Diagnosis of Endometriosis
What does a modern, accurate diagnosis of endometriosis actually involve today?
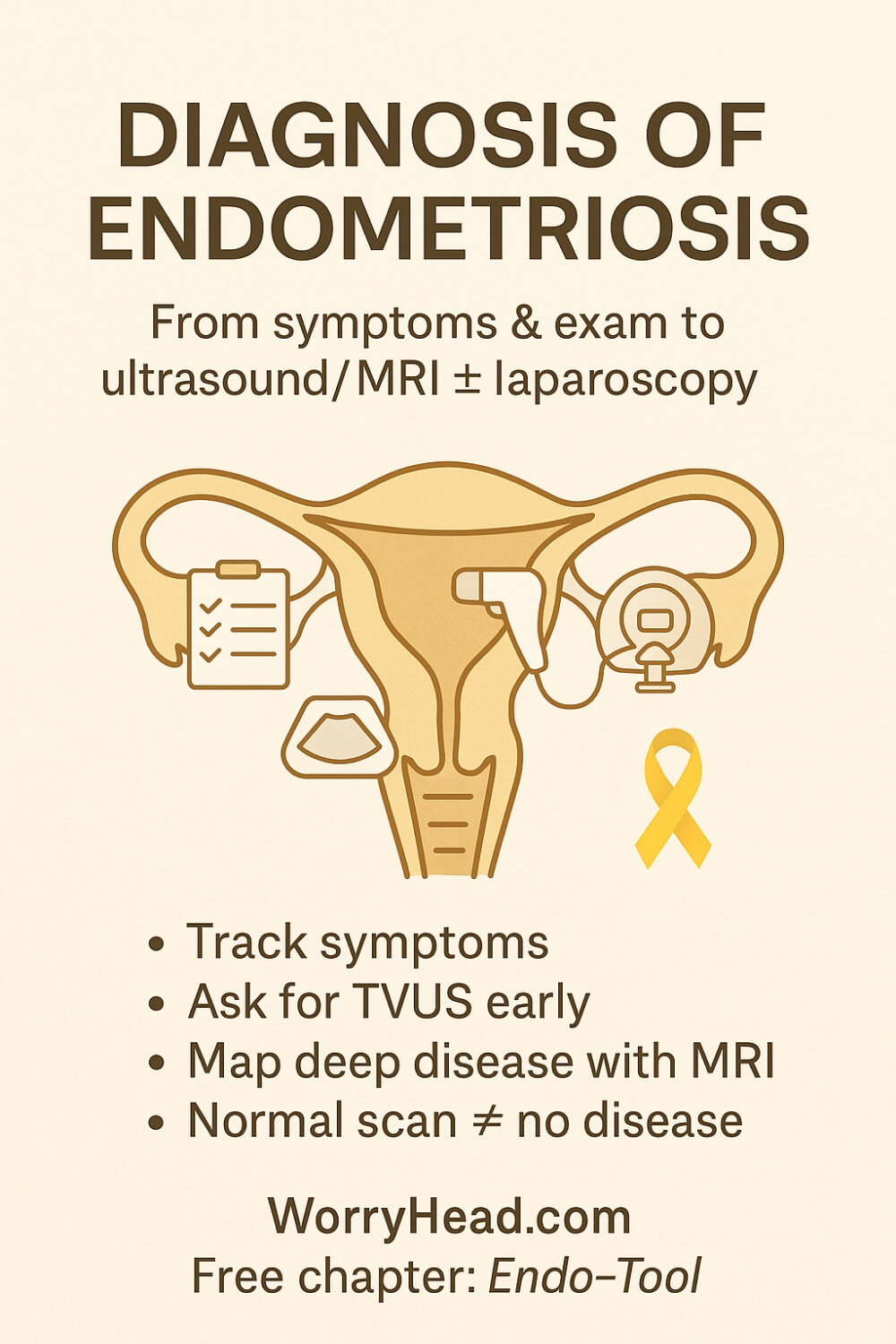
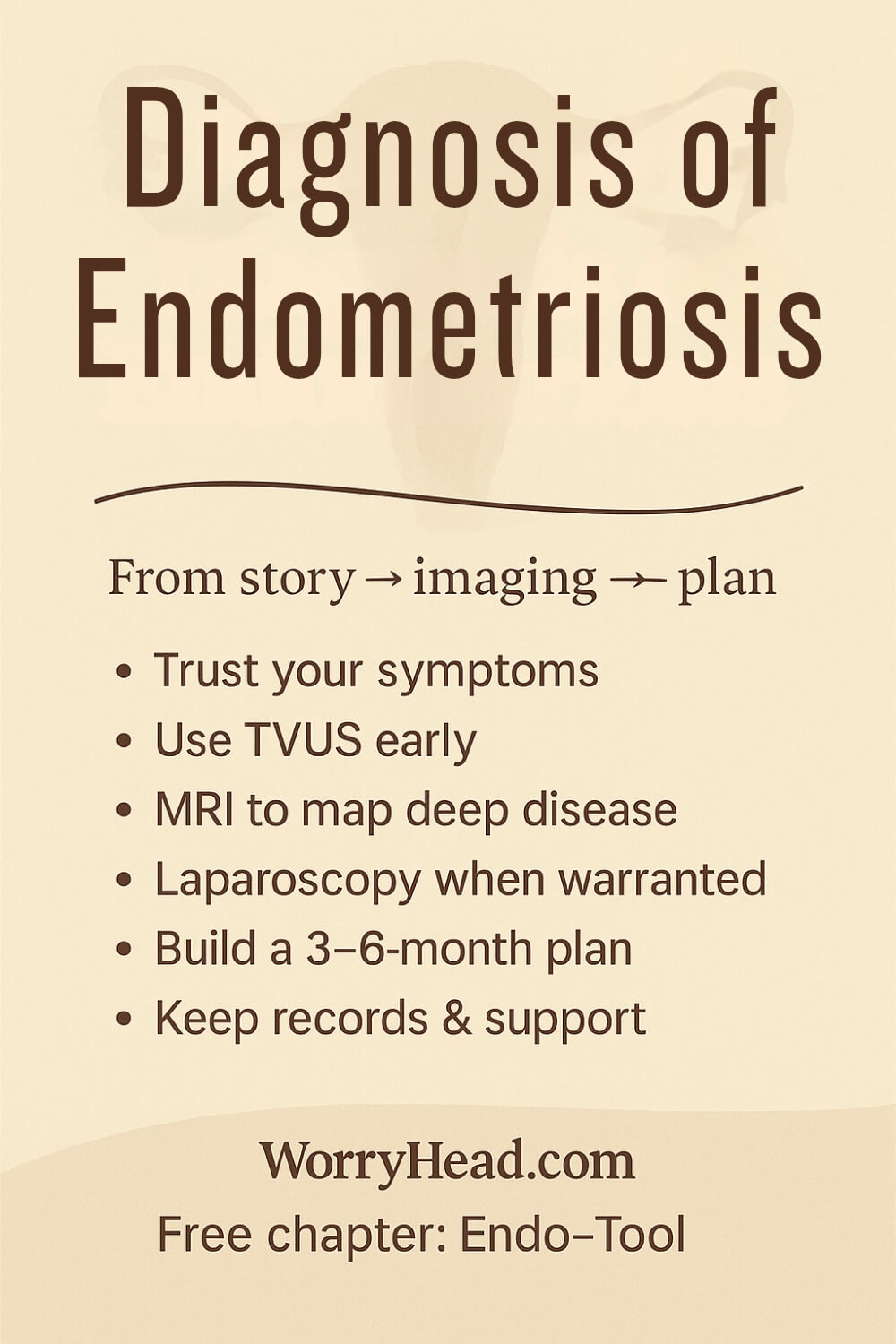
Diagnosis of endometriosis relies on symptoms and pelvic exam, supported by transvaginal ultrasound or MRI; surgery isn’t always required. Laparoscopy with biopsy can confirm and treat when needed, and updated guidelines now endorse earlier, clinically based diagnosis and compassionate care overall.
The landscape has shifted: laparoscopy is no longer the automatic “gold standard” starting point, with expert groups encouraging a working diagnosis based on history, exam, and imaging, especially for deep pelvic endometriosis.
Updated UK guidance (2024) prioritises earlier recognition to cut harmful delays and get treatment moving sooner. Ultrasound helps identify ovarian endometriomas; MRI with contrast refines mapping when disease is complex or deep.
And those delays are real: surveys and reviews show an average wait from first GP visit to diagnosis of about 8–10 years in the UK, with global averages around 6–7 years, far too long when every month of pain chips away at work, relationships, and hope. That’s why clear pathways and proactive primary care matter.
For us, this isn’t abstract. I watched my wife navigate years of symptoms, disbelief, and waiting rooms. Knowing what to ask for, and what tests actually help, changed everything for our family.
If this topic hits home, you can grab a free chapter of my book “Endo-Tool: Endometriosis for Men.” By joining our community, you’ll also get more freebies, big discounts on all our books, and emails packed with practical support to help both of you adjust to the new normal chronic illness brings.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis, and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men

Understanding the Diagnosis of Endometriosis
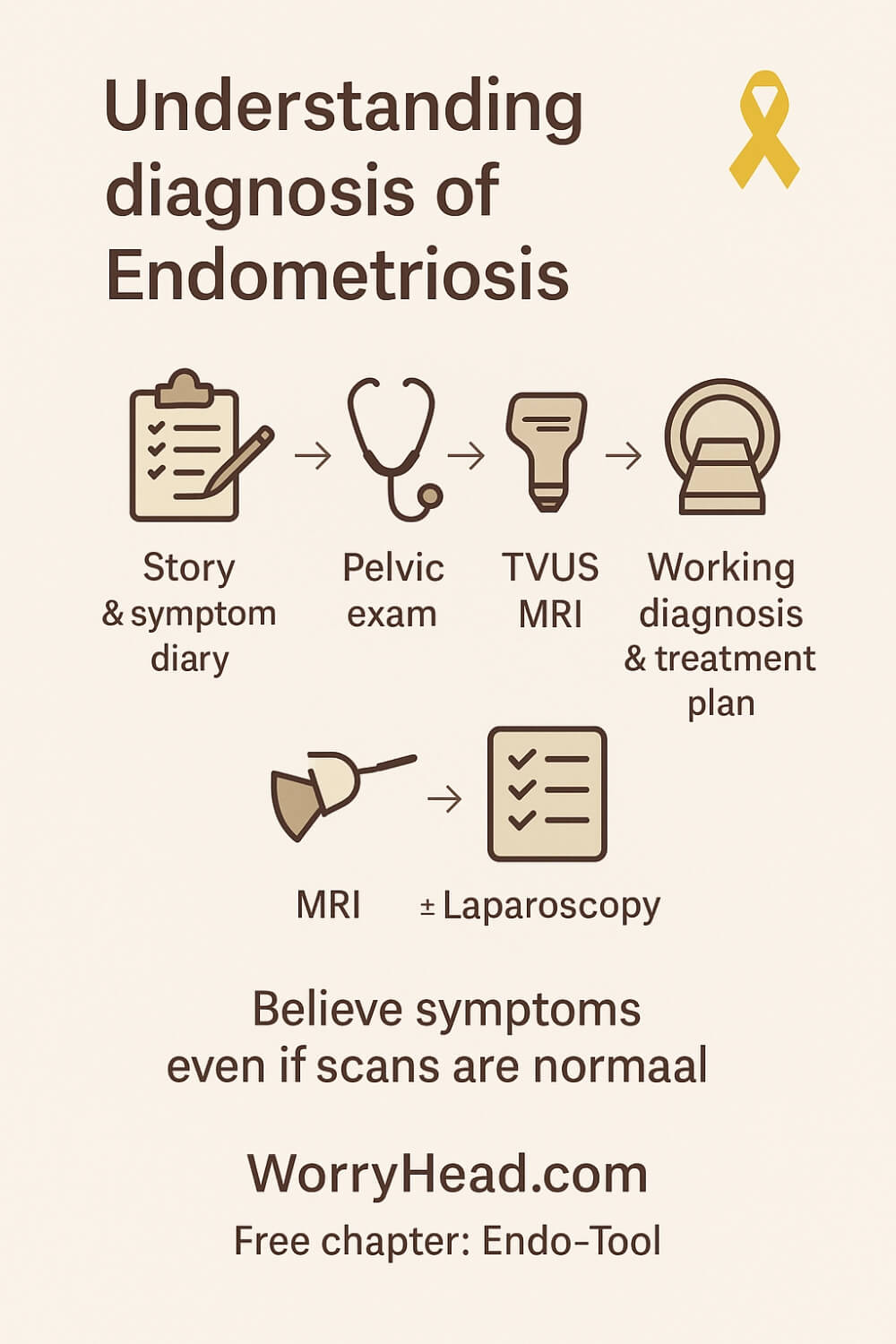
You start with a story, not a scan: pain patterns, bowel or bladder symptoms, fatigue, sex that hurts, days lost from work or school. A careful history and pelvic exam anchor the first step. When suspicion is high, a transvaginal ultrasound is now recommended early, even if the exam is normal, to identify ovarian endometriomas and signs of deep disease, and to rule out other causes.
If ultrasound can’t see what body keeps shouting, MRI can help map deep pelvic endo, especially when surgery is being planned or bowel, bladder, or ureter involvement is suspected. Protocols increasingly use MRI with contrast for better lesion characterisation and pre-operative planning, though accuracy varies by site and operator expertise.
Based on my wife’s diagnostic journey, I wouldn’t rely yon scans or MRI, and believe that the only true confirmation of endometriosis comes frorm surgery.
Here’s the critical shift: guidelines no longer insist that every path to certainty begins with a scope.
Clinicians can make a working diagnosis and start treatment based on symptoms plus imaging, and should not exclude the disease when scans are “normal” as they often do. That small sentence ends years of gaslighting for so many.
Definitive confirmation still exists: laparoscopy with biopsy can prove the tissue type and, in skilled hands, treat lesions in the same sitting. Balance clinical diagnosis first when appropriate, but have in mind that surgical confirmation or treatment when needed, is the modern, kinder pathway.
Why this matters: average time from first GP visit to a diagnosis in the UK is now 8 years and 10 months; globally, estimates hover around 6–7 years. That is nearly a decade of pain, missed promotions, strained intimacy, and too many nights wondering if you’re “imagining it.”
What sbout blood tests?
Well, despite exciting research and a few early commercial offerings, no biomarker is yet recommended in routine practice to rule in or out disease; imaging remains key, and surgery confirms when necessary. Keep an eye on this space, but don’t let a “normal” lab delay care.
Staging (how extensive lesions appear) can help plan treatment and set expectations, but stage doesn’t equal pain, some with “mild” appearance suffer profoundly, and some with extensive lesions feel less. What counts is believing symptoms and building a clear plan.
In our home, believing came first. I sat beside my wife through normal scans, abnormal pain, and the quiet shame that too many women carry. The day a clinician trusted her story, ordered the right imaging, and mapped a plan, I watched hope return to her eyes and I promised I would help other couples get there sooner.
Next, I want to hand you the most practical, lifesaving steps we learned – things I wish we’d known years earlier:
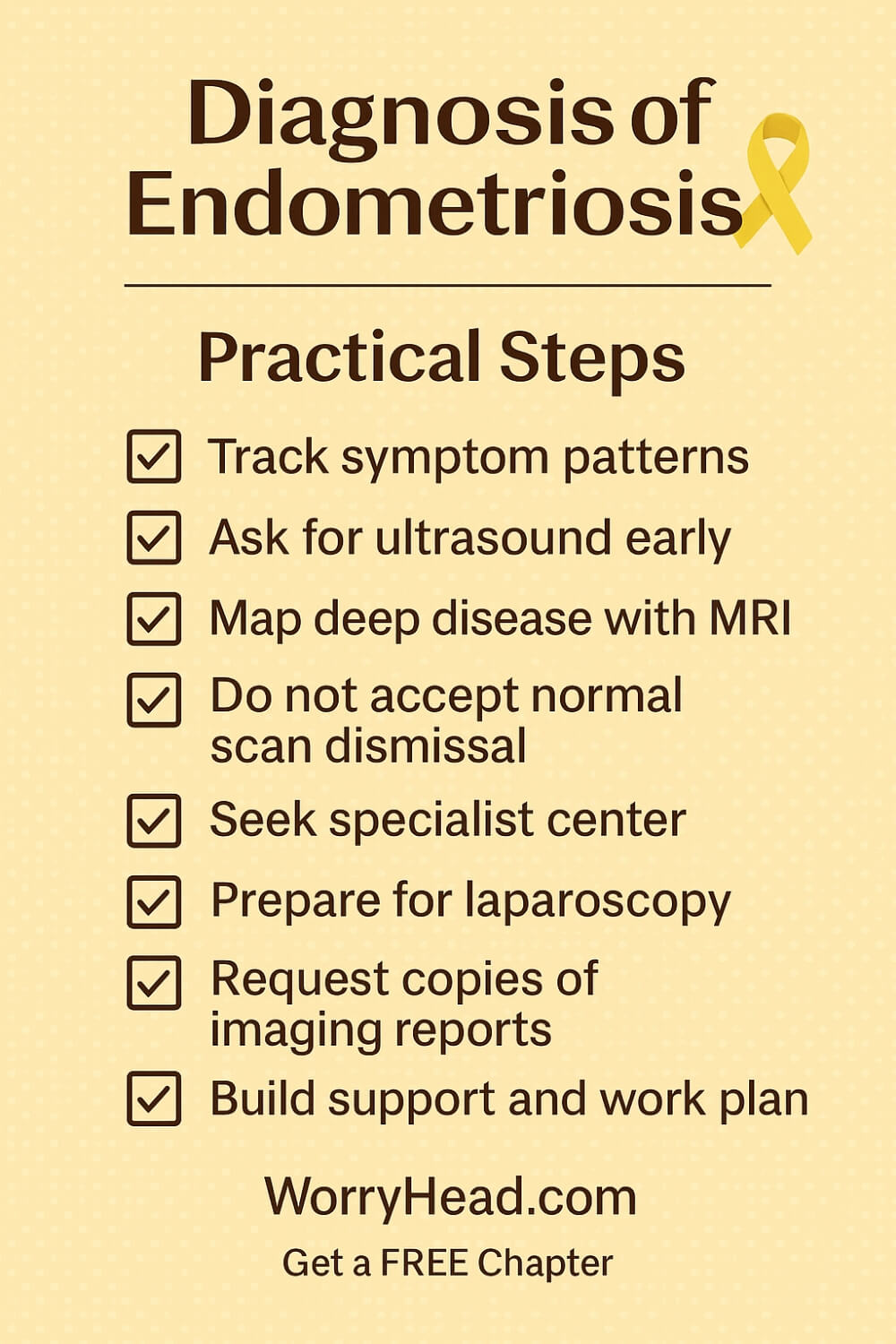
- Track symptom patterns with purpose
- Ask for transvaginal ultrasound early
- Map deep disease with MRI
- Don’t accept “normal scan” dismissal
- Seek an endometriosis specialist center
- Prepare for laparoscopy when warranted
- Request copies of imaging reports
- Build a support and work plan
Track Symptom Patterns with Purpose
I used to think we would remember all the pain details, but fear and fatigue blur the edges. Tracking brings clarity. Note what hurts, where, how it radiates, when it spikes in your cycle, and what helps even a little. Add bowel or bladder symptoms, nausea, night sweats, and how many days you miss from work or school.
Every two weeks, read the log together. Patterns start to speak. You can show a clinician hard data rather than scattered memories, and it changes the room. It also protects you from doubt when a scan is normal.
Use simple language. Morning cramps, dull ache left side, pain with sex, stabbing rectal pain day 2, relief with heat, worse after coffee. Small entries build a map.
For us, this record became proof and compass. It kept my wife seen on the worst days and gave me a way to help beyond holding her hand. That matters more than you think.
Ask for Transvaginal Ultrasound Early
The first time someone offered ultrasound without being prompted, I exhaled. Ask for it early, even if the exam is normal. Skilled transvaginal ultrasound can identify ovarian endometriomas, suggest adhesions, and sometimes hint at deep disease. It also rules out other causes that should not be missed.
Call ahead and ask if the sonographer has experience with suspected endometriosis. That one question saves time and heartache. Bring your symptom log and point to dates that match the worst pain.
If you have intense bowel or bladder symptoms, mention them clearly. Ultrasound may not see everything, but it sets a baseline and guides next steps.
You deserve speed, not a slow drip of referrals. Early imaging is not overreacting. It is stewardship of your health and your future days without pain.
Map Deep Disease with MRI
When pain wraps around the rectum, shoots down a leg, or makes every bathroom trip a negotiation, you need a map. MRI helps when deep pelvic endometriosis is suspected, especially before surgery. It shows compartments, possible bowel or bladder involvement, and the relationship of lesions to nerves and vessels.
Ask for pelvic MRI with an endometriosis protocol if available. Radiology reports should list compartments and suspected involvement in plain terms you can understand.
Bring the images to your consultation on a drive. Ask the clinician to walk you through them. Seeing anatomy on a screen turns fear into informed choice.
For us, MRI moved the conversation from “maybe” to “here is where” and “here is how we plan.” That shift rebuilt confidence and shortened the distance between suffering and action.
Do NOT Accept ‘Normal Scan’ Dismissal!
Normal imaging never cancels real pain. Endometriosis can be microscopic, hidden, or simply missed by an operator who does not know what to look for. If the report is normal but your body is not, ask what the next clinical step is rather than accepting a dead end.
Bring your diary. Ask, “Given these symptoms, what can we trial now?” Pain relief, hormonal options, pelvic floor therapy, or referral to a specialist center are valid steps. Have the plan written into your visit notes so it is not lost between appointments.
If you feel dismissed, seek another opinion. Request a copy of the report and ask if a second read by an expert is possible. You are not difficult for asking to be believed.
I watched my wife shrink after being told nothing was wrong. The day someone trusted her story, everything changed. Hold that line. You are not a scan.
Seek an Endometriosis Specialist Center
Specialist centers change the odds. They coordinate imaging, surgery, pelvic health physio, and pain management under one roof. Their teams read subtle scans differently and operate with techniques that protect fertility and function.
Ask your GP for referral criteria and waiting times. While you wait, gather records, imaging discs, and a summary letter of symptoms and treatments tried. Arrive as a prepared partner in your care.
Peer groups and patient stories can help you choose a center with experience in deep disease. Experience matters when lesions are near bowel, bladder, or ureters.
Walking into a clinic that speaks your language feels like stepping into daylight. I saw my wife breathe easier simply because the team understood before she finished her first sentence.
Prepare for Laparoscopy when Warranted
Surgery is not failure. It is one tool among many. When symptoms persist despite careful medical management or imaging suggests complex disease, laparoscopy may both confirm and treat. Preparation reduces fear.
Ask who performs the operation, their volume, and their approach to excision. Clarify fertility goals, risks, and what recovery will look like day by day. Discuss whether ablation or excision is planned, and what happens if bowel or bladder disease is found.
Pack practical items for discharge, plan time off work, and arrange help at home. Ask about bowel prep, pain protocols, and red flags that should prompt urgent review. Write down your questions and bring them to pre-op.
I learned to sit by the bed with soup and quiet presence. She learned to ask for strong pain control without apology. Prepared, we suffered less, healed faster, and kept our dignity intact.
Request Copies of Imaging Reports
Own your paper trail. Ask for the radiology report and the images on a disc or secure link every single time. Read the impression together, even if the language is technical. Over time, the terms become familiar and you spot changes that matter.
File everything in a shared folder with dates. Build a simple timeline that links symptoms, medications, imaging, and procedures. Bring it to every appointment, especially if you change clinics. Continuity is power in a system that often forgets to connect dots.
If a finding is unclear, send a brief message asking for clarification in plain language. Some hospitals offer patient portals with image viewers you can open at home. Respectful persistence keeps the plan moving.
Keeping records was the first time I felt useful beyond making tea. It turned chaos into continuity and helped the team see the whole story, not just a single visit.
Build Support and Work Plan
Endometriosis does not clock out at 5 pm. Build scaffolding around your life. Ask HR about flexible schedules, remote work, or sick leave protections. Create flare plans for meals, childcare, and transport so you are not negotiating through pain.
Loop in a trusted friend to sit in on big appointments and to be the person who texts after procedures. Small circles sustain you when stamina runs dry. If anxiety and low mood creep in, ask your clinician about counselling options and community resources.
At home, we keep heat packs ready, easy meals in the freezer, and a list of chores I take off her plate during flares. We set gentle routines that protect sleep and reduce noise on hard days. Relief is love made practical.
This is not giving up. It is building a life that bends without breaking while you pursue diagnosis and treatment with courage and patience.
Living the Path to a Diagnosis of Endometriosis
We moved from symptom diaries to real conversations, not as a case number but as two people who wanted our life back. The best appointments felt like teamwork, the clinician listening first and only then choosing the next step.
In those rooms we learned to translate pain into plans. Imaging was explained in plain words, what it could show, what it could miss, and how each result would change the road ahead.
A clear diagnosis of endometriosis is not one test, it is a timley pathway that combines your story, targeted imaging, and careful trials of treatment. You deserve consent that is informed and kind, with outcomes explained before anything begins. That kind of clarity turns fear into choices you can actually live with.
Sometimes the first move is medical therapy to calm a storm. Sometimes the wisest step is surgical evaluation with the right team, especially when daily life is shrinking around the pain.
We kept coming back to what mattered most. Could she keep her job, protect her fertility, and still have energy left for the parts of life that make a person feel like themselves.
I will never forget the day a clinician said I believe you and meant it. She cried in the car because the weight of doubt finally slid off her shoulders, and I held her hand like a man who had been waiting to exhale.
Since then we prepare for every visit with questions and goals, and we leave with written plans. We do not chase perfection, we chase progress we can feel.
If you are reading this in the thick of it, keep your notes, keep your courage, and keep asking for care that answers to your reality. You are not difficult, you are determined.
Hope is not a slogan here. It is the steady work of being listened to, mapped clearly, and treated by people who see your whole life, not just a chart.
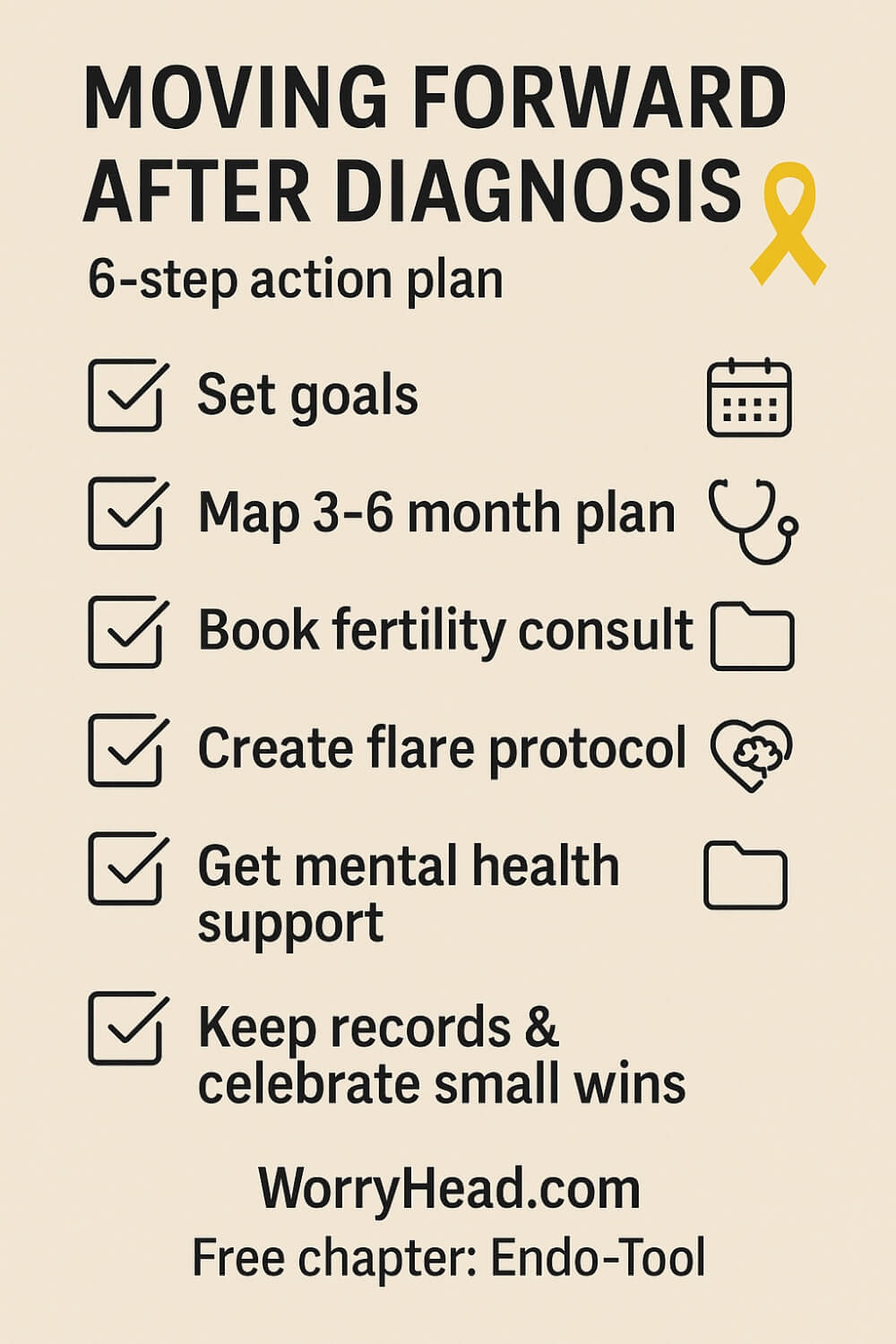
Moving Forward After the Diagnosis of Endometriosis
Getting a name for the pain, a diagnosis of endometriosis, is a doorway, not a finish line. The first days after clinic feel strange, relief that you were believed wrapped around grief for the years you lost.
We learned to turn that emotion into actions: write down goals for pain, work, intimacy, and energy so the team knows what “better” means to you. Ask your clinician to map the next 3 to 6 months on paper, medication trials, imaging reviews, or surgical dates, so time does not quietly slip away.
If fertility matters now or later, book a consult early to talk preservation, timelines, and how treatments may fit your plans. Bring a list of medications you have tried, what helped, what hurt, and any side effects, because clear history means fewer painful reruns.
At home, we created flare protocols, who calls work, which meals are ready in the freezer, which chores shift to me, so pain does not also create panic. On good days, we bank strength with gentle movement, pelvic health physio exercises, and sleep routines that keep the floor from dropping out.
Your mental health is part of the plan; trauma from years of dismissal can echo, so schedule support as seriously as scans. Share a one page summary of your condition with trusted people at work; that transparency traded shame for practical flexibility in our house.
And when opinions clash, seek a second read or a second surgeon, advocacy is not rudeness, it is survival. Most of all, celebrate small wins, because recovery is rarely linear, but every eased day is proof that you are moving forward.
Conclusion on the Diagnosis of Endometriosis
Finding a name for relentless pelvic pain is not a single heroic test, it is a sequence of good decisions made by you and a team that listens. It begins with a story told in detail, a careful exam, and imaging used with intent.
It may include medical therapy first or surgery when that is the safest, clearest step. The goal is not merely a label, but a plan that gives you days back, steadies your work and relationships, and protects the future you want.
What changed everything for us was understanding that clarity grows from preparation.
A symptom diary turns feelings into facts. Copies of reports and images turn fragmented visits into a continuous thread. Questions written in advance turn a rushed clinic slot into a meeting with outcomes. You deserve that standard every time. If a scan is normal and your life is not, the next step is to ask what else can be tried now, not to wait in uncertainty.
A modern pathway trusts your symptoms and uses ultrasound early, MRI when deep disease is suspected, and laparoscopy in skilled hands when confirmation or treatment is needed. None of these steps defines your worth or your strength. They are tools.
You are the person who must live with the results, so consent should include plain explanations, options, and time to think. Seek centres with expertise when disease may involve bowel, bladder, or ureters. Experience reduces complications and protects fertility.
Alongside the clinical work runs the quiet labour of building a life that bends rather than breaks. Flare plans, workplace adjustments, pelvic health physio, and sleep routines do not cure, but they create room to breathe while treatment unfolds.
Counselling helps repair the harm that years of dismissal can leave behind. Community makes the waiting bearable. Hope is not vague here. It is scheduled follow-up, written goals, and a team that calls you by your name.
I have sat in cars outside clinics where we cried from relief, not because pain vanished, but because someone finally believed her. That moment is the beginning, not the end. The diagnosis of endo matters because it turns random suffering into a navigable map.
With the right guides, you can choose a route that honours your body, your family, your work, and your dreams. Hold that line. Ask for care that answers to your reality. Keep the records. Keep the courage.
Better days are not a myth; they are the result of small, steady wins added together until life feels like yours again.
A clear path exists. You deserve to walk it with dignity, knowledge, and support, and to arrive not only with a diagnosis, but with a life rebuilt around what matters most to you and the person who loves you.
Empowerment begins now: trust your story, prepare your folder, ask precise questions, and choose partners in care who treat you as the expert in your own body.
Your next step can be small, but it counts.
I would love to hear your story. Leave a comment to help another reader feel less alone, and if you want practical, compassionate support from a partner’s perspective, grab the free chapter of “Endo-Tool: Endometriosis for Men.”


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MOREDiagnosis of Endometriosis FAQs
1). Can endometriosis be diagnosed without laparoscopy?
Yes. Many clinicians now make a working diagnosis using your history, pelvic exam, and targeted imaging. A skilled transvaginal endometriosis diagnosis ultrasound can identify ovarian endometriomas and clues to deep disease.
MRI with contrast for endometriosis helps map suspected bowel or bladder involvement and plan surgery when needed. Laparoscopy with biopsy still confirms definitively, but it is not required to begin treatment and support.
2). Are there reliable blood tests or online quizzes to diagnose it?
There is no validated endometriosis blood test in routine care yet. Biomarker research is active, but nothing currently rules the condition in or out.
A do I have endometriosis quiz or endometriosis self test can help you recognise patterns and advocate clearly, but quizzes cannot diagnose. If your symptoms fit, push for proper assessment rather than waiting for a lab to catch up with your life.
3). What if my scans are normal but pain is severe?
Normal imaging does not cancel real disease. Small or infiltrating lesions can be missed, and not all sonographers have advanced training in deep pelvic endometriosis.
Ask what the next clinical step is: trial of therapy, repeat imaging with an expert, or referral to a specialist center. Bring a symptom diary, request your reports, and consider MRI if red flags suggest deeper involvement. Your story is the anchor, not the scan.
4). How can I shorten the time to a diagnosis?
Come prepared. Track symptoms across the cycle, including bowel or bladder issues, fatigue, and days lost from work. Bring a concise history of treatments tried and responses. Ask specifically for transvaginal ultrasound, and for MRI if deep disease is suspected.
Seek clinicians familiar with the type of endometriosis that matches your symptoms, and do not hesitate to get a second opinion if you feel unheard. Preparation turns months into meaningful next steps.
5). When should I go to the ER?
Go urgently if you have sudden, severe pelvic or abdominal pain that does not ease, fainting or near-fainting, fever with worsening pain, heavy bleeding with clots and dizziness, vomiting with inability to keep fluids down, or symptoms of bowel or urinary blockage.
Ovarian cyst rupture or torsion, severe infection, or acute bowel issues can mimic or complicate endometriosis. If in doubt, seek emergency care; safety comes first for endometriosis when to go to ER.
Diagnosis of Endometriosis References
- https://www.nice.org.uk/guidance/ng73
- https://www.nice.org.uk/news/articles/nice-updated-guideline-to-improve-the-diagnosis-of-endometriosis
- https://www.nice.org.uk/guidance/ng73/resources/visual-summary-on-first-presentation-initial-management-diagnosis-referral-and-ongoing-care-of-pdf-13559822461
- https://www.nice.org.uk/guidance/ng73/resources/resource-impact-summary-report-13373534125
- https://www.nhs.uk/conditions/endometriosis/
- https://www.eshre.eu/guideline/endometriosis
- https://www.eshre.eu/-/media/sitecore-files/Guidelines/Endometriosis/ESHRE-GUIDELINE-ENDOMETRIOSIS-2022_2.pdf
- https://www.eshre.eu/-/media/sitecore-files/Guidelines/Endometriosis/ESHRE-ENDOMETRIOSIS-patient-Guideline_21032022.pdf
- https://www.endometriosis-uk.org/diagnosis-report
- https://www.endometriosis-uk.org/sites/default/files/2024-03/Endometriosis%20UK%20diagnosis%20survey%202023%20report%20March.pdf
- https://www.ncepod.org.uk/2024endometriosis/Endometriosis_A%20Long%20and%20Painful%20Road_full%20report.pdf
- https://www.nichd.nih.gov/health/topics/endometri/conditioninfo/diagnose
- https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661
- https://my.clevelandclinic.org/health/diseases/10857-endometriosis