Types of Endometriosis
What are the main types of endometriosis, and how do they differ?
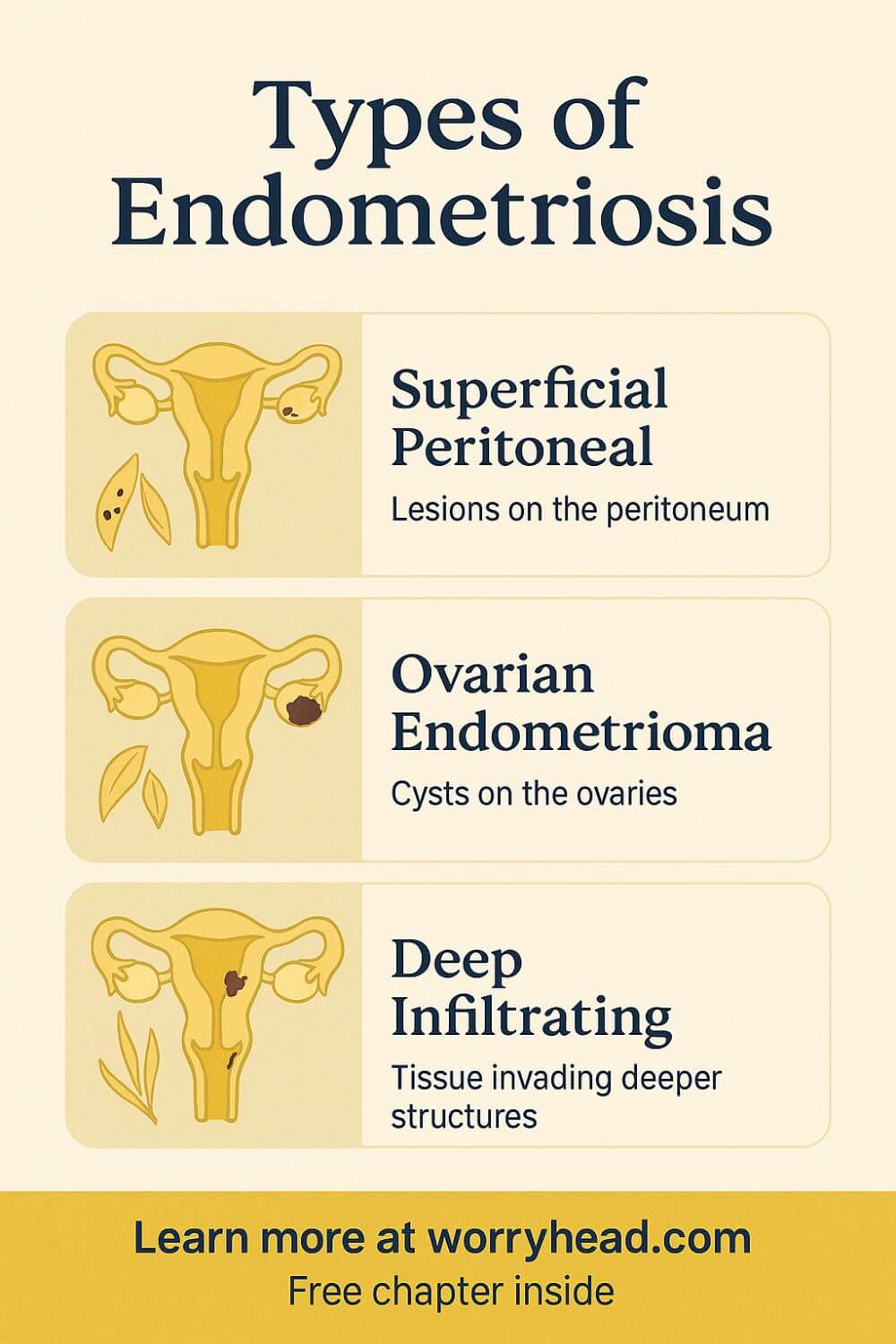
Superficial peritoneal disease sits on the pelvic lining; ovarian endometriomas form blood-filled cysts on the ovaries; and deep infiltrating endometriosis invades tissues under the peritoneum and nearby organs. These three patterns explain most clinical presentations and guide treatment choices.
Yet these labels rarely travel alone: lesions can mix across sites, mimic infections or fibroids, and even affect the bowel or bladder. Severity doesn’t always match pain. Imaging can miss subtle disease, and surgery sometimes reveals surprises. Understanding patterns helps you ask sharper questions and choose care with confidence.
It took years before my wife’s symptoms made sense; the map of her pain finally matched what surgeons found. Names gave us language and a plan.
If this topic touches your life, grab a free chapter of my “Endo-Tool: Endometriosis for Men.” By downloading it, you’ll also join our community, where I share more freebies, big discounts on all our books, and honest, practical emails to help you both adjust to the new normal chronic illness brings.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis, and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men

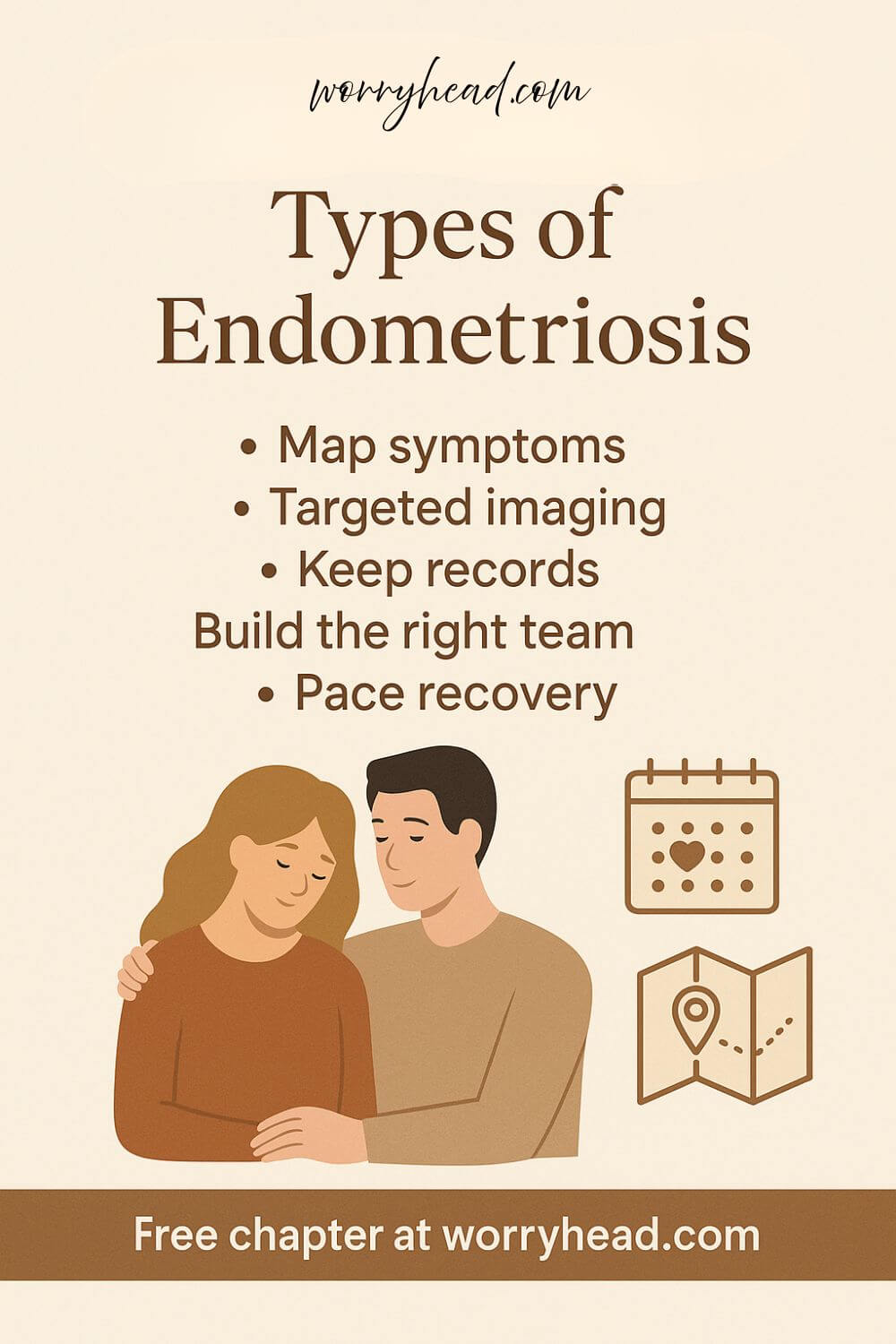
Understand the Types of Endometriosis
Doctors usually describe three disease patterns: superficial lesions on the peritoneum, ovarian endometriomas often called chocolate cysts, and deep lesions that infiltrate tissues beneath the peritoneum and can involve the bowel, bladder, or ligaments. Saying the types of endometriosis out loud gives shape to symptoms that once felt random.
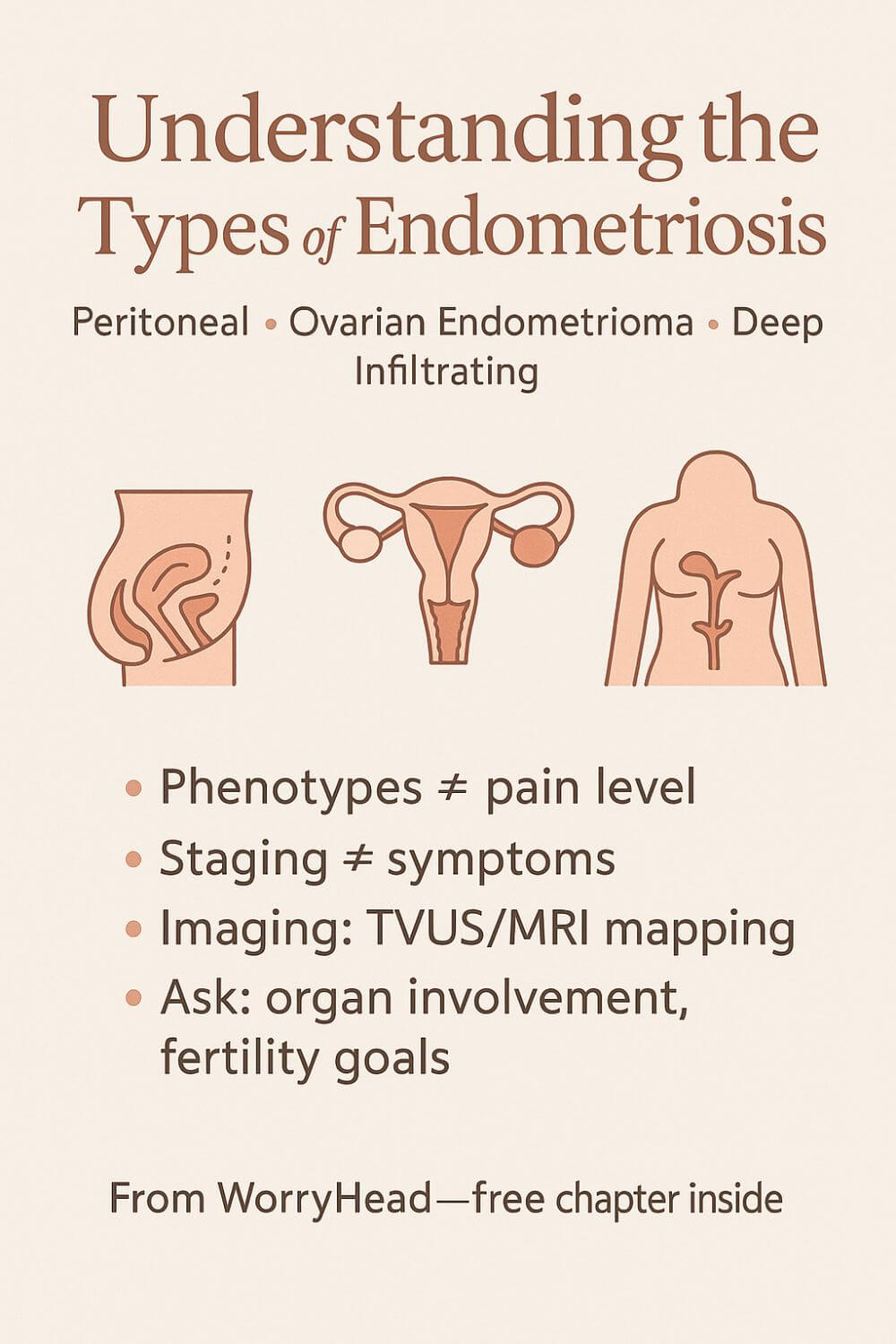
These patterns are phenotypes, not grades of pain. A tiny peritoneal spot can drop a strong woman to her knees, while someone with extensive disease may function on habit and grit.
Classification is also different from staging. The common stages I–IV describe surgical findings, such as extent and adhesions, but they do not reliably predict pain, fatigue, or how your month will unfold.
Imaging can help when it is targeted. A skilled transvaginal ultrasound can detect ovarian endometriomas and many deep lesions, while MRI with an endometriosis protocol maps complex sites before surgery.
Ovarian endometriomas are more than cysts. They can reduce ovarian reserve over time and complicate fertility planning, which is why individualized counseling matters long before family-building decisions feel urgent.
Deep infiltrating disease can tether organs and narrow the bowel or ureters. That is why red flags like cyclical rectal bleeding, pain with bowel movements, urinary urgency with blood, or shoulder-tip pain with menses deserve careful evaluation.
There are extrapelvic locations, too. The diaphragm, lungs, abdominal wall, and even surgical scars can host lesions that create puzzling patterns like cyclic chest pain or bleeding from a scar.
Adenomyosis often travels with endometriosis, but it is different. It lives inside the uterine muscle, causing heavy periods, clotting, and a stubborn, deep ache that can look like pelvic inflammatory disease or endometritis at first glance.
Not finding lesions at laparoscopy does not end the story. Disease can be missed without an experienced excision surgeon or proper visualization, and symptoms still deserve treatment and follow-up.
Treatment choices hinge on goals. Pain control, organ protection, and future fertility can pull in different directions, so the best plan is the one aligned with your season of life, not someone else’s checklist.
Some will try hormonal suppression to quiet lesions and reduce inflammation. Others need meticulous excision by a team that can manage bowel or urinary tract involvement safely.
Recovery is not linear. Scar tissue, nerve sensitization, and the long memory of pain can linger even after successful surgery, which is why pelvic floor therapy, pacing, and trauma-aware care belong in the plan.
For those thinking about pregnancy, timing matters. Endometriomas and deep disease can affect ovarian reserve and implantation, but many still conceive with or without IVF when care is coordinated thoughtfully.
Community matters more than it seems. Finding clinicians who listen and people who believe you is part of treatment, because validation lowers the quiet panic that keeps the nervous system on high alert.
Progress can feel slow, but clarity helps you take the next right step instead of spinning in fear. Knowing your phenotype helps you ask for the right imaging, the right surgeon, and the right pacing at home.
When my wife finally learned where her lesions lived, the map explained years of confusion. We cried in the car after the consult, not from fear this time, but from the relief of a name and a plan. The next section is the list we wish we had on day one: practical steps that turn understanding into action.
- Track symptom location and timing with a pelvic map
- Ask for an expert transvaginal ultrasound or MRI with protocol
- Collect and keep surgery photos, reports, and imaging CDs
- Screen for adenomyosis when bleeding is heavy and crampy
- Learn red flags for bowel and urinary involvement
- Discuss fertility goals early and protect ovarian reserve
- Prioritize excision consultation if suppression fails
- Plan recovery with pelvic floor therapy and pacing
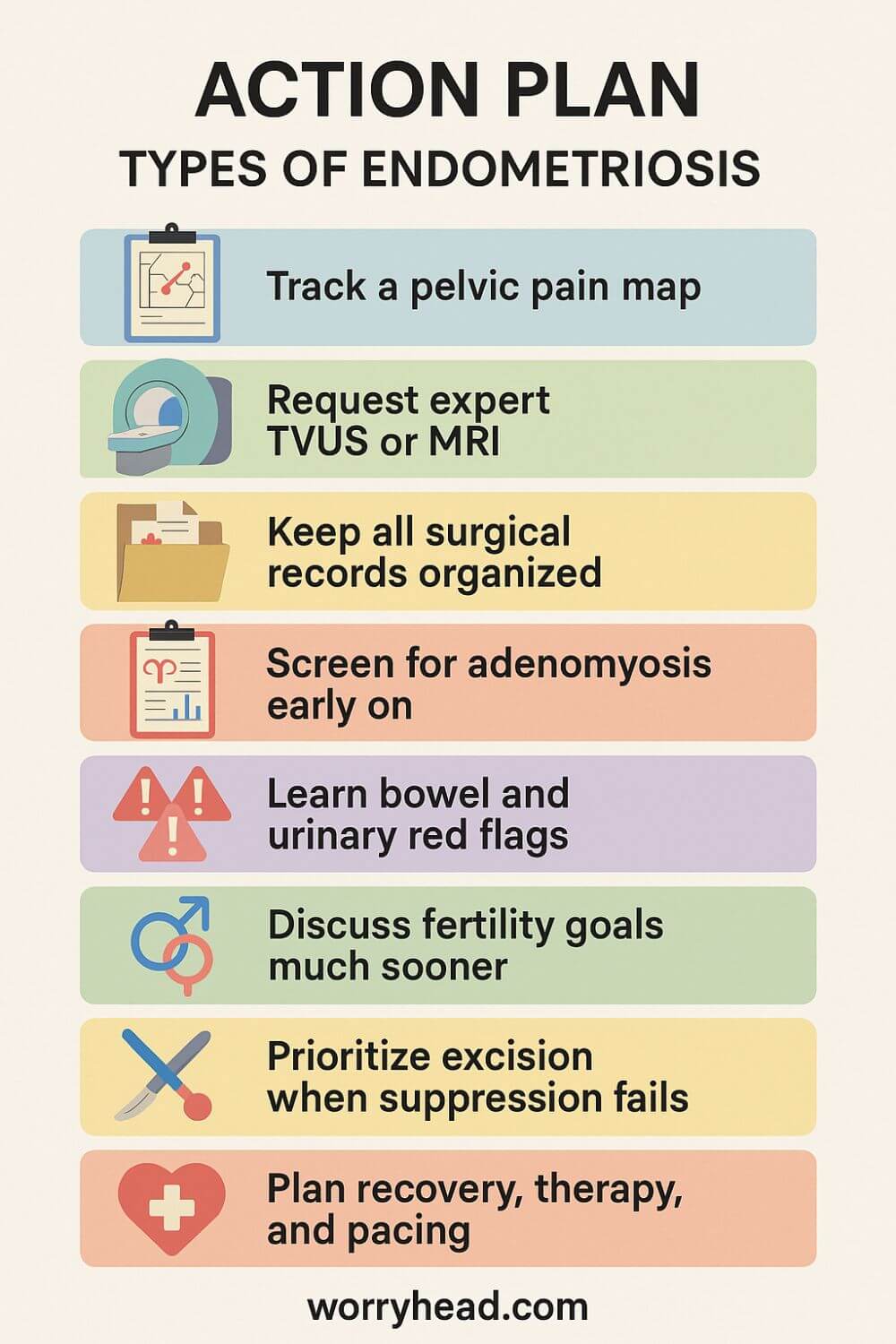
Track a Pelvic Pain Map
A pelvic map turns chaos into patterns. Print a simple diagram and note where pain shows up, how it feels, and when in your cycle it spikes. Add bowel or bladder symptoms, shoulder-tip pain, and fatigue, too. Two minutes a day builds a picture doctors can’t ignore.
After a month, you’ll notice rhythms that memory alone blurs. We saw how her left-sided ache always flared two days before bleeding, while deep rectal pain peaked mid-cycle. That detail changed the questions we asked and the referrals we pushed for. Data is advocacy in ink.
Request an Expert TVUS or MRI
Not all scans are equal. A targeted transvaginal ultrasound by an endometriosis-savvy sonographer can identify endometriomas, nodules in the rectovaginal septum, and sliding-sign restrictions. If the disease seems complex or bowel or ureter involvement is suspected, ask for an MRI with an endometriosis protocol.
Bring your symptom map, and name specific concerns so the radiologist knows what to look for. We learned to ask about bowel tethering, ureteral narrowing, and cul-de-sac obliteration. Clear questions lead to clear imaging notes. Good pictures don’t cure pain, but they aim the plan.
Keep All Surgical Records Organized
Treat every report like gold. Keep laparoscopy notes, operative diagrams, pathology, photos, and the video if available. Back it all up to a cloud folder and a USB. Future clinicians make better decisions when they can see what was found, biopsied, and removed.
We discovered how often crucial details get lost between clinics. Having the photos in hand prevented a second guess about prior excision and confirmed where adhesions were lysed. Organization saves time, money, and heartache. It also stops you from having to retell painful history from scratch.
Screen for adenomyosis early on
Heavy bleeding, clots, a boggy, tender uterus, and a deep, diffuse cramp that laughs at standard painkillers can point to adenomyosis. Ask for a targeted ultrasound looking at junctional zone changes, and consider MRI if symptoms are severe or medical therapy isn’t helping.
Adenomyosis can travel with endometriosis and change treatment goals. Knowing it early reframes choices about hormones, surgery, and fertility timing. It explained my wife’s relentless heaviness when peritoneal spots looked “mild.” Naming it validated her pain and reshaped the plan.
Learn Bowel and Urinary Red Flags
Cyclical pain with bowel movements, constipation that alternates with diarrhea, rectal bleeding during periods, or a feeling of blockage deserve attention. On the urinary side, urgency, burning without infection, flank pain, or blood in urine around menses are signals to escalate care.
Write these down and report timing precisely. Ask whether deep disease of the rectum, sigmoid, bladder, or ureters is possible, and whether a multidisciplinary team is needed. We learned to treat these signs as urgent, not dramatic. Protecting organs is not optional.
Discuss fertility goals much sooner
You don’t have to be trying now to talk about options. Endometriomas and repeated ovarian surgery can chip away at reserve, and age keeps moving. Ask for AMH and antral follicle count when appropriate, and discuss how any proposed surgery may affect the ovary.
Early clarity lowers pressure later. We talked about timelines, possible egg freezing, and when to try naturally after treatment. Just naming hopes and fears took weight off her shoulders. The best plan fits the season you are in, not someone else’s calendar.
Prioritize Excision when Suppression Fails
Hormonal suppression can quiet symptoms, but if pain breaks through or organ risk appears, ask about expert excision. Seek a surgeon who treats deep disease regularly and can operate with colorectal or urology colleagues when needed, so one operation addresses all involved sites.
We learned that incomplete surgery can mean repeat trauma. A thorough consult should review imaging, likely findings, risks, and recovery supports. When we finally met the right team, the plan felt careful, not rushed. Precision matters when quality of life is on the line.
Plan Recovery, Therapy, and Pacing
Recovery is more than wound healing. Scar remodeling, pelvic floor tension, and a vigilant nervous system need time and care. Build a plan that includes pelvic floor physiotherapy, gentle mobility, bowel support, and graded return to activity. Protect sleep like medicine.
We scheduled rest days the way others schedule meetings. Pacing gave her permission to stop before the crash. That respect for limits shortened setbacks and made gains stick. Healing is not linear, but a thoughtful plan bends the curve toward steadier days.
Making Sense of the Types of Endometriosis in Real Life
Labels help us plan care, but they don’t tell the whole story. What mattered most for us was translating medical notes into choices we could live with.
Peritoneal specks caused knives-on-glass pain when she sat too long; a small endometrioma tugged during ovulation and stole weekends. Deep nodules explained pain with bowel movements and the way her body braced against touch.
Once we had a map, we matched symptoms to specialists instead of bouncing between quick fixes. Pelvic floor therapy became as essential as medication, and nutrition was tuned to manage bloat and energy swings.
We also learned to separate fear from risk: not every cyst needs surgery tomorrow, and not every quiet month means remission. Tracking patterns over three cycles made our decisions calmer and our appointments sharper.
When the word “excision” entered the room, we asked about surgeon volume, access to colorectal and urology colleagues, and how often they operate on bowel or ureter disease. Prepared questions turned a scary consult into a partnership.
For fertility, we talked openly about reserve, timing, and the possibility of pausing suppression to try, because hearts and ovaries keep their own calendars. Even then, we protected her body from repeat procedures that could chip away at options later.
In the end, naming the types of endometriosis gave us language, but love, pacing, and informed consent gave us our lives back.
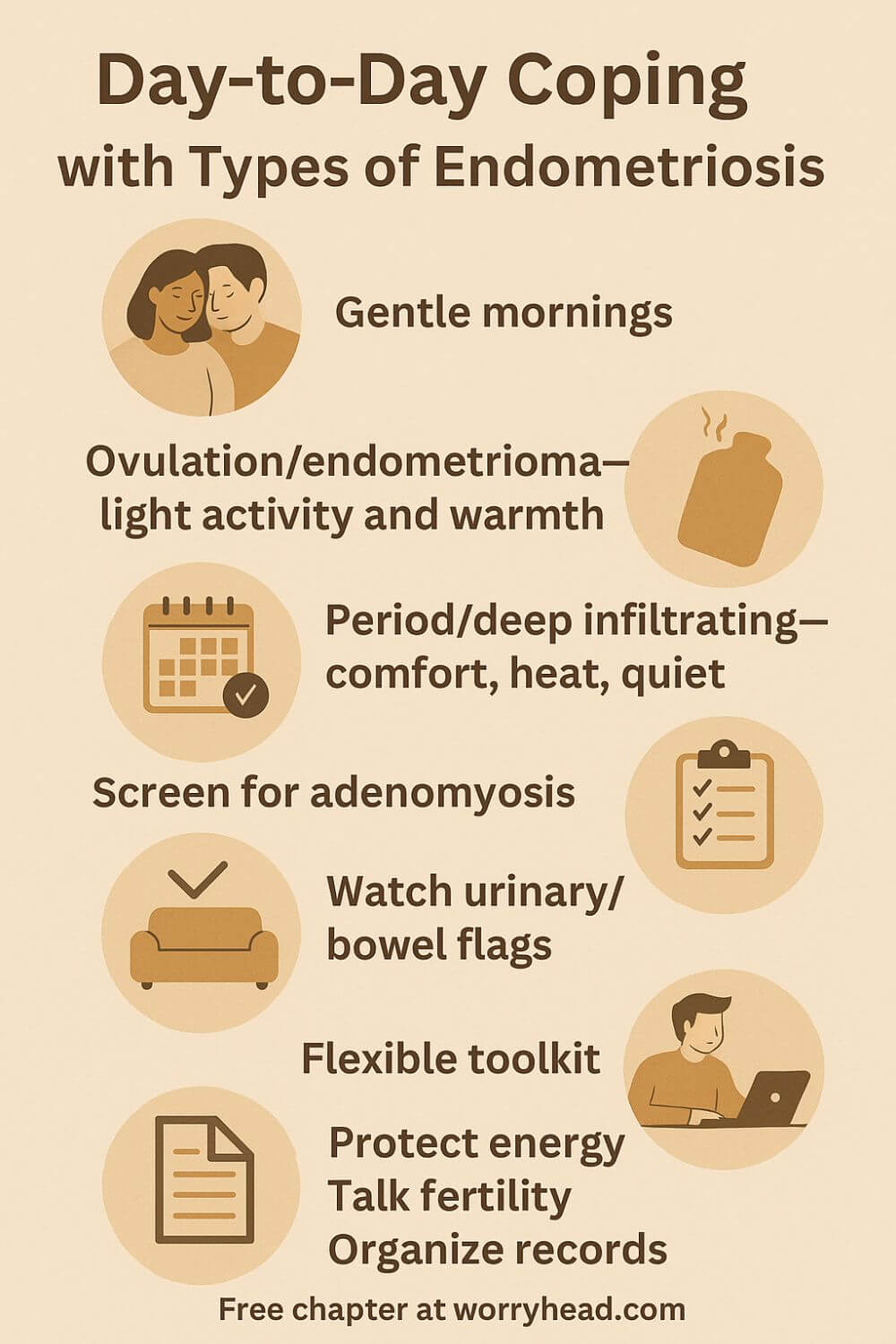
Day-to-Day Coping with the Types of Endometriosis
Learning how the types of endometriosis mapped onto my wife’s body changed our routine more than any single medication. Mornings became gentler, meetings were scheduled later, and we started planning meals and rest around her endometriosis symptoms instead of pretending she could outrun them.
During ovulation weeks, a stubborn ovarian endometrioma tugs like a weight, so we swap heavy lifting for walks and warmth. Period days carry a deeper, pressure-like ache that hints at deep-infiltrating endometriosis, so comfort, heat, and quiet become non-negotiable.
Heavy bleeding and a boggy, relentless cramp made us screen for adenomyosis early, rather than mislabel it as pelvic inflammatory disease or endometritis. Naming things brought kinder choices and fewer arguments with ourselves about willpower.
We track tiny triggers that add up: long car rides, skipped meals, and sleep cut short. When urgency and pink-tinged urine showed up around her cycle, we treated it as a flag for possible blood in urine, endometriosis, and asked the right questions fast.
Treatment became a flexible toolkit, not a single path. Hormonal suppression had seasons; pelvic floor therapy, gentle mobility, and an anti-inflammatory routine stayed steady when medicines changed.
My job is to protect her energy and our hope. I handle the errands, pad the calendar, and keep our home office calm so she can work when pain loosens its grip and rest without guilt when it doesn’t.
We talk honestly about endometriosis and pregnancy, letting goals guide decisions instead of fear. That honesty keeps us aligned when choices about timing or preserving ovarian reserve feel heavy.
We keep imaging, reports, and notes organized so each appointment builds on the last. Clear records cut through doubt, prevent repeat trauma, and remind us how far we’ve come.
Some days still collapse under pain, and we start again. But we’ve learned that softer mornings, smarter pacing, and steady compassion turn surviving into living, together.
Final Word on the Types of Endometriosis
If you are here, you are likely tired of being told your pain is mysterious. I was too, standing beside my wife through years of normal scans, brushed-off appointments, and the quiet fear that maybe this was simply life now. It wasn’t. Clarity came when we stopped chasing a single fix and started building a careful, compassionate plan.
Names helped, but only because they led to action. We learned to treat classification and staging as a map, not a verdict. A skilled ultrasound or MRI can aid the team. Surgical photos and reports keep stories straight between clinics. Pelvic floor therapy, pacing, sleep, and nutrition are not extras. They are the scaffolding that holds you while medicine does its work.
Goals matter more than rules. Protecting organs, reducing pain, and preserving fertility do not always point in the same direction, so your plan needs to fit this season of your life. That might mean targeted suppression for a time, or a thoughtful excision with the right colleagues in the room. It might mean saying no to repeat procedures that cost more than they give.
We also learned to read red flags without panic. Cyclical bowel or urinary symptoms deserve urgent attention and a team that handles complex disease safely. Heavy, clotted periods and a deep, diffuse ache can point to adenomyosis that changes choices. Nothing about this is your fault. Nothing about this is imaginary. You deserve care that takes your pain seriously and your hopes even more seriously.
What finally steadied us was rhythm. We tracked symptoms on a simple map, circled the worst days, and planned work and rest around them. I softened mornings, handled errands, and kept our home office quiet so she could protect her energy without apology. On the hard days, we shrank our world and kept our love big. On the better days, we let joy back in.
If you are at the start, begin small and concrete: map your symptoms, ask for targeted imaging, gather every record, learn the red flags, and write your questions before every visit. If you are in the middle, ask whether the current plan is still serving the goals you set. If you are recovering, give healing the time and tenderness it asks for.
In the end, understanding the types of endometriosis gave us language, but it was steady advocacy, kind pacing, and the right team that gave us our life back. I cannot promise it will be easy. I can promise that your pain has a name, your story matters, and there is a next step worth taking today.
Your pain is real, your story is valid, and a precise, compassionate plan can change everything. Map symptoms, ask for targeted imaging, keep your records, and build a team that listens. You do not have to do this alone. Start small today. Hope grows when action and kindness meet.
Have a question or a piece of your story to share? Leave a comment below, and grab a free chapter of my eBook “Endo-Tool: Endometriosis for Men.” You’ll also join our community for more freebies, big discounts on all our books, and honest, practical emails that help you both adjust to a new normal.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MORETypes of Endometriosis FAQ
1) What are the main types of endometriosis?
Clinically, doctors describe three patterns: superficial peritoneal lesions on the pelvic lining, ovarian endometriomas (blood-filled “chocolate” cysts), and deep infiltrating endometriosis that invades tissues beneath the peritoneum and can involve bowel, bladder, or ligaments. Adenomyosis is different—it lives inside the uterine muscle, but commonly coexists.
2) Do the types determine how much pain I’ll feel—or my fertility?
Not reliably. A tiny superficial lesion can be excruciating, while extensive disease can be quiet. That said, ovarian endometriomas may reduce ovarian reserve over time, and deep disease can affect organs (bowel, ureters) and sometimes fertility. The right plan focuses on your goals (pain relief, organ protection, family building), not just a label.
3) How are the types diagnosed—can imaging see them?
Skilled transvaginal ultrasound often detects endometriomas and many deep nodules; MRI with an endometriosis protocol helps map complex sites. Laparoscopy with pathology remains the definitive diagnosis in uncertain cases. There is no single diagnostic blood test. Good imaging plus a careful history usually narrows the picture before any surgery.
4) What if my laparoscopy showed “no endometriosis,” but I still have symptoms?
It happens. Disease can be missed without experienced visualization or when only ablation was done. Symptoms still deserve treatment—targeted imaging, medical therapy trials, pelvic floor physiotherapy, and, if needed, a second opinion with an excision specialist. Your pain is valid even when paperwork is inconclusive.
5) Does each type have a different treatment path?
Treatment is individualized. Some do well with hormonal suppression and pelvic floor therapy; others—especially with deep disease or organ risk—need meticulous excision, sometimes with colorectal or urology colleagues. Endometriomas require a careful balance between symptom relief and preserving ovarian reserve. The best plan fits your season of life.
Types of Endometriosis References
- https://www.endometriosis-uk.org/what-is-endometriosis
- https://www.endometriosis-uk.org/sites/default/files/2025-01/Understanding%20endometriosis%20updated%20Jan%202025.pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9918005/
- https://www.nature.com/articles/s44294-024-00052-w
- https://my.clevelandclinic.org/health/diagnostics/21814-endometriosis-ultrasound
- https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661
- https://www.pelvicpain.org.uk/conditions/deep-endometriosis/
- https://www.who.int/news-room/fact-sheets/detail/endometriosis