Endometriosis Advocacy and Awareness
What does endometriosis advocacy actually achieve for real families?
Endometriosis advocacy means mobilising patients, partners, clinicians, and lawmakers to end diagnostic delays, secure sustained research funding, expand equitable treatment access, and embed accurate education, turning pain into system change so care is earlier, safer, and truly rooted in evidence.
Here’s the part many people miss – average diagnostic delay still spans years, which is why organized voices push for clearer pathways and earlier recognition. Global efforts like the Worldwide EndoMarch focus attention every March, and 2025 events are already set.
In England, a newly approved daily pill on the NHS shows how policy and advocacy can translate into real treatment options. Toolkits now exist to help anyone contact lawmakers with specific, effective asks.
I’ve watched my wife fight for answers while we learned to rebuild life around pain and flare-ups. Advocacy isn’t abstract for us; it’s the difference between being dismissed and finally being seen, treated, and supported.
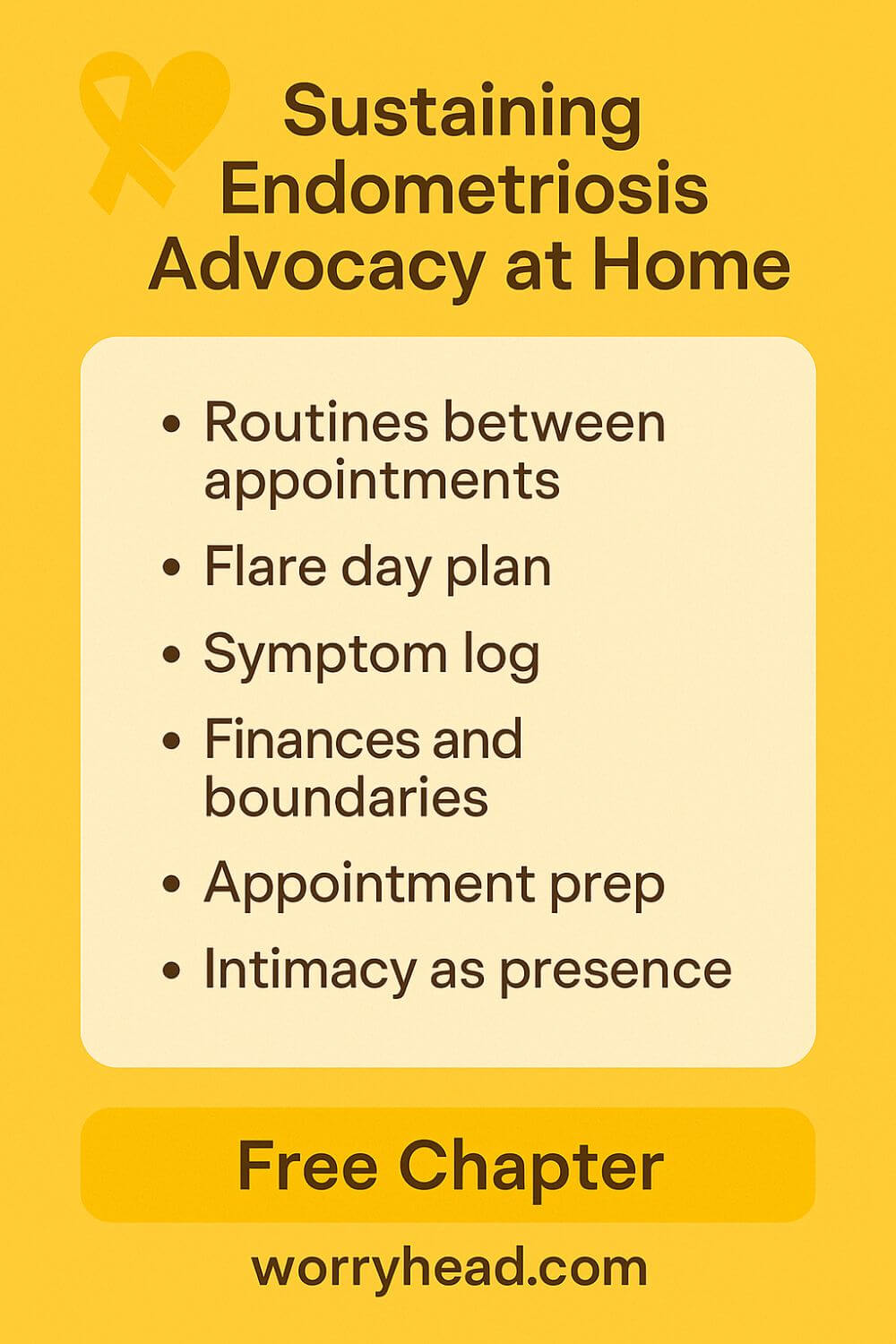
If this is your world too, you’re not alone. You can also grab a free chapter of my “Endo-Tool: Endometriosis for Men”; by joining, you’ll enter our community for more freebies, big discounts on all our books, and emails packed with practical, loving support to help you and your partner adjust to the new normal.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis, and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men

What Effective Endometriosis Advocacy Looks Like?
Change starts where stories meet data, and the people who hold both refuse to be quiet. Advocacy that moves the needle blends lived experience with measurable goals: shortening diagnosis delays, improving primary-care pathways, expanding access to evidence-based treatment, and securing ring-fenced research funding.
It begins with recognition that diagnostic delay is not a minor inconvenience but a multi-year harm that compounds pain, costs, and complications for families. Recent UK data shows the average wait is now eight years and ten months, worse than in 2020, so any strategy that doesn’t attack delay first is cosmetic.
Next comes structure. Toolkits now exist to guide letters to MPs, local commissioners, and employers, translating raw frustration into policy asks: better GP training, fast-track referral criteria, and funding lines for specialist services. This turns one voice into many, and many into legislation and budgets.
Momentum matters, which is why coordinated campaigns tie personal stories to national moments. Global events like the EndoMarch concentrate public attention and make it simpler to mobilise media, organise clinics to audit pathways, and invite policymakers to hear patients directly. 2025 dates are already set, giving advocates a clear rally point.
Policy wins must translate into care at the bedside. In England, the first long-term daily pill for endometriosis symptoms has been approved for NHS use; that’s a concrete example of advocacy, evidence review, and access policy lining up so patients aren’t left waiting for injections or referrals.
Education is the thread through it all. Updated national guidance now emphasises earlier recognition and clearer diagnostic routes, signalling to primary and secondary care that the target has shifted from “rule out” to “find and treat.” Local services can use the guidance to justify resources, and citizens can use it to hold services accountable.
Finally, sustainability: coalitions keep pressure steady when headlines fade. Organisations focused on research, surgical training, and Capitol Hill/Parliament advocacy show how consistent, well-briefed voices secure funding lines and curriculum changes year after year.
When I speak to clinicians or councillors, I carry my wife’s story, years of symptoms, the quiet dread of another dismissal, the relief when someone finally listened.
That’s why I care about endometriosis advocacy being practical, measurable, and relentless: because the cost of inaction is paid in her pain and our time together. The tips below are what I wish we’d had on day one:
- Map your local care pathway and identify the delay points
- Use a ready-made policy toolkit to write your MP/representative
- Tie your story to a public awareness date to amplify reach
- Ask your GP practice to adopt guideline-aligned referral prompts
- Request your hospital trust audit endometriosis wait times quarterly
- Push for equitable access to newly approved medical options
- Join a research/education coalition to keep funding on the agenda
- Train partners/families to be effective, concise advocates
- Track wins (and gaps) so momentum doesn’t stall
Map Your Local Care Pathway
Before we could change anything, I had to understand the maze my wife was walking through: GP, routine scans, referrals, surgical lists, pain clinics, mental health support. I sketched it on paper, then marked the places she got stuck: gatekeeping at primary care, inconclusive imaging, and the long, quiet months waiting for letters.
Next, I compared what should have happened to what actually did. Guidelines promised timelines; reality delivered silence. That contrast gave me language for emails and meetings: specific bottlenecks with dates attached, not just “it’s slow.”
When you map yours, note names, departments, phone numbers, and expected vs. actual waiting times. Patterns appear. Once you see them, you can challenge them, politely, firmly, with evidence, and invite your practice manager or Patient Advice and Liaison Service into a practical conversation about fixes.
Use a Policy Advocacy Toolkit
I used to write from the heart and hope it landed. It rarely did. A policy toolkit taught me to pair a story with an “ask” that fits how systems work: cite guidance, state the gap, propose a fix, request a reply date. Suddenly, doors opened, not because I was louder, but because I was clearer.
Toolkits help translate pain into governance language. They show how to structure letters to MPs or commissioners, add the right identifiers, and point to measurable outcomes—like adoption of referral prompts or an audit commitment.
Print one page that summarises your three asks and why they matter. Practice saying it in two minutes. When your representative hears a concise brief that ties personal harm to a solvable policy, you’re not just venting, you’re governing.
Tie Your Story to Awareness Dates
We used Endometriosis Awareness Month as scaffolding. Media want timely angles; clinics expect questions; lawmakers have diaries to fill. Anchoring our outreach to March meant our emails were “of the moment,” and local outlets were more willing to run a piece that paired our story with community resources.
Pick a date, then plan backwards. Two weeks out, pitch a short op-ed or radio segment. One week out, invite your hospital trust to share pathway data. On the day, host a small teach-in at the library or online, and collect contacts for follow-up.
The date isn’t the point; the momentum is. A fixed moment helps you gather allies, focus your asks, and measure outcomes:
- Did referrals change?
- Did training happen?
- Did anyone commit to report back?
Ask GP for Referral Prompts
Our turning point was small: a GP template that nudged for cyclical pain, bowel or urinary symptoms, family history, and impact on life and work. When a clinician clicks a box and the system suggests “consider endometriosis” with a clear referral route, fewer women are told to “watch and wait.”
You don’t need to write the template yourself. Ask your practice manager what they’re using now and whether a guideline-aligned prompt could be adopted. Offer examples, keep it friendly, and ask for a trial period with feedback.
Prompts don’t replace judgment; they protect it from busy days. They make it easier for the next patient to be heard the first time, not the fifth. That’s advocacy that quietly saves months of pain.
Audit Hospital Wait Times Quarterly
Hospitals track a lot, but not always what hurts most. We requested a simple quarterly snapshot: time from referral to specialist appointment, imaging to decision, decision to surgery. Once those numbers were visible, delays stopped being personal failures and became system issues to fix.
An audit doesn’t shame staff; it equips them. When a department sees its own trend line creeping up, it’s easier to argue for theatre time or additional clinic slots. It also gives patient groups a baseline to celebrate improvements or press for change.
Ask for anonymised data and a short meeting to review it. Offer to help craft a public-facing summary so families know what to expect and how to escalate if timelines slip.
Push for Equitable Treatment Access
My wife’s options shouldn’t depend on postcode, insurance quirks, or whether a clinician has time to fill a form. Advocacy here means understanding which therapies are approved, where the bottlenecks are, prescribing caps, eligibility criteria, stock, and asking services to publish clear, fair access pathways.
Start by documenting when access was denied or delayed and why. Then propose practical remedies: shared-care agreements between hospital and GP, named contacts for prior authorisations, or group education visits to speed informed consent.
Equity is not a slogan; it’s a calendar, a form, a signature. When those align, people get care on time, without begging.
Join Research and Education Coalitions
I used to feel alone, then I met people who speak evidence as a native language, researchers, educators, and seasoned patient leaders. Coalitions turn our lived experience into agenda items: training modules for GPs, teaching sessions for schools, research priorities shaped by what patients actually endure.
Joining isn’t about titles; it’s about rhythm. Show up, take notes, volunteer for one small task, bring a partner’s perspective to a room that needs it.
Coalitions outlast news cycles. They’re how we move from “someone should” to “this is funded, scheduled, and measured,” and they make sure the next family meets a trained listener, not a shrug.
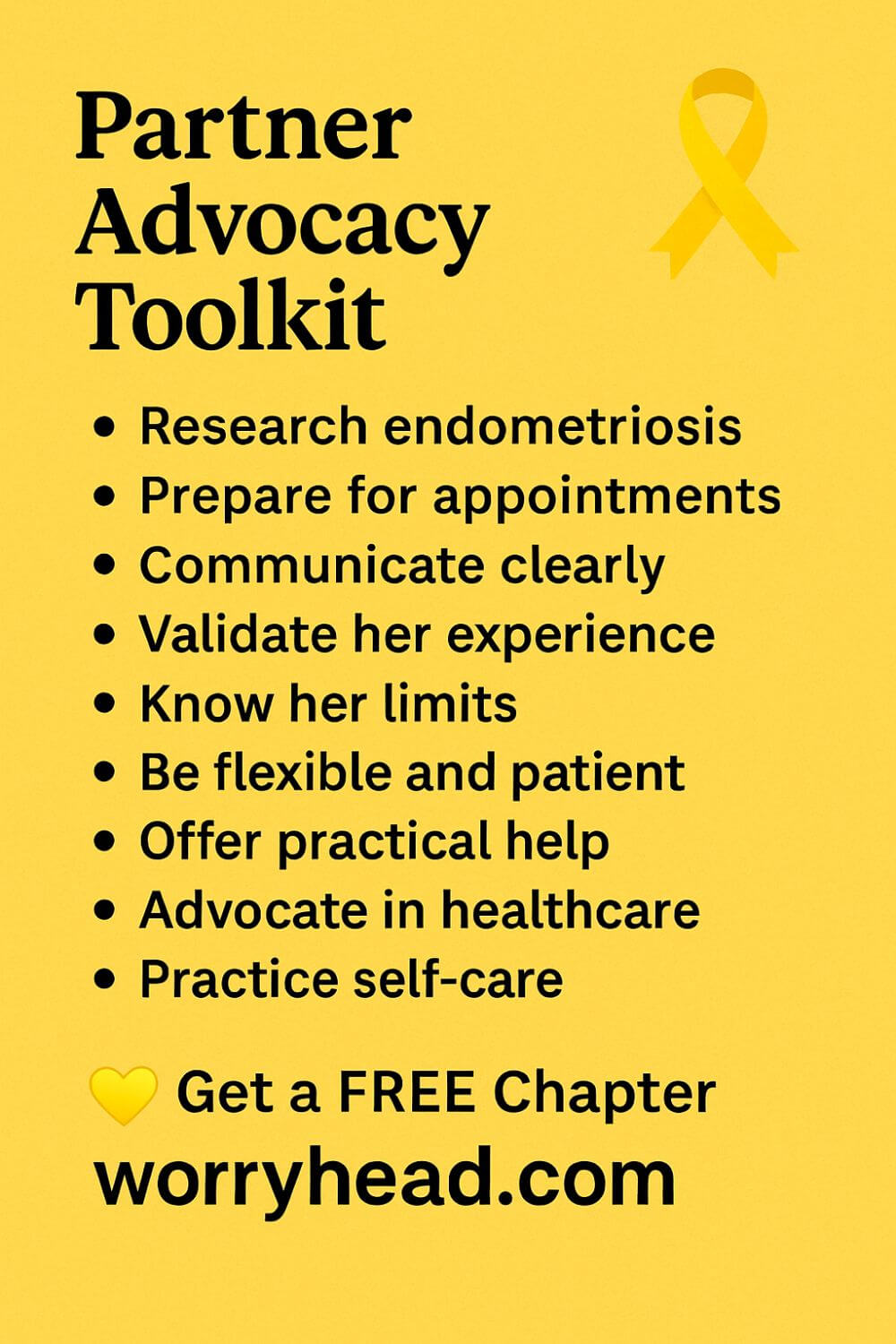
Train Partners as Concise Advocates
I learned to keep a symptom log, bring two copies, and open with a 30-second summary: onset, pattern, impact, goal for today. Then I stopped talking and let my wife lead. That balance, prepared support without overshadowing, changed appointments from chaos to progress.
Teach partners to ask clarifying questions, request safety-net plans, and confirm next steps in writing. Role-play at home. Pack snacks, heat pads, and a charger. It sounds small until a six-hour clinic runs late and you still get the answers you came for.
Concise advocacy respects clinicians’ time and protects your energy. It turns a hard day into a productive one.
Track Wins and Persistent Gaps
We kept a one-page timeline: referrals made, tests done, outcomes, promises. Not to dwell on steering. When something slipped, we had dates and names to nudge. When something worked, we thanked people and asked how to replicate it.
Tracking is accountability and encouragement in the same breath. It shows progress to a tired heart and gives structure to follow-ups with managers or representatives.
Most importantly, it prevents learned helplessness. When you can point to a pattern, you can plan a remedy. That’s how small wins stack into a new normal where being believed isn’t a miracle, it’s the standard.
How Endometriosis Advocacy Becomes Bedside Change?
Hospitals don’t move because we shout; they move because we show them the next right step and then the next. I learned that sitting in plastic chairs under fluorescent lights, watching the clock and my wife’s face, wondering which would crack first.
So I began translating feelings into fixes. I arrived with a 30-second summary, a symptom timeline, and a single outcome for today. Clinicians leaned in because I made it easy to help.
We asked for clarity, not miracles.
- What’s the plan if this medication fails?
- When should we call if pain spikes?
Simple questions turned fog into a path.
At the trust level, we requested small, measurable improvements. A quarterly snapshot of referral-to-appointment times. A named email for complex cases. Ten minutes at grand rounds to share what delays do to a family.
Then we focused on repeatable wins. A template in primary care that nudged for cyclical pain and fast-tracked referrals. A one-page leaflet for newly suspected cases, explaining scans, options, and pain safety.
Change gathered allies. A registrar who cared about audit quality. A practice nurse who updated the triage script. A manager who scheduled an extra clinic and protected it from cancellations.
I used my voice once, carefully: endometriosis advocacy. Not as a slogan, but as a promise to show up with evidence, stay with kindness, and leave with the next action written down.
On the hardest days, when pain stole her words, I spoke the bare minimum and handed over the notes we’d prepared at the kitchen table. The care team saw a couple with a plan, not a problem with no end.
When surgery finally came, it wasn’t luck. It was the quiet accumulation of small asks that shortened months into weeks. It was the staff who felt respected enough to fight for theatre time.
If you’re reading this at 3 a.m., counting breaths and minutes, I know that thud in your chest. What you build tomorrow will be small and specific. It will also be the seed of a different year.
Because bedside change is not a speech, it is a list, a name, a date, and two people who refuse to let love be measured only in waiting rooms.
Conclusion on Endometriosis Advocacy
When I think about what actually moved the needle for my wife, and for the families who write to me, it wasn’t a single headline or a viral post. It was the slow, stubborn craft of turning stories into structures: clear referral prompts in primary care, published wait-time audits, and access to the right therapies at the right time. Policy, practice, and people had to meet in the same room. That is the heart of change.
In the last year, we’ve seen what an aligned effort can win. National guidance has shifted toward earlier recognition based on symptom history, even when imaging is inconclusive, so fewer patients are left in limbo. At the same time, England approved the first long-term daily pill options for symptoms, giving clinicians and patients a practical alternative to repeated injections and long clinic waits. Policy isn’t abstract when it shortens a queue or eases a night.
But guidance on paper doesn’t erase years lost to delay. Average diagnosis times still stretch across much of a decade in the UK, with families bearing the cost in pain, employment, and fertility fears.
Advocacy earns its name when it pushes systems to measure what matters, referral-to-appointment times, imaging-to-decision intervals, decision-to-surgery windows, and to publish, fix, and repeat. That’s how we stop normalising avoidable harm.
I’ve learned that the most credible voice in the room is the one that brings receipts: dates, names, guidance paragraphs, and one clear ask. Toolkits now exist to help any partner, patient, or clinician write to representatives, boards, or commissioners with language that lands, is specific, lawful, and tied to measurable outcomes. Use them. They turn grief into governance.
And keep your courage anchored to the community. Awareness months and coordinated campaigns are not just yellow ribbons on a calendar; they’re scaffolding for audits, media conversations, and meetings with decision-makers who need to hear what quiet rooms already know.
When we show up together, patients, partners, nurses, surgeons, and researchers, the story changes faster than it used to.
If you carry this at 3 a.m., I see you. I’m just a husband who learned to translate love into minutes and checklists, into letters that ask for one practical step and then the next.
Systems don’t respond to shouting; they respond to steady light. Take the guideline in one hand and your lived experience in the other, and keep walking them toward each other until they meet at the bedside. That’s how tomorrow gets kinder, for you, for her, for the next family who hasn’t found the words yet.
Progress is real: earlier-recognition guidance, new NHS treatment options, stronger toolkits, but long diagnosis delays still hurt families. The work that changes lives is local and measurable: map delays, ask for audits, press for equitable access, and use coordinated awareness to keep pressure and hope alive.
I’d love to hear your story in the comments, and if you need practical support, grab a free chapter of my “Endo-Tool: Endometriosis for Men.” When you join, you’ll also enter our community for more freebies, big discounts on our books, and steady, real-world guidance to help your relationship adjust to the new normal.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MOREEndometriosis Advocacy and Awareness FAQs
1) What’s the single most effective first step for endometriosis advocacy?
Map your local care pathway and identify the exact delay points (GP triage, imaging, referral, surgery). Write them down with dates, then send a concise letter to your practice manager or hospital PALS with one clear ask (e.g., adopt guideline-aligned referral prompts or share wait-time data). Specifics move systems faster than general complaints.
2) How can a partner advocate without speaking over the patient?
Prepare together. Bring a one-page summary (onset, pattern, impact, today’s goal), then let your partner lead. As a supporter, ask clarifying questions, request a safety-net plan, and confirm next steps in writing. After the appointment, send a short thank-you email that also documents agreed actions and timelines.
3) Does awareness month activity actually change care—or just make noise?
It changes care when you attach measurable asks to the moment. Use March to request a referral-to-appointment audit from your trust, ask your GP network to trial a symptom prompt, or invite local media to cover concrete pathway improvements. Pair your story with one policy change and a follow-up date.
4) What can I do if new treatments are approved but access is patchy where I live?
Document the denial (who, when, why), cite the relevant national guidance or formulary status, and request a named contact to escalate. Ask for a shared-care agreement if prescribing is stuck between hospital and GP. If criteria are unclear, request them in writing and ask when they’ll be published for patients.
5) How do I support advocacy when I’m already exhausted by pain and admin?
Shrink the scope. Choose one micro-action per month: update your symptom log, send one policy letter using a template, or attend one coalition call. At home, protect recovery time on the calendar and delegate tasks to a friend or partner. Sustainable advocacy is rhythmic, not heroic; small, steady steps add up.
Endometriosis Advocacy and Awareness References
- Endometriosis UK diagnosis report: “Dismissed, ignored and belittled” (2024)
- NICE guideline NG73: Endometriosis—diagnosis and management (2024 update)
- NICE news: First daily pill for endometriosis approved for NHS use (13 March 2025)
- Endometriosis UK statement on relugolix–estradiol–norethisterone (Ryeqo) approval (2025)
- Worldwide EndoMarch: EndoMarch Day 2025 & AGCES
- Society for Women’s Health Research: Endometriosis Advocacy Toolkit (2024)
- Endometriosis Foundation of America (EndoFound): advocacy, education, research
- NICHD Endometriosis Resources (U.S. NIH)
- Time to Diagnose Endometriosis: Current Status and Potential Solutions (2024 review, open access)
- ClinicalTrialsArena: NHS in England approves Ryeqo daily pill for endometriosis (Mar 2025)
- Endometriosis Association: Awareness Month—how you can make an impact (2025)