Theories & Causes for Endometriosis
What are the real theories & causes for endometriosis?
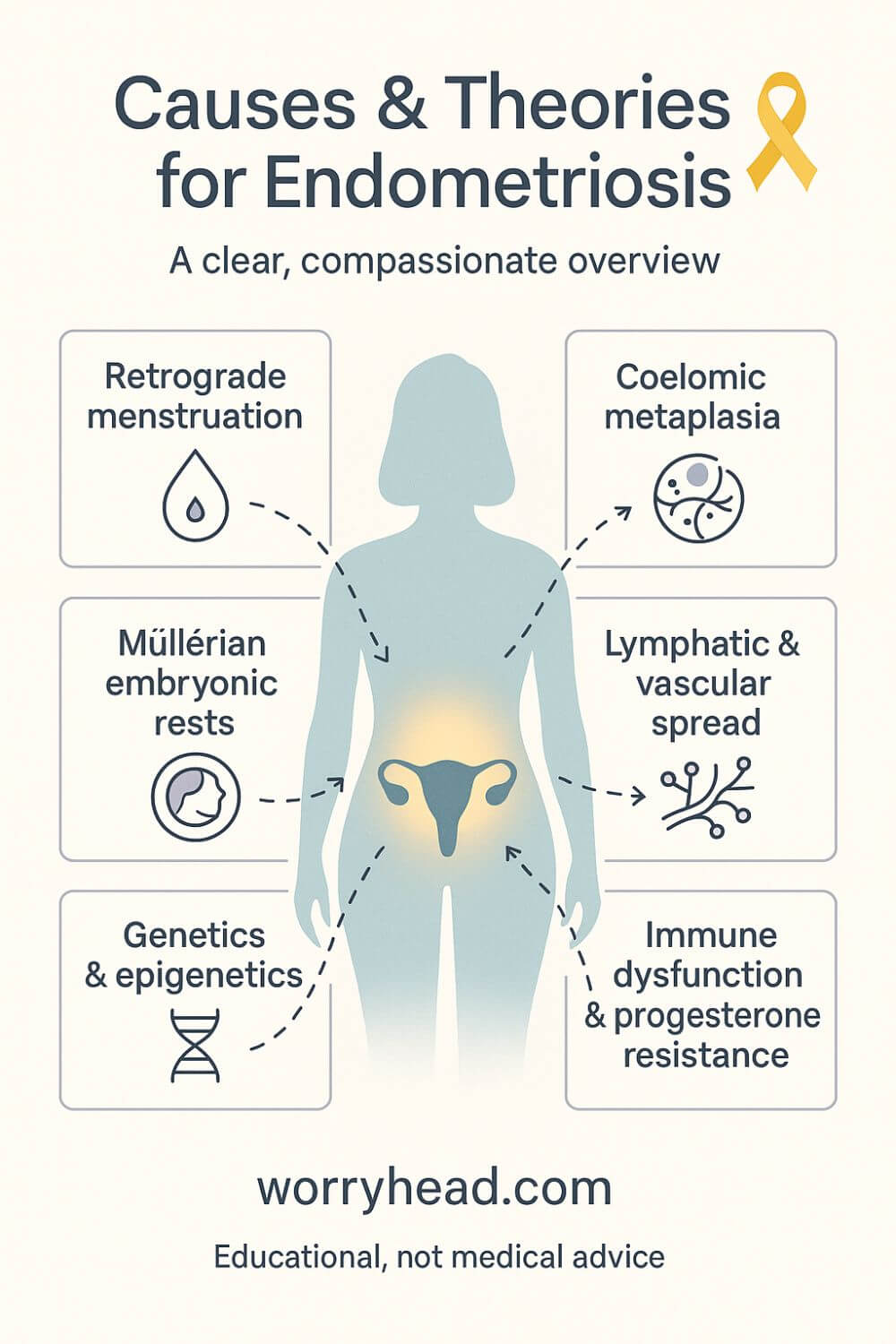
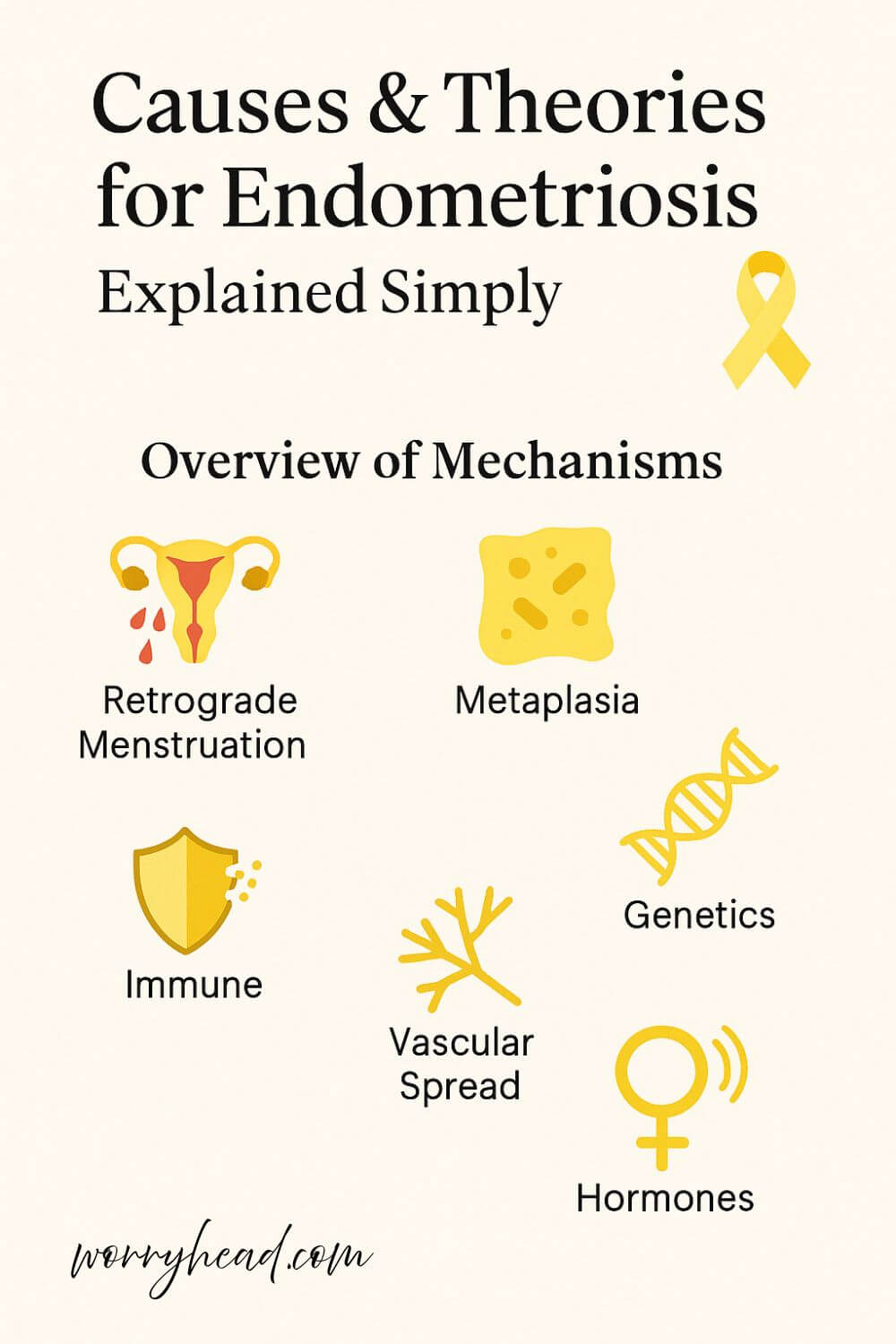
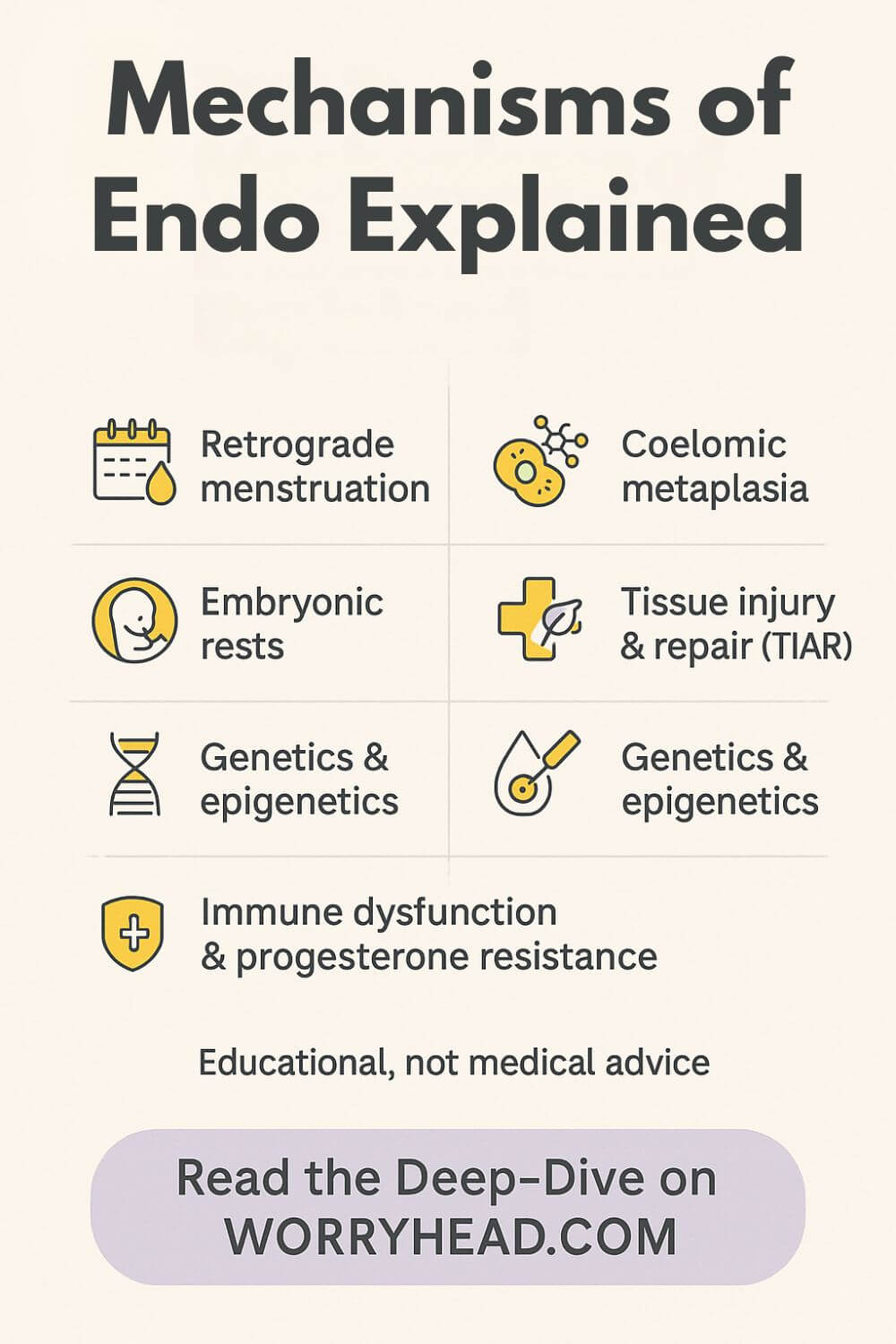
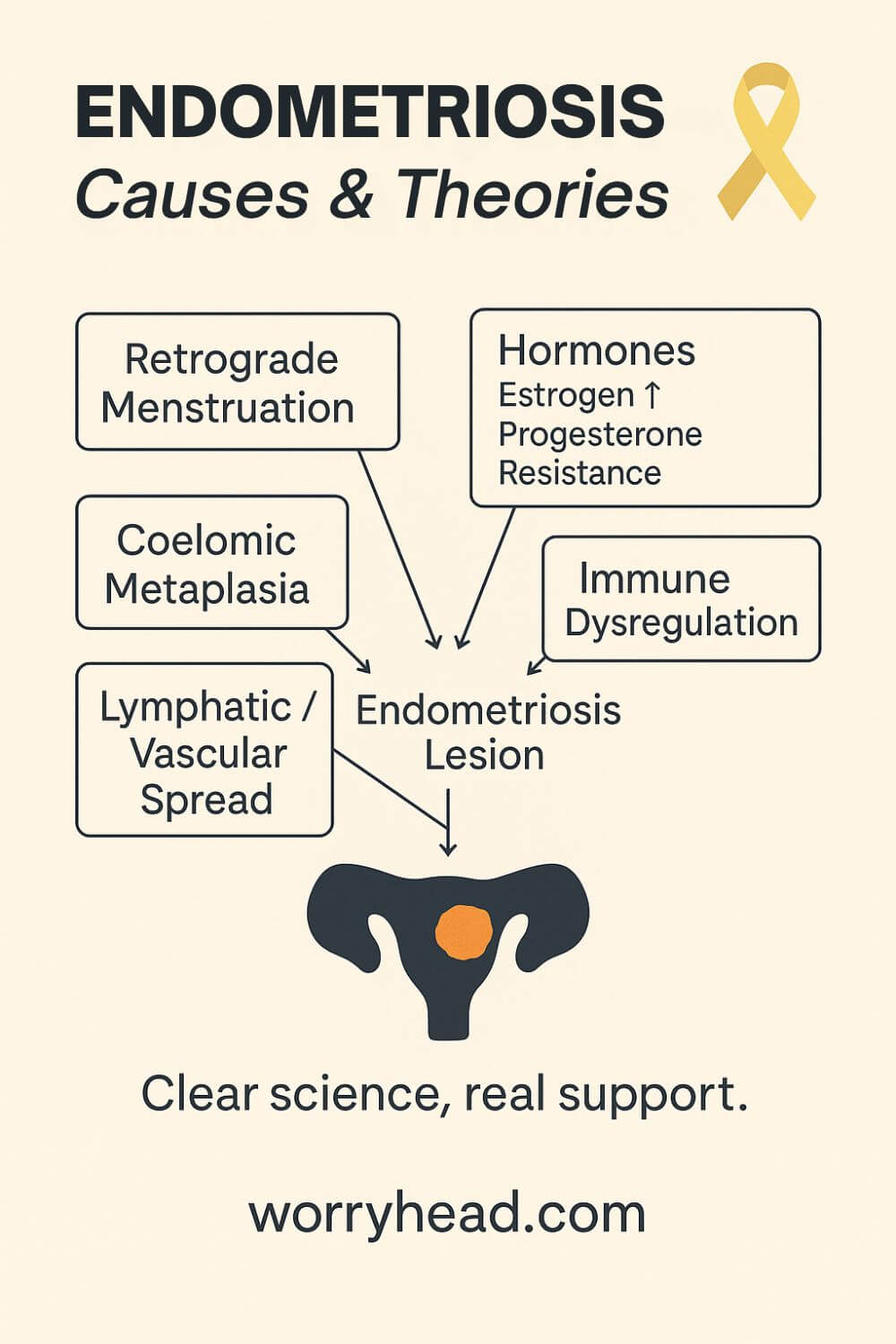
Endometriosis likely arises from multiple interacting mechanisms: retrograde menstruation with implantation, coelomic metaplasia, lymphatic or vascular spread, and genetic and immune factors. No single cause explains all cases; it’s a multifactorial disease influenced by hormones and environment.
Some lesions are found in places that make you pause, on the diaphragm, in surgical scars, even rarely in the lungs, hinting that cells can travel or transform in surprising ways. Researchers are exploring somatic gene changes and immune dysregulation that may “prime” tissue to behave like endometrium outside the uterus.
We’re also learning that stage doesn’t predict pain, and that biology can be wildly individual. All of these points to one truth: there isn’t a single map – there are several, and they overlap.
I’ve watched my wife fight through this maze, the pain, the confusion, the appointments where answers felt just out of reach, and it changed the way I read every paper and talk to every clinician. If you’re here, you deserve more than definitions. You deserve clarity, compassion, and a path that actually helps.
If endometriosis is part of your life, grab a free chapter of my “Endo-Tool: Endometriosis for Men.” By joining our community, you’ll also get more helpful freebies, big discounts on all our books, and honest emails designed to help you and your partner adjust to the “new normal” with practical support and real hope.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis, and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men

Theories & Causes for Endometriosis
Let me unpack the causes & theories for endometriosis in plain language and show you what actually has evidence behind it.
The truth is, there isn’t one single cause. Different mechanisms can start the fire, and others keep it burning, so understanding them helps you ask better questions, push for the right care, and make sense of confusing advice.
Sampson’s idea, often called the retrograde menstruation theory, says menstrual tissue can flow backward through the tubes into the pelvis, stick, and grow. That backflow likely happens in most menstruating people, yet only a minority develop disease, which hints that something about immune surveillance and local biology decides what takes hold.
The coelomic metaplasia theory (“metaplastic theory of endometriosis”) proposes that cells lining the abdomen can transform into endometrial-like cells under hormonal or inflammatory signals. It helps explain disease in teens, in those without a uterus (MRKH), and in very rare cases in men on estrogen therapy.
An embryonic (Müllerian) rests explanation says tiny embryologic leftovers along the reproductive tract can later “switch on” and behave like endometrium. That’s why some lesions pop up in unusual places along embryologic pathways.
The vascular theory of endometriosis (lymphatic/hematogenous spread) explains distant sites, such as the diaphragm, pleura, and even surgical scars, by cells traveling via lymph or blood before implanting. It fills the gaps that the retrograde idea can’t cover on its own.
You’ll also hear about tissue injury and repair (TIAR): repeated micro-trauma and uterine hyper-peristalsis trigger a repair loop that’s estrogen-driven, encouraging more lesions and pain. Think of it as biology stuck on “repair,” amplifying itself.
Stem cell models add that endometrial or bone-marrow-derived stem cells can seed new lesions moving with backflow, lymph/blood, or direct invasion, then settle into local “niches” and persist.
Layered on top are genetics and epigenetics. Family risk is real, heritability is substantial, and lesion biology often shows estrogen dominance with progesterone resistance molecular shifts that help tissue survive where it doesn’t belong. These changes help explain why stage doesn’t predict pain, and why treatments work differently person-to-person.
Finally, immune dysfunction matters. Recent Mendelian-randomization work links specific immune cell profiles with altered endometriosis risk, reinforcing the idea that impaired clearance and a pro-inflammatory environment allow ectopic cells to implant, grow, and sustain nerves and blood vessels.
Major clinical sources summarise these threads together, adding practical notes such as surgical scar implantation and cell transport through vessels, reminding us why mechanisms also tie to endometriosis and fertility through scarring, inflammation, and distorted pelvic anatomy.
When my wife and I sat in yet another waiting room, I kept wishing someone would explain all of this like a map with honest “we don’t knows,” but also the roads worth taking next. If you’re reading this for someone you love, I see you. Here’s the map we never got, starting with the most actionable places to focus:
- Retrograde menstruation: what actually happens
- Coelomic metaplasia: peritoneum transforming
- Embryonic Müllerian rests: early origins
- Lymphatic & vascular spread pathways
- Tissue injury and repair theory
- Stem cell seeding and niches
- Genetics and epigenetics, family risk
- Immune dysfunction: clearance and inflammation
- Hormonal milieu: estrogen and resistance
Retrograde Menstruation
Retrograde menstruation is simple to picture, yet complicated in practice. During a period, some endometrial cells travel through the fallopian tubes into the pelvis instead of leaving the body. Most people have some backflow, but only a subset keeps living cells that attach.
What decides who develops a disease is the local environment. If immune cells fail to clear the debris efficiently, those fragments can implant on the peritoneum, ovaries, or ligaments. Once attached, estrogen exposure and inflammatory signals help them survive, sprout tiny blood vessels, and connect with nerves.
This is why pain can feel out of proportion and why lesions can persist for years. The mechanism also hints at prevention discussions, not as blame, but as biology, where reducing inflammation and treating heavy bleeding early may change the field these cells land in.
Coelomic Metaplasia
The metaplastic theory of endometriosis asks us to look at the peritoneum not as a passive sheet, but as adaptable tissue. Under hormonal or inflammatory stress, those lining cells may transform into endometrial-like cells, a process called coelomic metaplasia.
This model helps explain disease in adolescents, in people with obstructive anomalies, and in rare cases outside classic menstrual routes. It also accounts for lesions near the diaphragm or on surfaces with no direct contact with menstrual flow.
If tissue can change identity under signals, the focus shifts to what drives that signal. Chronic inflammation, local estrogen production, and growth factors become targets. For my family, this lens removed the shame that something “leaked”, and replaced it with a clearer question, which signals can we calm.
Embryonic Müllerian Rests
Embryonic rests are tiny remnants from early development, pieces of Müllerian tissue that never fully regressed. They can lie dormant along embryologic pathways for years. Later in life, hormonal exposure or inflammation may activate them, leading to endometrial-like lesions where no transport route makes sense.
This concept clarifies why some diseases appear in unusual spots and why symptoms can start very young. It also fits with observations that pain severity does not neatly follow the stage.
When I learned this, I stopped chasing a single event to blame. A seed can be there from the start, then awaken under the right conditions. That shift matters emotionally too, because it replaces self-blame with a kinder, developmentally grounded explanation.
Lymphatic and Vascular Spread
The vascular theory of endometriosis proposes that cells can ride the body’s own highways. Through lymphatic channels or blood vessels, fragments or stem-like cells reach distant sites, then implant. This pathway explains lesions in the chest, the diaphragm, and even in scars after surgery.
Transport is only part one. For cells to take root, they need a welcoming niche, which often means inflammation, estrogen exposure, and immune evasion.
Clinicians sometimes find microscopic disease in lymph nodes, which supports the possibility of cellular traffic through these routes, even if not every node signals clinical trouble. Mapping symptoms to the calendar can reveal patterns that suggest thoracic involvement, guiding imaging and referrals.
With appropriate suspicion and a coordinated team, seemingly disconnected dots form a clearer picture, and patients get faster answers.
Tissue Injury and Repair
Tissue injury and repair, sometimes called the TIAR model, views the uterus as an active muscle exposed to repeated micro-trauma. Hyperperistalsis and heavy bleeding trigger repair programs that are estrogen-driven. Over time, this loop can increase backflow, promote lesion survival, and wire pain circuits more sensitively.
This is not a moral failing; it is physiology spiraling. Interrupting the loop can involve reducing bleeding, calming inflammation, and addressing pelvic floor dysfunction that keeps muscles in a guarded state.
Pelvic congestion, adhesions, and sensitized nerves can all be downstream of this cycle, which is why comprehensive care looks beyond hormones alone. Gentle movement, pelvic physiotherapy, and paced activity become medical, not optional, because they reduce inputs that keep the injury repair loop humming.
Stem Cell Seeding
Stem cell models suggest that progenitor cells from the endometrium or bone marrow can travel and differentiate into endometrial-like tissue outside the uterus. Unlike mature fragments, these cells are flexible, able to settle into new niches and persist.
This theory ties together findings from retrograde flow, vascular spread, and metaplasia, because stem-like cells can move through each pathway. It also explains why lesions can recur, even after seemingly complete removal.
Research into lesion heterogeneity shows that not all implants look or behave the same, which fits a world where different progenitors seed different neighborhoods. Therapeutic research is exploring how to change the soil rather than just pluck the plants, shifting from one-time fixes to sustained ecosystem care.
Genetics and Epigenetics
Family history increases risk, which points to heritable factors, while epigenetic changes in lesions show how the environment writes on genes that regulate hormone response and inflammation. The endometrium in those with disease often behaves differently, with progesterone resistance and heightened estrogen signaling.
These molecular shifts matter clinically. They may explain why some people do not respond to certain treatments, and why pain can persist despite small lesion loads.
In our home, understanding biology softened hard days. When a therapy failed, it felt less like a personal defeat and more like data about pathways that needed a different approach. Families often share not only genes but environments, so teasing apart risk requires care, yet the pattern remains after adjustments.
Epigenetic marks can be reversible, which offers hope that targeted therapies or lifestyle shifts might tilt biology toward less inflammation and more normal hormone response over time.
Immune Dysfunction
Immune dysfunction does not mean a weak immune system; it means a misdirected one. In endometriosis, clearance of refluxed cells may be impaired, while inflammatory cytokines, macrophages, and mast cells create a fertile ground for implantation.
Nerve fibers grow into lesions, which amplifies pain and maintains the cycle. For patients, this framework validates symptoms beyond the pelvis, including fatigue and flares that feel like inflammation everywhere.
Adhesions and deep infiltrating lesions recruit fibroblasts that lay down collagen, which tightens tissues and restricts mobility. That stiffness feeds pain and can affect fertility by distorting pelvic anatomy. Calming inflammation and breaking that cycle, surgically when needed and medically day to day, is therefore a rational, layered plan.
Hormonal Milieu and Resistance
Estrogen fuels growth, angiogenesis, and innervation of ectopic tissue, while progesterone resistance limits the usual braking effect. Lesions themselves can produce estrogen locally through aromatase, creating a self-sustaining loop.
Understanding this helps explain why therapies that lower estrogen or boost progesterone signaling can reduce pain, and why responses vary. The target is not just hormone levels in blood, but the tissue’s local conversation.
Side effects and goals differ for each option, so shared decision making matters. For my wife, seasons of hormonal treatment alternated with surgical care and nonpharmacologic supports, an evolving plan that respected her body and our life outside the clinic.
From Theories & Causes for Endometriosis to Daily Life
By now, the map is clearer: no single spark explains the fire, but overlapping mechanisms do. Retrograde menstruation is commonly seen in most menstruating people, yet only a small fraction develop disease, which tells us implantation needs more than backflow.
Coelomic metaplasia and embryonic rests explain lesions that appear far from menstrual routes and even early in life. In these models, peritoneal or embryonic cells can transform under hormonal and inflammatory cues, turning into endometrial-like tissue.
Lymphatic and vascular spread accounts for implants on the diaphragm, chest, and in scars, the body’s own highways moving cells to receptive niches. Again, transport isn’t destiny; survival requires a permissive immune and hormonal climate.
At the molecular level, estrogen-driven growth alongside progesterone resistance shapes how lesions persist and why some therapies falter. These tissue-level differences also explain why two people with the same stage can live completely different stories.
Immune dysregulation, reduced clearance, activated macrophages, and altered NK function create the inflammatory soil where implants vascularize and innervate. Put simply, biology keeps whispering “stay” to tissue that should have been cleared.
Current clinical guidance reflects this multifactorial picture and pushes care toward symptom-focused, individualized plans while research closes the gaps. For fertility, pain, and quality of life, that nuance matters more than any single theory.
I learned this standing beside my wife through scans and surgery notes, begging the science to make sense of the nights she couldn’t sleep. Understanding the causes & theories for endometriosis didn’t cure her, but it finally gave us language and with language, a way to ask for the right help.
Understanding the mechanisms gave us a way to choose care without constant second-guessing. It turned scattered symptoms into patterns we could track and act on.
For my wife, knowing that lesions can survive through local estrogen and inflammation reframed flares as chemistry we could influence. For me, it replaced helplessness with a checklist, reduced bleeding, calmed inflammation, protected sleep, and paced activity.
Together we walked into consults, asking which mechanism seemed most likely in her case, rather than arguing about pain being real. That question changed the room; it led to targeted imaging, thoughtful timing for surgery, and realistic expectations. It also saved us from chasing every supplement and viral claim that promised a cure.
At home, we built routines that respected biology, warm compresses near the desk, flexible hours, and meals that kept inflammation quiet. Grief still visited, especially when plans collapsed, yet understanding why pain spikes happen made it feel less like a personal failure.
Naming the puzzle as causes & theories for endometriosis gave us language to advocate and breathe. It did not erase the hard days; it gave us a way to move through them as a team that knows the why and fights for the how.
Conclusion on the Theories & Causes for Endometriosis
When I first tried to make sense of my wife’s pain, I kept hunting for one culprit. What finally helped was accepting that endometriosis is a networked disease. Different mechanisms can start it, other mechanisms help it survive, and your story is written by the mix you carry and the care you receive.
Retrograde flow may seed cells, but immune clearance and inflammation decide whether they stay. Coelomic metaplasia and embryonic rests explain the early onset and odd locations. Lymphatic and blood routes account for distant implants. Hormones shape the terrain, with local estrogen and progesterone resistance turning a spark into a slow fire.
None of this is abstract. It is the reason a period can feel like an injury, why pain does not match “stage,” why surgery helps some but not all, and why medical therapy buys time for some and not others. It is also why a tailored plan beats a template. Diagnosis is a beginning, not a finish line.
If I could hand you our hard-won lessons, they would sound like this. Track symptoms alongside your cycle and life stresses to see patterns worth testing. When imaging or surgery is planned, ask what question it will answer and how the result will change your next move. Combine pelvic floor care, sleep protection, and inflammation-aware nutrition with the medical options you choose.
If fertility is part of your dream, speak it out loud early. There are routes through this landscape, from timing and referrals to dedicated teams, to support that protects your mental health while you decide. If work is part of your healing, reshape it.
A flexible schedule, a warmer chair, fewer commutes, a kinder boss, these are medical too, because they lower the daily load your body carries.
When people argue about causes & theories for endometriosis, I remember the nights we counted breaths between cramps and the mornings we reset plans again. Theory matters because it points to action. Ask about excision skill, not just access to an operating room. Ask whether thoracic symptoms need attention. Ask how to prevent long waits between follow-up and next steps.
Build a team that can think across silos. A gynecologist who knows deep disease. A pelvic floor physiotherapist who sees how muscles guard. A pain or rehab specialist who can help you pace and move again. A therapist who can hold the grief that rises and falls. Trusted people who speak to each other will spare you from repeating your story alone.
Most of all, refuse shame. You did not cause this. You deserve care that listens, partners, and adapts. Science is moving, and while it has gaps, it already gives us tools to reduce pain, protect function, and reclaim joy. You are not behind; you are in the middle of a story that can bend toward relief with the right hands on the map and your hand on the pen.
Endometriosis is not your fault or your limit. Understanding the biology turns chaos into choices. Track patterns, ask targeted questions, and build a team that thinks together. With informed care and self-compassion, pain can lessen, function can grow, and your life can widen again. You deserve care that adapts and hope that lasts.
If this helped, please leave a comment and tell me what you want covered next. And if endometriosis touches your life, grab the free chapter of my “Endo-Tool: Endometriosis for Men” and join our community for more support, discounts, and practical tools.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MORETheories & Causes for Endometriosis FAQ
1) Is there one proven cause, or many?
There isn’t a single culprit. Endometriosis is best explained by overlapping mechanisms: Sampson’s retrograde menstruation, coelomic/metaplastic change of peritoneal cells, lymphatic/vascular spread, stem-cell seeding, plus genetics, progesterone resistance, and immune dysregulation. That’s why people with the “same” diagnosis can live very different stories.
2) Can endometriosis be prevented?
Short answer: There’s no known way to prevent it. Some guidance focuses on lowering estrogen exposure or treating heavy bleeding early to reduce symptomatic burden, but true prevention isn’t proven. Early recognition and tailored care matter most to reduce long-term impact.
3) Does stage 4 endometriosis change life expectancy?
Endometriosis, even stage 4, doesn’t generally shorten life expectancy, though it can be profoundly life-altering. There is a small increased risk of certain ovarian cancer subtypes, and new evidence that people with endometriosis face higher odds of earlier (often surgical) menopause risks that call for informed monitoring, not panic.
4) How can endometriosis reach the diaphragm or lungs?
The “vascular theory of endometriosis” (benign metastasis) proposes that cells travel via blood or lymph, seeding distant sites; thoracic endometriosis is the clearest example. Coelomic metaplasia and embryonic Müllerian rests likely contribute too, which is why location alone doesn’t prove a single pathway.
5) Do these theories change treatment or fertility planning?
Yes, mechanism guides action. If pain is driven by estrogen dominance/progesterone resistance, hormonal suppression may help; if deep disease distorts anatomy, skilled excision and a fertility plan (IUI/IVF when indicated) can be decisive. Because stage doesn’t reliably predict pain, care must be individualized.
Theories & Causes for Endometriosis References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8951218/
- https://www.eshre.eu/guideline/endometriosis
- https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656
- https://www.ncbi.nlm.nih.gov/books/NBK567777/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10001466/
- https://www.mdpi.com/1422-0067/25/14/7624
- https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2022.879015/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6684338/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11678721/
- https://www.fertstert.org/article/S0015-0282(22)00461-7/fulltext
- https://www.rbmojournal.com/article/S1472-6483(19)30783-7/fulltext
- https://pubmed.ncbi.nlm.nih.gov/1853899/
- https://academic.oup.com/biolreprod/article/92/3/64%2C%201-10/2434026
- https://iv.iiarjournals.org/content/37/5/1922
- https://academic.oup.com/humrep/article/40/6/1094/8115700
- https://obgyn.onlinelibrary.wiley.com/doi/10.1111/jog.16089