menstrual issues in relatives. Clinicians are trained to weigh risk, and when you present it clearly, you help them consider endometriosis sooner. This simple page can tilt the conversation from dismissal to diligence.
Advocate Confidently in GP Appointments
Go in with a script and a goal. Lead with impact: school or work missed, intimacy affected, daily function reduced. Then present your symptom log and ask for imaging, a referral, or treatment options aligned with the ACOG endometriosis guidelines.
If you feel minimized, it’s okay to say, “I’m not feeling heard.” You deserve care that takes pain seriously. Bring a supporter if you can; two sets of ears catch more. Advocacy is not aggression, but it is protecting your life from becoming smaller than your potential.
Learn Guideline Basics Before Visits
Skim trusted summaries – NIH endometriosis pages, professional guidance – so you know the vocabulary: excision, ablation, combined hormonal therapy, GnRH analogs, pelvic floor therapy. You don’t need a medical degree; you need a compass.
When you understand options, you can spot when a plan fits your story or when it’s a copy-paste care. Knowledge reduces the power imbalance. It also helps you ask sharper questions like, “How does this choice affect fertility?” or “What’s the plan if first-line therapy fails?”
Seek Counselling for Anxiety and Pain
Endometriosis anxiety is real and rational. Pain rewires attention, steals sleep, and makes the future feel foggy. Counselling isn’t admitting defeat; it’s building tools. Look for therapists who are comfortable with chronic pain, couples strain, and medical trauma.
Skills like pacing, cognitive strategies, and compassion-based work soften the edges while you pursue medical care. If intimacy has changed, consider endometriosis counselling together. You’re not broken; you’re adapting. Emotional steadiness makes medical decisions clearer and daily life kinder.
Build an Everyday Self-Care Plan
Self-care here isn’t candles and slogans. It’s a repeatable plan that respects flare patterns and energy limits. Map meals you tolerate during the worst days, gentle movement you can sustain, heat routines, sleep anchors, and recovery windows after busy weeks.
Add boundaries you’ll actually keep, like no big commitments in the luteal phase if that’s when symptoms roar. Include partner roles so you don’t carry everything alone. This plan won’t cure disease, but it protects the life around it while you pursue proper treatment and a better endometriosis prognosis.
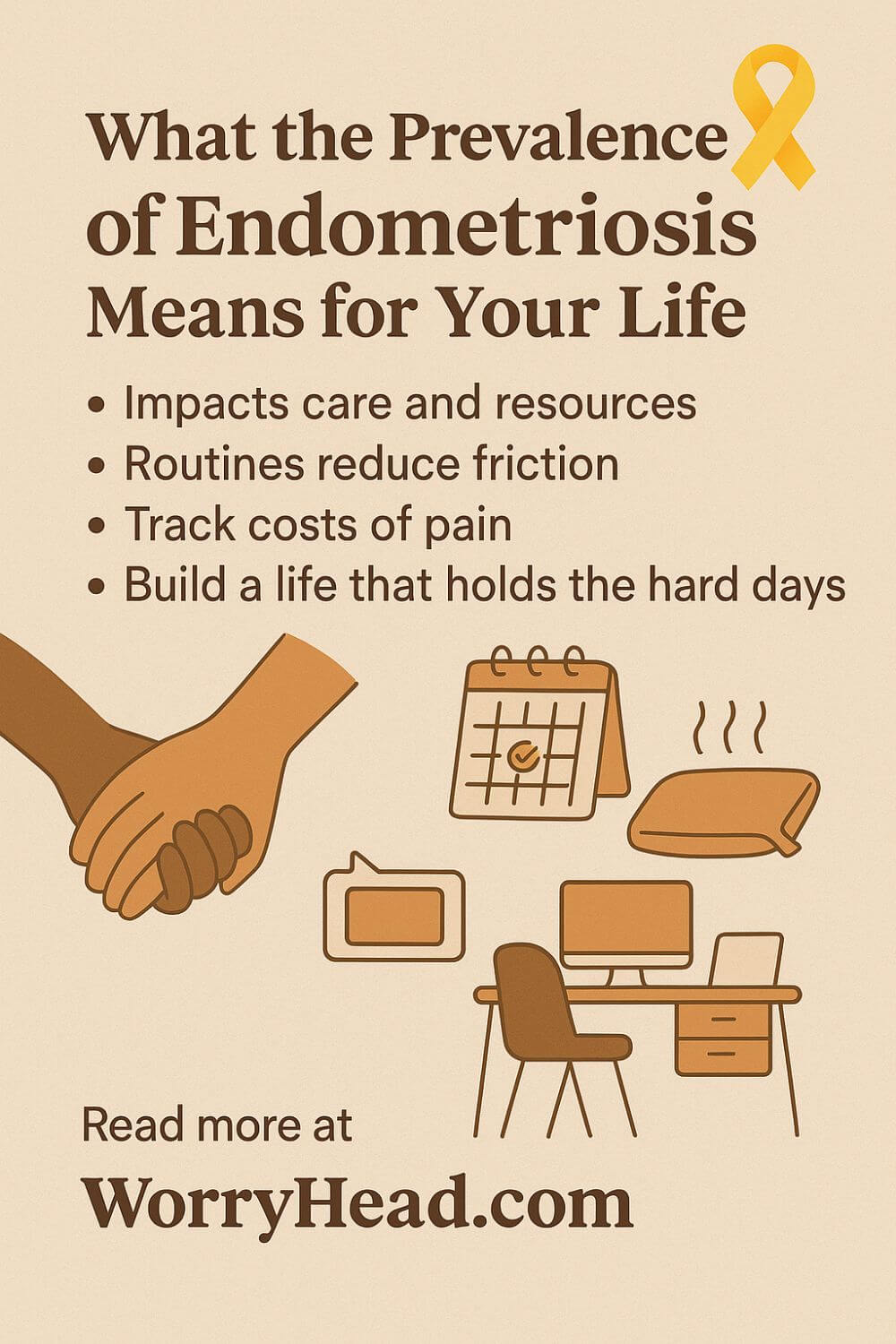
What Does the Prevalence of Endometriosis Mean for Your Life?
Statistics are only useful when they translate into care that shows up on time and with compassion. For us, the gulf between symptoms and help felt like standing on one side of a river, waving at a clinic across the water.
Numbers decide how many specialists are trained, how many MRI slots exist, and whether a school nurse takes severe cramps seriously. When the calendar fills with missed classes, cancelled dates, and half-worked shifts, data stops being abstract; it becomes a budget for hope.
I learned to track not just pain but the cost of it: unused train tickets, holidays deferred, the tiny heartbreak of saying “maybe” to everything. When those hidden costs are counted, families finally get permission to design life around health rather than squeezing health into the cracks.
That is why the prevalence of endometriosis must be measured with more than operating lists and insurance codes; it needs the truth of lived weeks.
Better counting pushes hospitals to build endometriosis pathways, not just gynecology waiting rooms, and it funds pelvic physio, counselling, and post-op follow-up as standard. It also changes the tone at home: partners feel less like overprotective worriers and more like teammates who are finally playing a visible game.
I remember holding my wife’s hand outside another appointment, pretending I wasn’t scared, promising her dinner by the sea when this was sorted.
Some nights we made pasta and laughed anyway; other nights I learned that love is carrying the bags, running the bath, and cancelling the world without resentment. None of this is dramatic.
It is discipline, the gentle, repeatable habits that keep identity larger than pain while the medical plan does its work. If you’re reading this and seeing yourself, let these words be proof that you’re not asking for too much; you’re asking for your life back, and that is the most reasonable request on earth.
Prevalence of Endometriosis and Us
When I understand the prevalence of endometriosis, I stop seeing our hard days as rare bad luck and start planning for them like the weather. It turns the chaos into patterns we can prepare for, not monsters we must fear.
For my wife, that means admitting mornings can be rough and building gentle starts into her week. Endometriosis anxiety often rides in alongside pain, so we budget emotional energy the way we budget money.
For me, it means keeping my calendar flexible, taking the heavy errands, and protecting her quiet without making her feel fragile. For us, it means routines that reduce friction: a heat pack always charged, simple meals prepped, a work-from-home setup that forgives flare days.
We treat care like project management, with one shared document listing meds, cycle notes, questions for appointments, and what helped last time. When intimacy gets complicated, endometriosis counselling gives us language and options so closeness remains spacious, not pressured.
Work-wise, building an online business from a calm home office gave us dignity and margin, because a traditional job rarely pauses for pain.
On the hardest nights, we read about the natural course of endometriosis and the honest range of endometriosis prognosis, then remind ourselves that progression is not linear and no article can tell you how quickly endometriosis progresses in any one body. Data becomes our compass, but love, boundaries, and practical kindness are the engine that carries us forward together.
Final Word on the Prevalence of Endometriosis
We began with numbers because numbers unlock resources, but it is the lives behind them that matter. If you have been living with pain, fatigue, bowel or bladder flares, and a sense that something is not being taken seriously, you are not alone, and you are not imagining it. What gets counted gets cared for; what gets dismissed gets delayed.
Counting is hard because diagnosis still leans on specialist skills and, too often, surgery. Many women are missed for years, so population figures feel smaller than the reality you see in waiting rooms. Clinic studies look larger because they start with those who have already broken through to referral. That gap is not a failure on your part; it is a signal that our systems must change.
Risk and access shape who gets labeled.
Earlier periods, strong family history, and certain anomalies raise suspicion, yet suspicion helps only if it leads to action. Where imaging protocols are strong and surgeons are trained to excise thoughtfully, people are found sooner and treated with more precision. Where services are thin, symptoms are managed in circles and hope frays.
What helps at home helps in the clinic. For example: a clear record of symptoms, a simple family map, and a calm, specific ask at appointments shorten the path.
Learning the language of options makes choices less frightening. Gentle routines, wise rest, pelvic physio, and supportive counselling protect your life while the medical plan takes shape. None of this replaces care; it prepares you to receive it fully.
I write as a husband who has kept the heat pack ready, rearranged work, and held my wife’s hand across too many corridors to count. We learned to plan for hard mornings, to give intimacy time and tenderness, to let our home office be a refuge rather than a reminder of limits.
Love is not loud here; it is steady, and it stays.
If today you are earlier in the journey, take heart.
You can ask for a referral. You can request imaging read by people who see this every week. You can bring a partner or friend to appointments, and you can say, kindly and firmly, that your pain is impacting function and plans. Bravery is not the absence of fear; it is choosing the next helpful step.
If you are further along, you know the power of a good team. Share what worked with someone just behind you. Quiet solidarity shortens the road for others and reminds you how far you have already come. There is no one right timeline and no one right outcome; there is the dignity of informed choice and care that respects your goals.
One phrase has guided us: build a life that can hold the hard days and still make room for joy. Statistics inform that work; your fierce, ordinary courage completes it. The map is not perfect, yet with the right support, you will not walk it alone.
You deserve timely answers, skilled care, and a life larger than pain. Track your story, ask for a referral, learn your options, and build routines that protect joy. With informed steps and kind support, hope becomes a plan, and your future opens again.
Have a question or a story to add? Leave a comment below, and if endometriosis is part of your life, grab a free chapter of my “Endo-Tool: Endometriosis for Men” to join our community for more honest help, bonuses, and big discounts.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MOREPrevalence of Endometriosis FAQ
1) How common is endometriosis?
Best current estimates suggest that about 1 in 10 people assigned female at birth in their reproductive years live with endometriosis. Rates are higher in groups with chronic pelvic pain or infertility. Because many go undiagnosed for years, true prevalence is likely higher than what medical records show.
2) Who is most likely to get endometriosis?
Anyone with periods can develop it, but the risk is higher with a first-degree relative affected, early menarche, shorter cycles, heavy bleeding, or certain Müllerian (uterine) anomalies. It affects people of every race and income level. Lifestyle does not “cause” it, and having children does not guarantee protection.
3) Why do prevalence figures vary so much between studies?
They depend on how “cases” are defined: surgical confirmation, specialist imaging, or diagnosis codes all capture different slices of reality. Access to care, cultural stigma, and long diagnostic delays also mean many cases never make it into datasets. Clinic-based studies usually show higher rates than population surveys because they see those already referred for symptoms.
4) Does endometriosis shorten life expectancy or raise mortality?
Endometriosis itself is not considered a fatal disease, and life expectancy is generally normal. However, it can be linked with significant pain, infertility, and mental-health burdens, and there is a small increased relative risk for certain conditions (for example, some ovarian cancers). Good, guideline-based care and follow-up help manage risks and improve quality of life.
5) What should I do if these numbers sound like my story?
Track symptoms clearly for 2–3 cycles, then ask your GP for a referral to a gynecologist experienced in endometriosis. Consider targeted pelvic ultrasound or MRI at centers with endometriosis protocols, and read a trusted guideline summary before appointments so you know your options. If anxiety or relationship strain is rising, add counselling, medical care, and emotional support; they work best together.
Prevalence of Endometriosis References
- https://www.who.int/news-room/fact-sheets/detail/endometriosis
- https://www.acog.org/womens-health/faqs/endometriosis
- https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/12/dysmenorrhea-and-endometriosis-in-the-adolescent
- https://www.niams.nih.gov/health-topics/endometriosis
- https://www.nichd.nih.gov/health/topics/endometriosis
- https://womenshealth.gov/a-z-topics/endometriosis
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9131783/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9127440/
- https://www.jpagonline.org/article/S1083-3188%2820%2930287-4/abstract
- https://journals.lww.com/greenjournal/fulltext/2018/12000/acog_committee_opinion_no__760_summary_.45.aspx
- https://www.sciencedirect.com/science/article/pii/S2949838424000239
- https://www.nature.com/articles/s44294-024-00048-6
- https://www.endometriosis-uk.org/diagnosis-report
- https://www.endometriosis-uk.org/sites/default/files/files/Endometriosis%20APPG%20Report%20Oct%202020.pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11625652/
- https://www.endometriosis-uk.org/endometriosis-facts-and-figures