Fertility and Endometriosis
When it comes to fertility and endometriosis, what’s the real chance of becoming a parent if this disease keeps getting in the way?
Endometriosis raises the risk of subfertility (roughly 2–4×), yet many still conceive, about 60–70% over time, especially with mild disease. Mechanisms include inflammation, adhesions, and ovulatory effects; stage, age, and co-factors guide whether expectant care, surgery, or ART best optimise outcomes.
Here’s what surprised me as I dug into the latest data: in a real-world longitudinal cohort, preliminary pregnancy rates were ~11% per natural cycle in moderate/severe disease and ~22% per cycle with assisted reproduction, showing why early referral matters if months keep slipping by.
Expert groups also stress that many with mild–to–moderate disease still conceive naturally, and that choices like timed intercourse, IUI, IVF, or selective surgery should be tailored rather than one-size-fits-all. The 2022 European guideline ties these decisions to age, ovarian reserve, disease distribution, and your timeline to parenthood.
I’ve watched my wife battle pain that steals sleep and plans, yet we’ve learned that hope is not naive; it’s a strategy. If you’re reading this with a lump in your throat, you’re not alone here.
If endometriosis is shaping your relationship, you can grab a free chapter of my “Endo-Tool: Endometriosis for Men.” By joining, you’ll also step into our community, where I send more freebies, big discounts on all our books, and practical emails that help couples adjust to the new normal without losing each other along the way.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis, and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men

Fertility and Endometriosis
When doctors talk about timelines, they aren’t just being clinical; they’re protecting your chances. Age, stage, ovarian reserve, and months already spent trying all bend the odds, and each one can be measured and acted on rather than left to hope.
ESHRE’s 2022 guideline leans into this individualised plan: confirm disease with expert imaging when possible, weigh expectant management against IUI or IVF, and use surgery selectively when it’s likely to improve conception, especially with deep disease or painful endometriomas.
I’ve seen how inflammation, adhesions, and distorted anatomy can make “how to get pregnant with endometriosis” feel like a riddle with missing clues. But there are clues, cycle tracking, mid-luteal progesterone, AMH, AFC, and a good ultrasound tell a story that helps you choose the next best step instead of spinning in circles.
For some couples, a few more natural cycles with timed intercourse or IUI make sense; for others, IVF moves the needle faster, especially when months matter more than anything. Recent evidence suggests implantation can be lower in IVF when endometriosis is present, yet live-birth rates may still match other causes across multiple cycles, a context you deserve to hear so you can plan with clear eyes.
When pain flares, sleep fragments, and sex hurts, “Does endometriosis make it harder to get pregnant?” stops being theoretical. It lands in your kitchen at 2 a.m., when you’re holding a hot water bottle and Googling success stories.
Guidelines in the UK now emphasise earlier referral to fertility pathways when pregnancy is a priority, and they’ve updated surgical recommendations so the decision to operate is tied to your goals, not just your symptoms.
Endometriomas are their own chapter. Sometimes they’re observed; other times, size, pain, or access to follicles pushes toward surgery, balancing ovarian tissue preservation against surgical benefit. And while new take-home pills are expanding pain options on the NHS, they suppress ovulation, great for symptoms, not for trying to conceive, so timing treatments around your family plans really matters.
Lifestyle isn’t a magic wand, but it’s not nothing either. Endocrine-disrupting exposures, high-temperature work environments, or air pollution may chip away at outcomes, especially in assisted reproduction; choosing cleaner air days for retrieval or transfer and supporting sleep, nutrition, and movement are small levers worth pulling.
I’ve walked beside my wife through scans and second opinions, through months that felt wasted and through plans that finally made sense. If you’re reading with wet eyes, know this: you’re not broken, and you’re not late, you’re strategic.
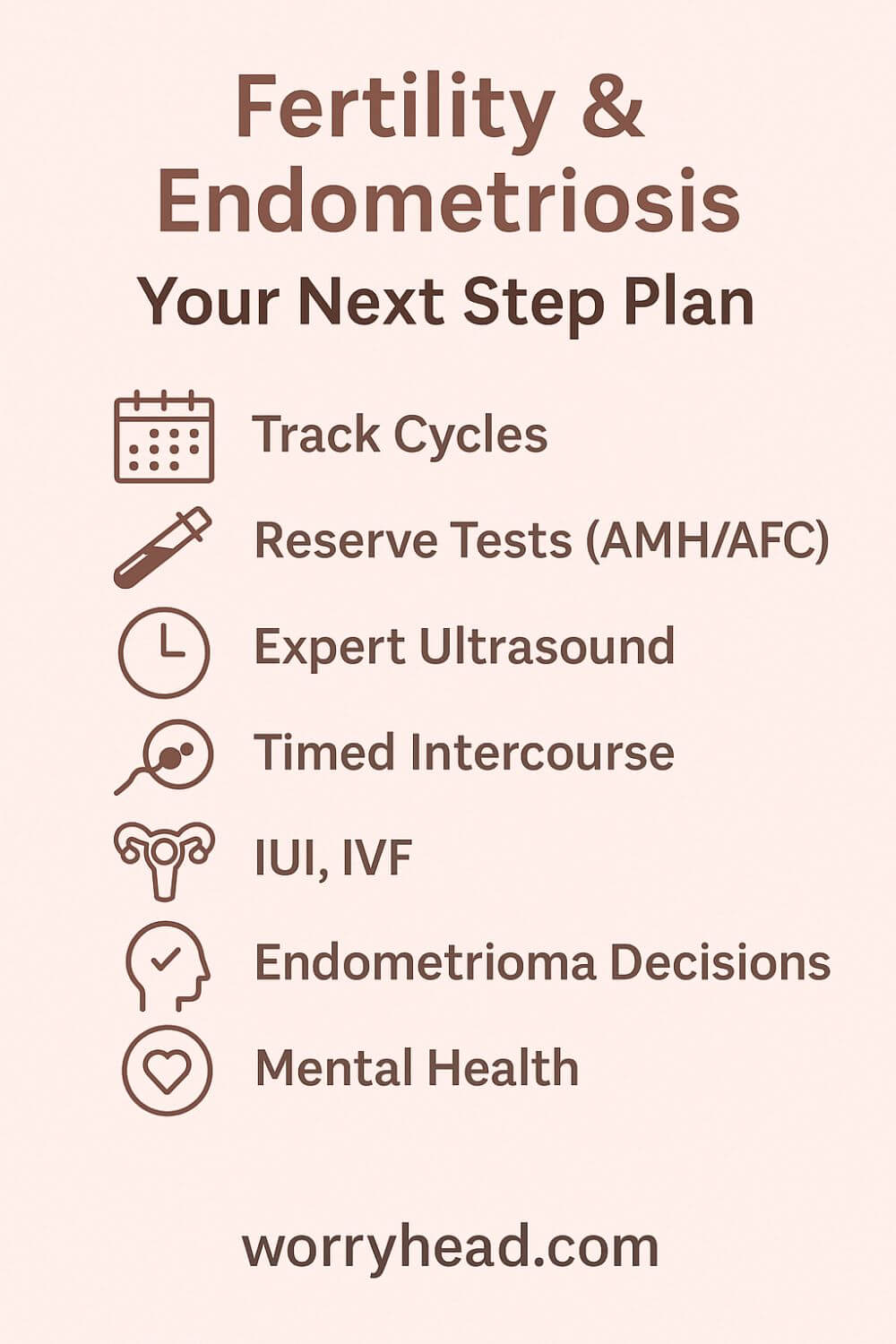
Next, I’ll share the practical, lived-through tips we wish we had at the start:
- Track cycles like a scientist
- Test ovarian reserve early
- Use an expert pelvic ultrasound
- Time intercourse with intent
- Decide when to try IUI
- Know when IVF saves time
- Weigh endometrioma surgery
- Protect mental health together
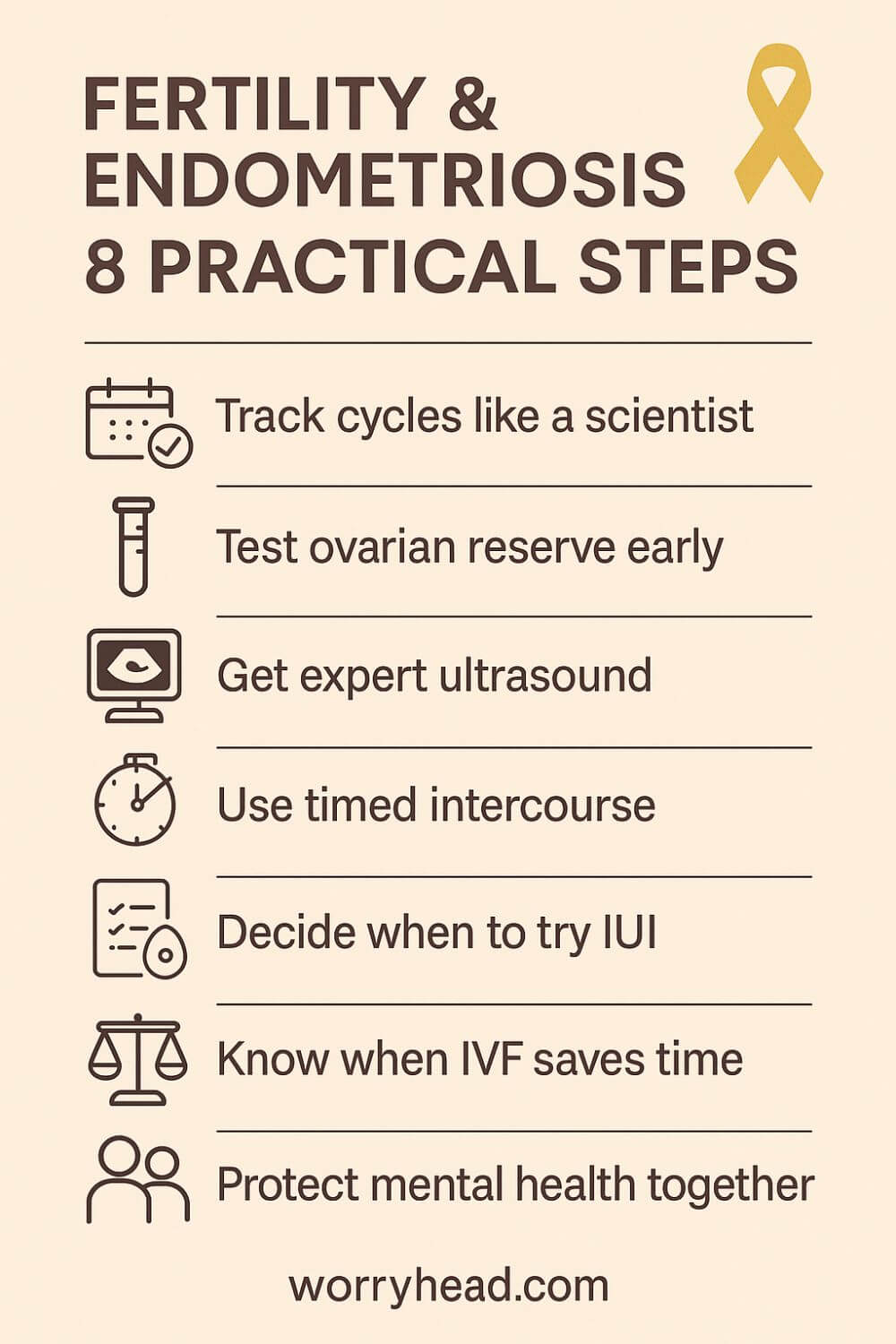
Track Cycles Like a Scientist
Cycle data turns anxiety into information. Start with simple, consistent tracking of bleeding, pain, cervical mucus, and mid-cycle twinges, then layer in ovulation prediction kits and mid-luteal progesterone when needed. Two to three months of clean notes can reveal whether ovulation is regular and if the luteal phase is long enough to welcome an embryo.
When you’re trying to get pregnant with endometriosis, clarity eases the pressure between you. We treated charting like a shared project: gentle check-ins, not score-keeping. Patterns guided timing, flagged red-letter pain days to skip, and gave doctors specifics instead of guesswork. Data won’t fix everything, but it will stop you feeling lost.
Test Ovarian Reserve Early
AMH and antral follicle count aren’t crystal balls, but they do anchor decisions to reality. An early snapshot of ovarian reserve helps you decide whether to continue naturally, try IUI, or move to IVF before months slip by. It also frames the best age to get pregnant with endometriosis as a conversation about you, not averages.
We learned to treat results with compassion. A “lower than expected” AMH is not a verdict; it’s a nudge to choose faster paths. If AMH is steady and AFC reassuring, you may buy time for conservative steps. If not, acting now can protect tomorrow’s chances. Either way, numbers reduce regret.
Use an Expert Pelvic Ultrasound
Not all scans are equal. An expert pelvic ultrasound can map deep disease, identify endometriomas, and show if organs are stuck together by adhesions that complicate conception. That map changes everything: it tells you whether surgery could help, or whether IVF bypasses obstacles better.
For us, the first high-quality scan felt like switching on a light. Suddenly, “why is this taking so long?” had anatomy behind it. If you’re wondering if endometriosis can affect ovulation or tubal movement, imaging is how you stop wondering. Find a sonographer who sees endometriosis every day. Precision saves time and heartache.
Time Intercourse with Intent
If you’re asking how to get pregnant with endometriosis naturally, precision beats pressure. Aim for the two days before ovulation plus ovulation day, guided by LH surges and your cycle maps. Keep it kind to the body: when pain is high, skip and protect intimacy in other ways.
We learned to separate love from logistics. A plan set in calm daylight made evenings gentler. Short fertile windows are not moral tests; they’re just physiology. If cycles look erratic, consider a few monitored cycles to confirm ovulation and adjust timing. Small changes in when you try can yield big differences in odds.
Decide When to Try IUI
IUI can help when semen parameters are borderline or when you want to stack the deck in cycles that otherwise look healthy. It places washed sperm closer to the egg and pairs well with careful ovulation triggering. The question isn’t whether you can still get pregnant with endometriosis, but whether IUI increases the probability enough for you right now.
We treated IUI as a time-boxed trial. Two to three well-timed attempts can be sensible when tubes are open and pain is manageable. If results stall, you haven’t failed; you’ve gathered evidence for the next step. Your timeline matters as much as the technique.
Know When IVF Saves Time
IVF sidesteps many barriers: distorted anatomy, mild tubal factors, and even some ovulatory issues. For the endometriosis effect on pregnancy rates, the first cycle can look average, while cumulative live-birth across cycles levels the field. If months already feel heavy, IVF can compress uncertainty into a plan with checkpoints.
What helped us was reframing IVF as an efficiency tool, not a last resort. With endometriosis, what are the chances of getting pregnant become less abstract when fertilisation and embryo development are visible. If reserve is tight or age is pressing, earlier IVF may be the most loving choice for your future self.
Weigh Endometrioma Surgery
Endometriomas are complicated houseguests. Large or painful cysts can block follicles, hide eggs at retrieval, or hurt quality of life. Surgery may help, but it can also trim ovarian reserve. The decision is not “operate or not” but “operate when the benefit clearly outweighs the loss.”
We sought surgeons who treat fertility like a co-pilot, not an afterthought. If a cyst hinders access or poses an infection risk, careful excision by an expert can clear the runway. If it sits quietly, monitoring may protect follicles for IVF. Ask bluntly about technique, experience, and how many eggs they’d expect you to keep.
Protect Mental Health Together
Hope is a muscle, and endometriosis can exhaust it. Protect sleep. Keep pain plans ready. Set boundaries with unhelpful advice. Therapy, peer groups, and honest check-ins keep love from being crowded out by logistics. Trying to get pregnant with endometriosis is hard enough; you don’t need to do it in silence.
We built tiny rituals: walks after appointments, no-fertility Sundays, permission to cry without fixing. Your relationship is not a fertility tool; it’s the home you’re inviting a child into. Guard it. Healing isn’t linear, but connection can be.
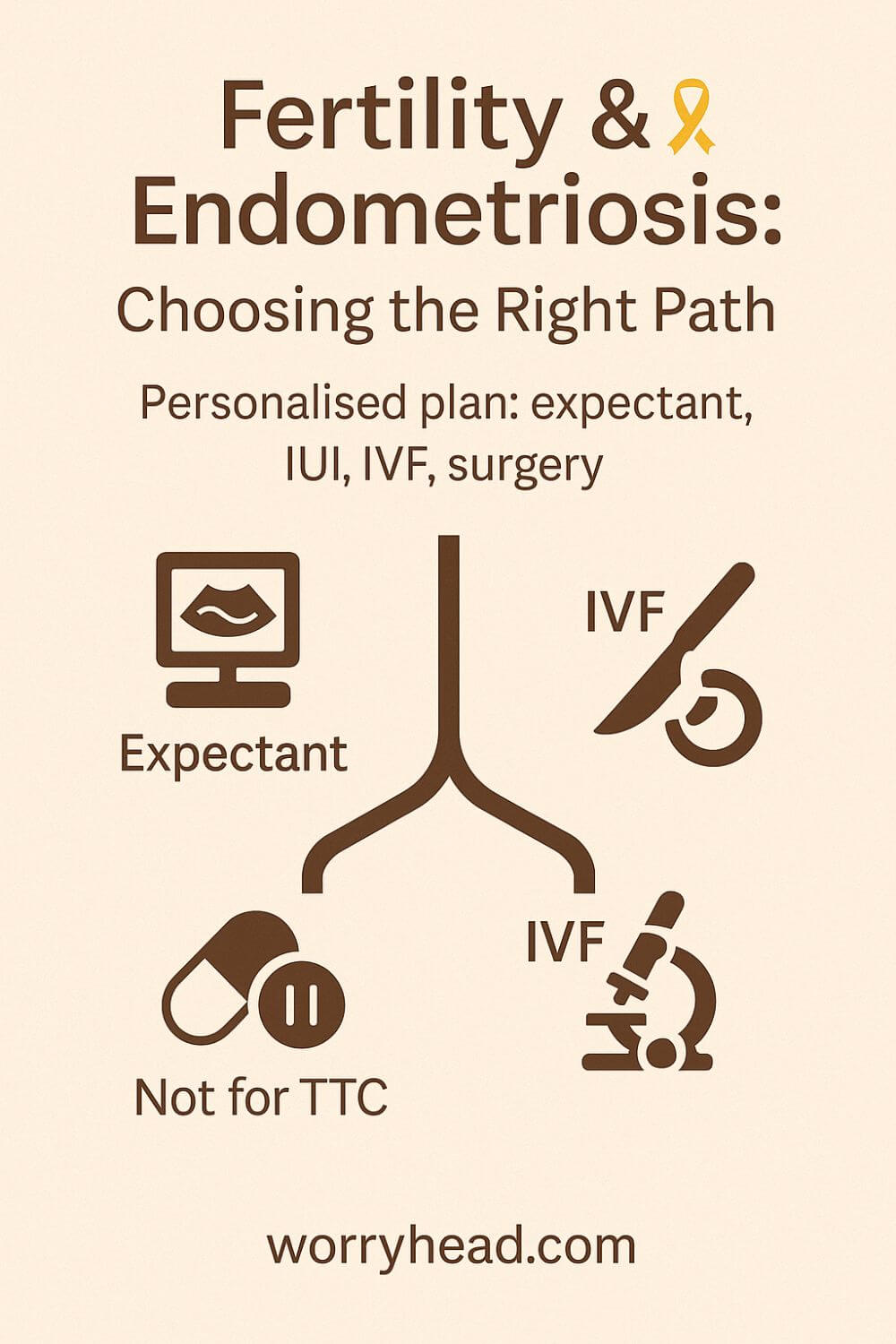
How to Deal with Fertility and Endometriosis
The fork in the road is real: keep trying naturally a little longer, or step onto a fertility pathway with monitoring, IUI, or IVF. Good care doesn’t guess, it personalises the route using age, ovarian reserve, disease map, and how long you’ve already been trying. That’s the spirit of modern guidance, which ties decisions to your goals and timeline rather than a one-size approach.
When deep disease or endometriomas are in the picture, many couples ask whether surgery first will boost IVF results. Recent analyses suggest that routine surgery before IVF rarely improves live birth and can trim ovarian response, so the question becomes access, pain, and infection risk, not reflex removal. This is where an expert scan and a surgeon who respects eggs as much as anatomy matter.
If you do proceed to IVF, expect some mixed headlines. Several studies show lower implantation in the first cycle for those with disease, yet cumulative outcomes across multiple cycles can narrow the gap, evidence that perseverance with a smart plan pays off. Knowing this upfront protects you from panic after a single result.
Pain control also needs fresh thinking when pregnancy is the goal. New NHS-approved daily pills can calm symptoms, but they suppress ovulation, so they’re tools for symptom seasons, not for conceiving months. Planning when to use them and when to pause keeps treatment from stealing your window.
I’ve watched my wife grit her teeth through scans, hold my hand during hard conversations, and still find a way to laugh on clinic days. On the nights when hope felt thin, we came back to this: the plan is not a verdict; it’s a bridge. And every careful step, test, timing, and choice was love in motion.
If you’re standing at this fork, take a breath. Get the best imaging you can. Ask blunt questions about surgery trade-offs.
Consider time-boxed trials of IUI. And if IVF is the straightest line to the family you want, step onto it without shame; strategy is not surrender.
More on Fertility and Endometriosis
There’s a moment when tenderness has to share the room with tactics. We learned to plan pain relief without muting ovulation, to choose imaging that answers questions, and to move quickly when the calendar, not just the disease, was the loudest voice. Modern guidance backs that calm urgency: tailor choices to age, reserve, disease map, and how long you’ve already tried.
When hormones soothe pain, they also pause ovulation; that’s mercy for symptoms, but not for conception. We treated them like seasonal tools, useful between attempts, paused when trying, so treatment never stole the window we were working so hard to find.
Endometriomas demanded grown-up conversations. If a cyst hid follicles or raised infection risk, we considered expert surgery; if it sat quietly, we guarded every egg and kept the scalpel holstered. Evidence keeps repeating this lesson: routine removal before IVF rarely improves live birth and can trim the oocyte count you’ll wish you had later.
IVF wasn’t a defeat for us; it was an efficiency decision. The first cycle can sting with lower implementation, but cumulative outcomes often catch up when the plan is steady and smart. Knowing that in advance saved us from spiraling after one result and helped us keep going together.
Most of all, we protected ourselves. We set no-fertility Sundays, asked blunt questions in clinics, and kept a short list of things that made her body feel safe. Love didn’t wait for two lines; it showed up in the choices that made those lines more likely.
Final Word on Fertility and Endometriosis
If you are here, you already know how quickly hope can turn into homework. You have read studies late at night, compared numbers you never wanted to learn, and tried to make plans while pain kept moving the goalposts.
I have stood in those same kitchens at 2 a.m., holding a hot water bottle for my wife, asking how much longer we keep trying the same way, and when we change the plan. What finally steadied us was not a single miracle treatment but a way of thinking. Get the clearest map of the disease you can with truly expert imaging. Measure time honestly, not abstractly.
Treat ovarian reserve as information, not identity. Decide in daylight what you will try next and for how long, so the hard moments do not get to rewrite your goals.
We learned that progress often looks smaller than you expect. One better scan. One cycle where timing finally matched biology. One appointment where a clinician speaks to you like partners in the same mission.
Sometimes the right choice is to keep trying naturally with intention. Sometimes it is trying to do IUI with a strict time box. Sometimes it is better to move to IVF sooner to protect tomorrow’s chances. None of these choices says anything about your worth. They are simply different bridges toward the same shore.
Pain management needs honesty. Treatments that calm symptoms can pause ovulation, and that is not failure. It is a season.
Use them when you need to breathe. Press pause when you are ready to try. If an endometrioma is part of the picture, seek a surgeon who treats eggs like treasure and who can explain in plain words why operating now helps more than it harms. If the cyst can be safely observed while you pursue assisted reproduction, guard those follicles like you would guard your future.
Most of all, protect the two of you. Build small rituals that remind you you are a couple first and a case second. Make room for laughter even on clinic days. Ask blunt questions. Keep a written plan you both agree on, with dates you will review, so you are never drifting.
The outcome matters. How you get there matters too. Your child deserves parents who learned, long before birth, how to stay on the same side when life turns complex.
I cannot promise an easy road. I can promise you are not walking it alone. If tonight is one of those nights, take a breath, write down the next two steps, and rest. Tomorrow you will move again, not because you are lucky, but because you are brave enough to keep choosing.
A short summary to carry in your pocket: your odds are shaped by age, reserve, anatomy, and time. Get the best imaging you can, decide your path in advance, and adjust with data, not fear. Natural timing, IUI, or IVF are tools. Use the one that serves your timeline, your values, and your love for each other.
If this helped, leave a comment so others can find it, and grab a free chapter of my “Endo-Tool: Endometriosis for Men.” When you join us, you also join a community that shares more freebies, big discounts on all our books, and real emails that help couples adapt to a new normal without losing each other.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MOREFertility and Endometriosis FAQs
1) Can you still get pregnant with endometriosis?
Yes. Many people conceive naturally, especially with milder disease and good ovarian reserve. Chances depend on age, cycle regularity, tubal health, and whether endometriomas or deep lesions distort anatomy. When time matters, a time-boxed plan (natural cycles → IUI → IVF) helps protect pregnancy rates.
2) Does endometriosis make it harder to get pregnant—and how?
Inflammation, adhesions, and distorted pelvic anatomy can affect ovulation, egg pickup, and tubal transport. Pain can also reduce intercourse timing during the fertile window. Mapping disease with expert ultrasound and tracking cycles closely improves the odds when trying to get pregnant with endometriosis.
3) Should an endometrioma be removed before IVF?
Not automatically. Surgery can help if a cyst blocks follicle access, causes significant pain, or raises infection risk, but it may reduce ovarian reserve. Discuss size, position, prior surgeries, and retrieval access with a specialist before deciding; sometimes careful monitoring plus IVF is the safer route.
4) What’s the best age to get pregnant with endometriosis?
There’s no single “best” age, but age strongly influences egg quantity and quality. If family-building is a priority, test AMH/AFC early and plan timelines accordingly. For some, it’s reasonable to try naturally for a few cycles; for others, moving to IUI or IVF sooner preserves chances.
5) Can lifestyle changes improve the chances of getting pregnant with endometriosis naturally?
Lifestyle isn’t a cure, but it can support fertility: consistent sleep, anti-inflammatory nutrition, gentle movement, and stress buffers can make timed intercourse more feasible and reduce flare-ups. These steps complement—not replace—medical options like monitored cycles, IUI, or IVF when months matter.
Fertility and Endometriosis References
ESHRE Guideline: Endometriosis (2022, full PDF)
- ESHRE Guideline overview page (issued Feb 2, 2022)
- NICE update: improving diagnosis of endometriosis (news, Nov 11, 2024)
- NICE NG73: Endometriosis—diagnosis and management (resource impact, Nov 11, 2024)
- ASRM Practice Committee: Endometriosis and infertility (Committee Opinion)
- Human Reproduction: Cumulative live birth under consecutive IVF/ICSI in endometriosis/adenomyosis (2025)
- PMC review: Endometriosis lowers cumulative live birth rates in IVF (2020)
- J Minim Invasive Gynecol: Endometrioma surgery vs expectant management before IVF—systematic review & meta-analysis (2019)
- NHS England: New endometriosis pill could benefit >1,000 women/year (May 1, 2025)
- NICE: First daily pill for endometriosis approved for NHS use (Mar 13, 2025)