Treatment of Endometriosis
What truly works when pain keeps derailing your life and fertility hopes when it comes to the treatment of endometriosis?
The treatment of endometriosis combines pain control, hormonal suppression, and surgery tailored to symptoms and fertility goals. Care often starts with NSAIDs and hormones; if these fail or deep disease exists, laparoscopic removal of lesions may be offered by an experienced specialist team.
Alongside familiar choices like combined oral contraceptives, progestins, and GnRH agonists, newer oral GnRH antagonists have widened options. In 2025, NICE recommended relugolix combination therapy and later linzagolix for selected patients in England, offering convenient take-at-home alternatives.
Current guidance still emphasizes matching care to pain drivers, disease location, and pregnancy plans, and using surgery judiciously within a multidisciplinary approach.
I’ve watched my wife fight through endometriosis pain on days when simply sitting upright felt like an achievement. Every decision, medicine, diet, and surgery has been about giving her back ordinary moments and protecting our hope for the future.
If you’d like a compassionate, practical companion for your partner, grab a free chapter of my “Endo-Tool: Endometriosis for Men.” By joining, you’ll also become part of our community where I share more freebies, meaningful support, and big discounts on all our books to help you both adjust to the new normal with confidence and care.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis, and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men

Treatment of Endometriosis
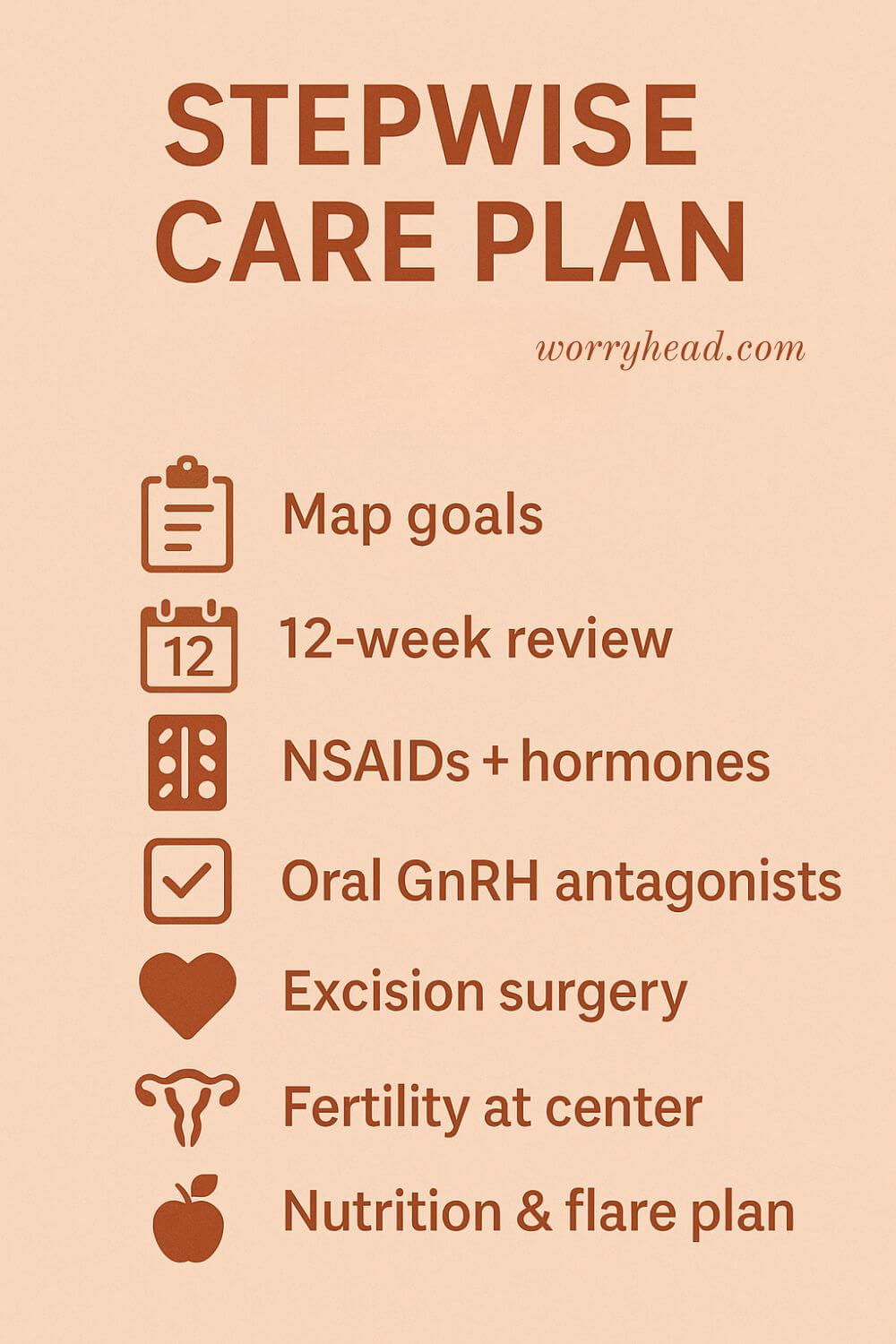
Most care starts simple and builds only as needed. You begin by naming the pain: period pain, ovulation pain, bowel or bladder pain, because patterns point to which levers to pull first. Then you and your clinician map goals: pain control now, fertility later, or both. That clarity keeps choices compassionate and strategic, not chaotic.
First-line options usually pair an anti-inflammatory plan with cycle suppression. Combined pills, progestin-only pills, depot progestins, or a levonorgestrel IUD can thin or quiet endometrial-like tissue, often easing cramps and heavy bleeding. If NSAIDs aren’t touching flare days, it’s a signal to adjust hormones, not a sign you’re “failing”.
In 2025, the NHS added a genuine step-change: daily oral GnRH antagonist therapy. Relugolix with add-back oestrogen and norethisterone (Ryeqo) became available for selected adults whose symptoms persist after standard options. It offers clinic-free dosing and faster on/off titration than injections. Linzagolix followed in June 2025 for similar candidates, expanding choice. These are not “forever drugs,” but time-limited tools that can break a pain spiral.
If hormones don’t line up with your goals or deep disease drives bowel, bladder, or nerve pain, surgery enters the conversation. Excision performed by an experienced team can reduce pain and improve function, especially for deep-infiltrating lesions or endometriosis cysts on the ovary. The decision is never only about what’s seen on a scan; it’s about symptoms, life plans, and who’s on your surgical bench.
Fertility plans shape every fork in the road. Suppression helps pain but prevents conception; excision may help some couples move sooner toward trying, expectant management, or IVF. The right choice weighs stage and site of disease, age, ovarian reserve, and the very human limits of waiting.
Whole-pelvis care matters. Pelvic floor physical therapy can calm guarding and dyssynergia; GI and urology input can untangle endometritis, pelvic inflammatory disease sequelae, or adenomyosis that mimic or magnify symptoms. Central nervous system sensitization is real; multimodal pain medicine and paced rehabilitation build capacity without gaslighting your pain.
Lifestyle won’t cure the disease, but it can lower the volume. Some people find anti-inflammatory eating patterns, turmeric for endometriosis adjuncts, or heat and movement routines nudge bad days into tolerable ones. Use diet and supplements as supportive scaffolding, never as a substitute for evidence-based care.
In short, the treatment of endometriosis is a personalized, stepwise partnership matching therapies to symptoms, goals, and timing, then revisiting as your life changes. What helped your endometriosis last year might not be what serves you now, and that’s okay. Good care evolves.
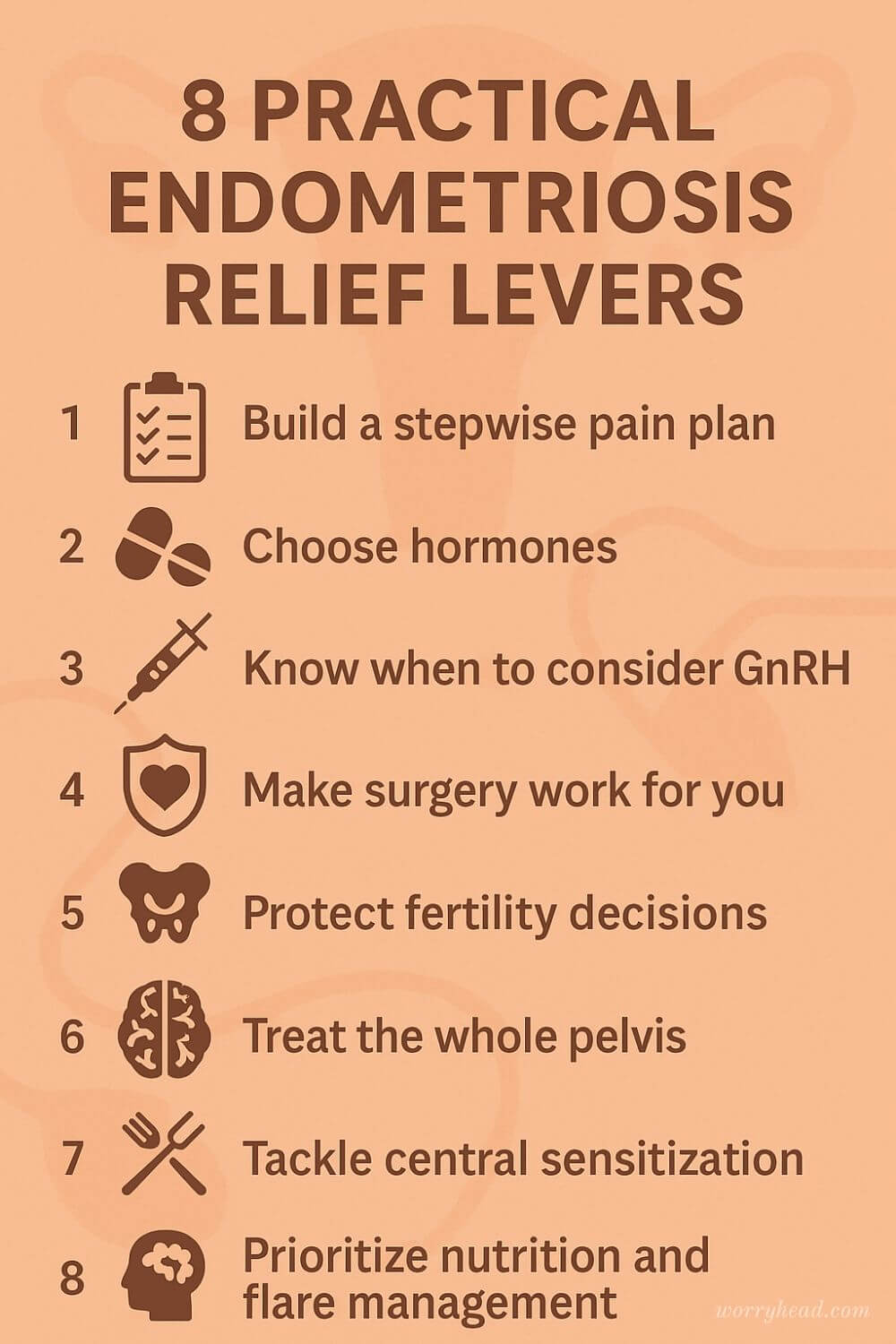
When my wife and I finally had a plan that respected her pain and our hopes, the room felt lighter. We stopped chasing “perfect” and started choosing “useful for this season.” Below are the practical levers we kept returning to, the ones we wish we’d had on a single page at the start.
- Build a stepwise pain plan
- Choose hormones strategically
- When to consider GnRH
- Make surgery work for you
- Protect fertility decisions
- Treat the whole pelvis
- Tackle central sensitization
- Nutrition and flare management
Build a Stepwise Pain Plan
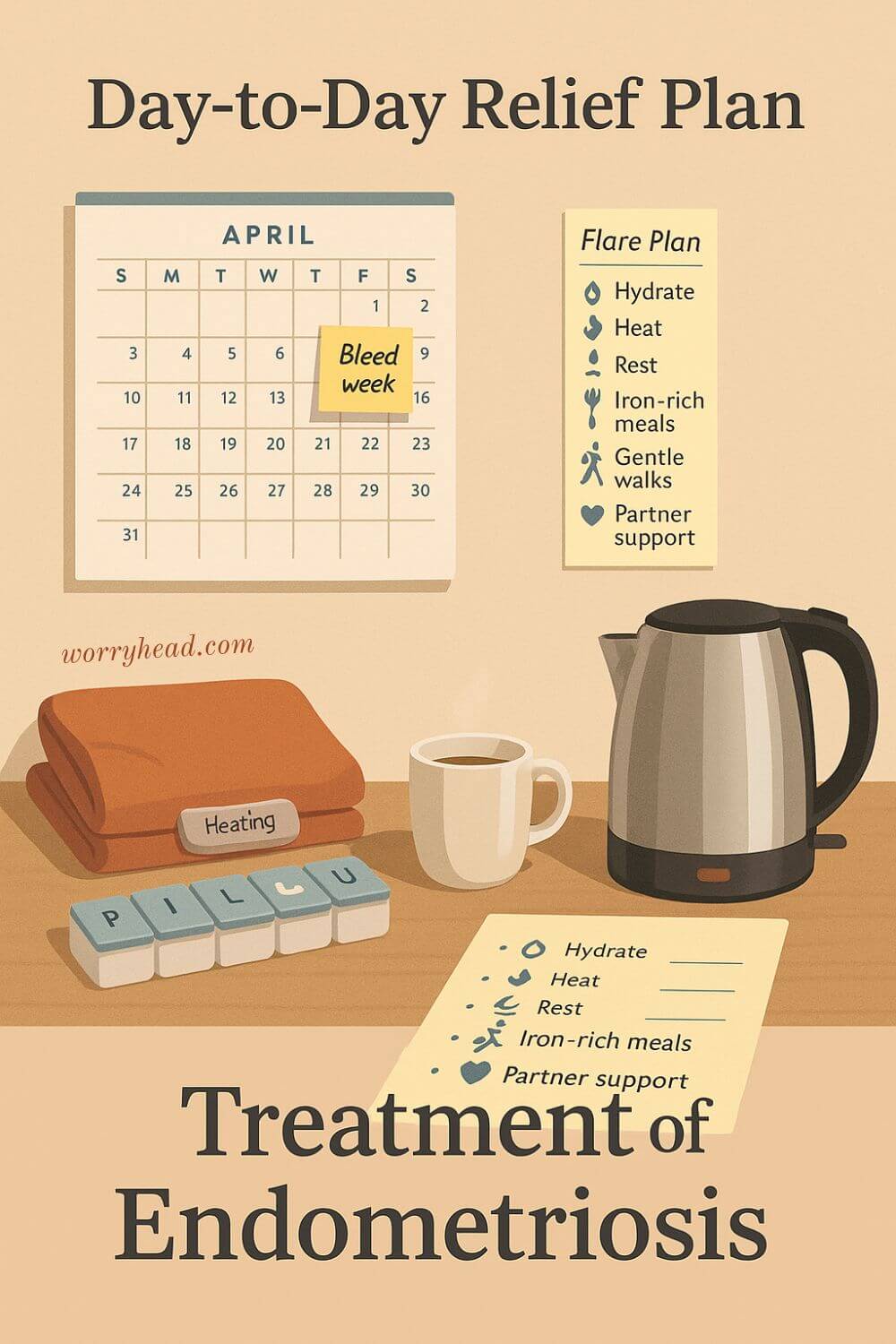
Start by mapping pain types, timings, and triggers, then write a simple ladder you can climb only when needed. Level one might pair NSAIDs timed before bleeding with heat, bowel support, and gentle mobility on flare days. Level two adds a short course of stronger analgesia agreed with your clinician, plus rest plans that protect work and family life.
Keep a one-page flare script so no one is guessing at 2 a.m. Note when pain breaks through, what helped, and what side effects showed up. Share this log at reviews so tweaks are based on evidence, not memory.
Add pelvic floor care early since guarding can amplify cramps. Track sleep and stress since both change thresholds. We learned that naming the plan out loud calms panic, and that calm buys room for better choices.
Build safety lines too. Write red flags that mean urgent care, such as sudden new severe pain, fainting, or fever. When the rules are clear, you do not have to be brave every minute, only honest about what your body is saying.
Choose Hormones with a Clear Strategy
Cycle suppression is not one size fits all, so pick a goal, then the tool. For heavy bleeding or cyclical cramps, combined pills in extended cycles or progestin-only options can quiet activity and shorten bad weeks. A levonorgestrel IUD may lighten periods and reduce pain once settled, while depot progestins suit those who prefer not to take a daily pill.
Test one approach for a clear window, usually three months, while tracking pain, bleeding, mood, and headaches. If cramps worsen or bleeding becomes unpredictable, it is data, not failure, and the plan can shift route or dose.
Discuss migraines, clot risk, and bone health before you start. If intimacy pain or spotting persists, consider a different formulation or delivery method, not just more of the same.
We found that choosing on purpose, with criteria and a review date, felt empowering. The question changed from “why is this happening” to “does this meet the target we set,” which is a kinder way to live.
Know When to Consider GnRH
When standard hormones cannot create breathing space, short-term GnRH therapy can be a bridge. Antagonists taken by mouth or agonist injections like zoladex quiet ovarian signaling, often lowering pain intensity and bleeding. Add-back therapy protects bone and mood while keeping benefits, and the on-off switch is quicker with oral agents.
Agree on a time limit, monitoring, and what this phase unlocks, such as rehab, a return to work, or preparation for excision of endometriosis. Side effects like hot flushes, sleep change, and low libido deserve proactive care plans, not stoicism.
Bone health, migraine history, and mental health guide dosing and duration. Keep calcium, vitamin D, and weight-bearing movement on the checklist from day one.
For us, the value was clarity. A defined season of quiet lets pain settle, the nervous system breathe, and decisions about surgery or fertility happen without the drumbeat of constant flare.
Make Surgery Work for You
Surgery is a tool, not a verdict, and the details matter. Ask about excision rather than burning off endometriosis, the plan for deep infiltrating disease, and how bowel, bladder, or nerve involvement will be handled if found. For an endometriosis cyst, discuss preserving ovarian tissue while removing the capsule fully.
Request a written aim, risks, and alternatives, including what happens if adenomyosis or pelvic inflammatory disease scarring is suspected. Prehab helps with iron if you are anaemic, bowel prep guidance if needed, and pelvic floor strategies to reduce guarding after.
One operation with the right team can be kinder than multiple laparoscopies for endometriosis with partial results. Insist on a post op plan that covers pain, hormones, and when to try for pregnancy or move toward IVF.
We learned to ask for operative photos and a plain language debrief. Understanding what was found turned fear into agency, and agency into better healing.
Protect Fertility Decisions from the Outset
Pain plans and pregnancy hopes can live in the same room when you design them together. Stage does not map perfectly to fertility, so combine symptoms, ultrasound, and ovarian reserve tests when choosing a path. If an endometriosis cyst needs removal, talk through techniques that protect ovarian tissue.
Decide on timelines you can live with, not ones built on pressure. Some couples try after excision, others move directly to assisted reproduction, and both choices are valid. Age, reserve, and the weight of waiting inform the route more than any single label.
Fertility preservation can be part of the conversation for those facing repeat surgery or extensive disease. A referral early does not commit you to treatment; it keeps options open.
What steadied us was having a Plan A and a Plan B on paper. Hope felt less fragile when it had structure, milestones, and a next step if the first door did not open.
Treat the Whole Pelvis Well
Pain is not only in lesions; muscles, nerves, and organs join the choir. Pelvic floor physiotherapy can soften guarding, improve bowel and bladder habits, and reduce dyspareunia with gentle, paced work. Breathing patterns and posture affect pressure in the pelvis more than most of us realise.
Screen for neighbours that mimic or magnify endometriosis symptoms, such as irritable bowel, endometritis, or interstitial cystitis. A simple bladder and bowel diary can reveal patterns that pain fog hides.
Dilators, lubricants, and consent-based touch retrain the system safely. Sexual pain deserves care that protects intimacy rather than avoiding it out of fear.
When the team speaks to each other, the pelvis feels less like a battlefield. Coordination turned our chaos into care that flowed, and that flow reduced pain without adding more medicine.
Tackle Central Sensitization with Gentleness
Chronic pain can teach the central nervous system to sound alarms faster, so part of the relief is turning down the gain. Pain education, paced activity, and graded exposure rebuild trust in movement without invalidating the pain. Good sleep, nutrition, and steady routines lower background noise so flares do not dominate.
Anxiety, depression, and OCD can grow in the soil of constant pain, so bring mental health into the plan with the same respect as medication. Approaches like CBT or ACT teach skills for difficult days, and they work alongside medical treatment, not against it.
Non opioid multimodal care, such as neuropathic agents, topical options, and mindful breathing, gives more keys for different locks. Celebrate small wins because small wins change trajectories.
In our house, compassion was the strongest analgesic. When the goal shifted from zero pain to more life inside the pain, freedom started to return.
Prioritize Nutrition and Flare Management
Food does not cure disease, yet a calm gut steadies the whole system. Many do well on an anti-inflammatory pattern rich in plants, omega-3s, and steady protein, while easing ultra-processed foods that drive swings. Track personal triggers since endometriosis and the bowel have a loud conversation.
If periods are heavy, ask about iron testing and ways to protect energy. Gentle movement, heat, and hydration during flares create margin, and turmeric for endometriosis as an adjunct may help some, though it is not a replacement for treatment.
Plan work, childcare, and rest around predictable storm windows. A ready bag with pads, heat packs, and rescue meds reduces panic when symptoms surge.
What helped us most was permission to plan for pain without shame. Prepared does not mean defeated; it means you kept a promise to your future self.
Make the Treatment of Endometriosis Truly Personal
Personal care starts with a map you can read on the worst day. We write goals in plain language: less bleeding, better sleep, intimacy without fear. Then we choose the treatment of endometriosis that fits those goals for the next 12 weeks, not forever.
At home, we keep a one-page tracker for pain, bleeding, bowels, mood, and side effects. Every Friday, we glance at it together and mark, keep, tweak, or stop. This tiny ritual, done at the kitchen table with tea, turns guessing into decisions.
Side effects get their own plan, so they do not quietly end the therapy. If bone health is on the table, we agree on vitamin D, calcium, and weight-bearing days, plus a review date for scans when appropriate. If headaches or low mood appear, we phone sooner instead of soldiering on.
Surgery prep is the same kind of kindness. We ask for expected findings, photos, and a plain summary, then set a post-op script for pain control, hormones, and pelvic floor resets. Having these printed on the fridge protects recovery from panic and fog.
Most of all, we build a life around flare windows: meal kits for a period week, a flexible work schedule, and code words that mean I’m here and you’re safe. I remember the night she whispered, “I can’t be brave every day,” and we agreed that real bravery is asking for help and planning so tomorrow hurts a little less.
Living with the Treatment of Endometriosis Day to Day
Mornings start with a simple check-in and the pill box that sits beside the kettle. We time medicines with breakfast, note side effects, and leave sticky notes that say what needs watching today.
On bleed days, we switch to slower routines, extra hydration, and clothes that don’t fight the belly. Work bends to health, not the other way round, so the calendar carries flexible blocks and quiet hours. Her chair, heat pad, and footrest are not luxuries; they are the difference between coping and crashing.
We treat food as fuel, prepping iron-rich meals before period week so energy doesn’t fall off a cliff. Intimacy stays tender because pain can arrive without warning, so we use soft language, options, and the right to pause without guilt. When fear climbs, we return to breath work and the plan on the fridge, because certainty eases the nervous system’s grip.
The treatment of endometriosis is not only what happens in the clinic; it is how a couple protects hope on ordinary Tuesdays. I keep my own guardrails too, walking at dusk, writing down what scared me, and asking for help before I burn out.
Together we celebrate tiny wins, like a commute-free day or a night without cramps, because stacking good moments changes the slope of the month. None of this is heroic; it is just love with a schedule and a promise to choose each other when pain tries to choose for us.
Conclusion On the Treatment of Endometriosis
Care works best when it honours the person who lives inside the pain. Labels, stages, and scans matter, yet the real progress begins when you and your clinician agree on simple goals that you can test in the real world. Relief is rarely a single leap. It is a series of small, deliberate steps that you adjust as life changes.
Start with a clear plan for pain, sleep, bleeding and energy. Track what helps and what hurts, then review on a timetable you can keep. This turns rough weeks into information rather than defeat. One change at a time is kinder on the body and clearer on the mind.
Hormonal choices are tools, not verdicts. If a pill unsettles mood or bleeding, that is data for a different option, not a reason to carry on in silence. Short seasons of more advanced therapy can create space to rehabilitate, reconnect, and think again. Know the exit before you enter, and set a review date you both respect.
Surgery deserves the same clarity. Ask who will be in the room, what they plan to do, and what the plan becomes if the findings change. Excision in skilled hands can be life-changing, but it still needs a post-op script for pain, hormones, bowel and bladder habits, and intimacy. Healing accelerates when everyone is reading the same page.
Fertility plans belong at the centre, even when you are focused on today’s pain. Map timelines you can live with. Some couples try after surgery. Others move to assisted reproduction. Both paths are valid. What matters is informed choice, supported by tests and by compassion for the weight of waiting.
The pelvis is a network. Muscles, nerves, and organs influence each other, so bring pelvic floor therapy, bowel and bladder care, and gentle conditioning into the plan. Central sensitisation does not mean your pain is imagined. It means your system is faithful to what it has learned. With patience and practice, one can learn something kinder.
Lifestyle will not cure disease, yet routines can soften the edges. Food that steadies the gut, movement that respects fatigue, and rest that is scheduled rather than stolen all add up. Tiny wins, counted honestly, change the month more than rare, heroic days.
Most of all, make this a partnership. In our home, we stopped chasing perfection and started choosing what is useful for this season. We wrote it down, we reviewed, we forgave the hard days, and we celebrated the ordinary ones. The treatment of endometriosis is not only medicine. It is a way of protecting hope while you build a life that pain does not get to run.
Healing is built, not found. Choose one next step, write it down, and review it on a date you set today. Protect sleep, schedule rest, and ask for help sooner than you think you should. Small, honest changes repeated with care can return more life than any single dramatic decision.
If this resonated, leave a comment to share your journey, and grab a free chapter of my “Endo-Tool: Endometriosis for Men.” It is my gift to you, and a gentle doorway into a community that will keep you supported when the days feel heavy.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MORETreatment of Endometriosis FAQ
1) What is the best treatment for endometriosis?
There isn’t one “best.” Good care is stepwise and personal: targeted pain relief, hormonal suppression to quiet cycles, and—when symptoms or goals call for it—excision of endometriosis by an experienced surgeon. Plans change with life stage, fertility hopes, side effects, and how your body actually responds. In our home, reviewing progress every 8–12 weeks kept choices kind and clear rather than all-or-nothing.
2) Will surgery cure my endometriosis?
Surgery can be transformative, especially meticulous excision for deep disease or an endometriosis cyst, but it’s not a guaranteed cure. Results hinge on surgeon skill, disease location, and what happens after—hormonal strategy, pelvic floor rehab, and flare management. One thorough operation with a clear post-op plan is usually better than multiple laparoscopies that only burn the surface and leave pain drivers behind.
3) Can I still get pregnant with endometriosis?
Many do. Fertility depends on age, ovarian reserve, disease site, and time trying. Excision may improve pain and sometimes natural conception, but some couples benefit from moving sooner to assisted reproduction. If you’re trying and months keep slipping by, get individualized advice early rather than waiting in worry. Protecting ovarian tissue during surgery and planning timelines you can live with matter more than any single “stage” label.
4) Is there a blood test or scan that proves I have it?
No single blood test confirms endometriosis. Markers like CA-125 can rise for many reasons. Ultrasound can spot ovarian endometriomas and suggest deep lesions; MRI can map complex disease; yet some lesions hide. Many clinicians treat based on symptoms and imaging while reserving laparoscopy for when it will change management. The goal is diagnosis that actually unlocks the right help, not procedures for their own sake.
5) Do diet or supplements help—and which ones are safe?
Food and supplements won’t cure disease, but an anti-inflammatory pattern, iron support if bleeding is heavy, and gentle movement can lower the “volume” of bad days. Some people find turmeric helpful as an adjunct, while others notice triggers in ultra-processed foods. Treat these as supportive tools alongside evidence-based therapies, and sense-check everything with your clinician to avoid interactions with hormonal medicines or pain regimens.
Treatment of Endometriosis References
- https://www.nice.org.uk/guidance/ta1057
- https://www.nice.org.uk/guidance/ta1067
- https://www.nice.org.uk/news/articles/first-daily-pill-for-endometriosis-approved-for-nhs-use
- https://www.england.nhs.uk/2025/05/new-endometriosis-pill-on-the-nhs-could-benefit-more-than-1000-women-a-year/
- https://www.nhs.uk/conditions/endometriosis/
- https://www.mayoclinic.org/diseases-conditions/endometriosis/diagnosis-treatment/drc-20354661
- https://my.clevelandclinic.org/health/diseases/10857-endometriosis
- https://www.aafp.org/pubs/afp/issues/2022/1000/endometriosis.html
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12239828/
- https://www.dovepress.com/oral-gnrh-antagonists-in-combination-with-estradiol-and-norethindrone–peer-reviewed-fulltext-article-IJWH
- https://www.uclh.nhs.uk/our-services/find-service/womens-health-1/gynaecology/endometriosis/medical-treatment-endometriosis
- https://www.nhsinform.scot/healthy-living/womens-health/girls-and-young-women-puberty-to-around-25/periods-and-menstrual-health/endometriosis/