10 Interesting Facts About Endometriosis (Rare Facts)
If these interesting facts about endometriosis were true in your body, would it change how you ask for care?
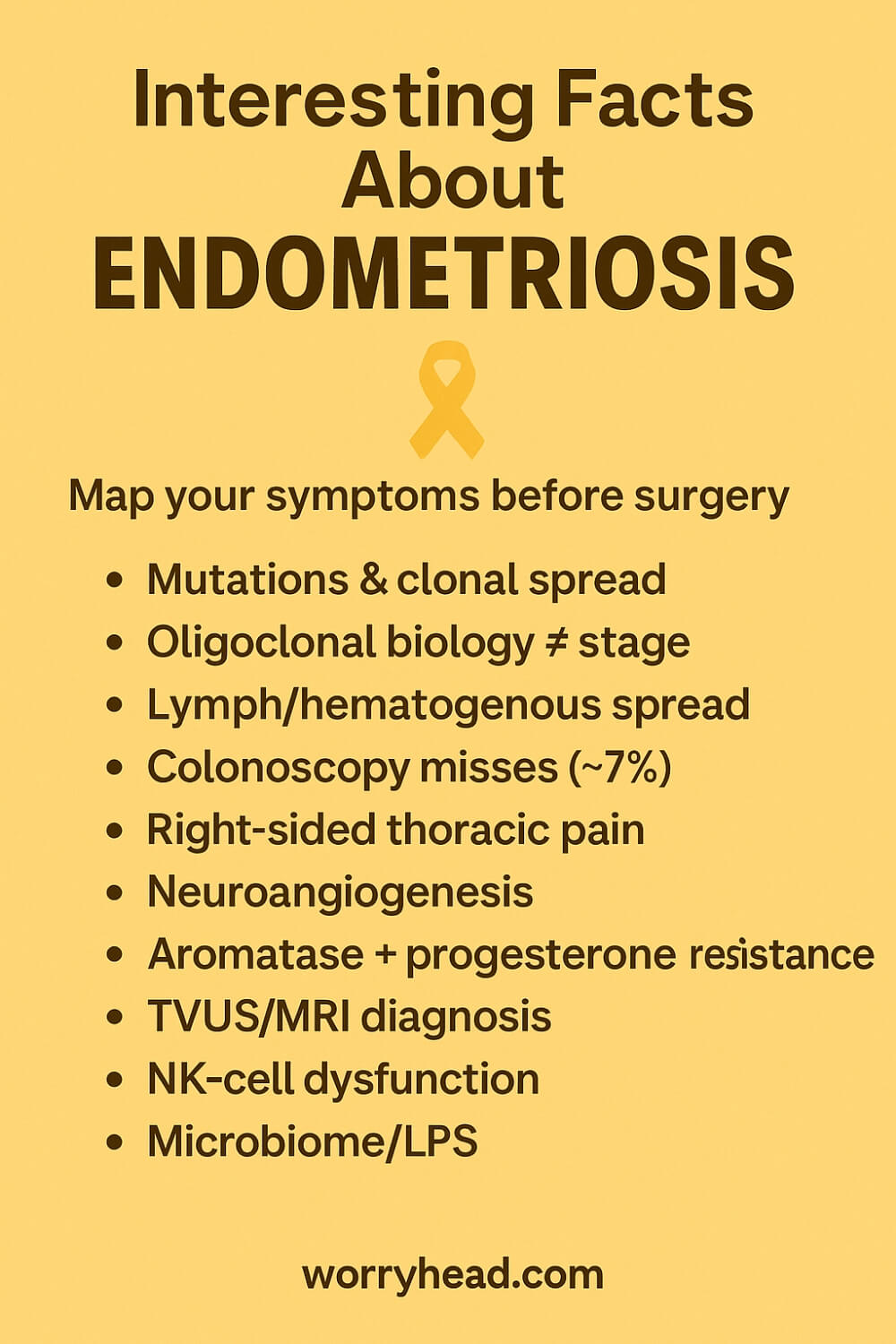
Driver mutations (KRAS/PIK3CA/ARID1A); clonal spread; oligoclonal, stage≠biology; lymph/blood spread; colonoscopy ~7% (outside-in); often right-sided thoracic catamenial pain; neuro-angiogenesis (NGF/IL-1β); aromatase + progesterone resistance; TVUS/MRI dx; low NK cytotoxicity; E.coli/LPS dysbiosis.
What most people never hear is how these mechanisms weave together in real life: genetics shaping where pain shows up, immune brakes failing, imaging revealing deep disease before a scalpel ever touches skin. Newer diagnostics and multidisciplinary care are changing outcomes, but only when we know what to ask for.
I know this because I live beside it. My wife’s pain did not match what simple checklists predicted, and learning the biology helped me show up better, ask better questions, and protect her energy on the days it all felt too much.
If this topic touches your life, you can grab a free chapter of my “Endo-Tool: Endometriosis for Men.” By joining, you also enter our community where I share more freebies, meaningful discounts on our books, and real, practical support for adjusting to the new normal chronic illness brings to love and daily life.
- 10 Interesting Facts About Endometriosis
- Cancer-Driver Mutations and Clonal Spread
- Oligoclonal Disease, Stage Not Biology
- Lymphatic and Hematogenous Dissemination Routes
- Colonoscopy Can Miss Bowel Disease
- Thoracic Involvement Frequently Right-Sided Predominance
- Neuroangiogenesis and Inflammatory Pain Drivers
- Aromatase Activity and Progesterone Resistance
- Imaging Can Diagnose Deep Disease
- NK-Cell Dysfunction and Immune Targets
- Microbiome and Endotoxin-Driven Inflammation
- Interesting Facts About Endometriosis
- Final Word on Interesting Facts About Endometriosis
- Interesting Facts About Endometriosis FAQs
- interesting facts about endometriosis References
10 Interesting Facts About Endometriosis
Most people hear fragments about pain, cysts, and surgery, but the story is bigger and more precise than that. Things such as genetics, immune signaling, imaging advances, and even the gut all shape how this disease behaves and why it is so often misunderstood.
Deep infiltrating disease can be mapped before a scalpel ever touches skin. Expert transvaginal ultrasound and pelvic MRI reveal patterns that explain severe pain even when a routine exam looks “normal.”
Molecular studies show some lesions share the same mutations across different sites, hinting at clonal spread and reminding us that anatomy-based staging can miss the biology driving symptoms.
Outside-in bowel involvement is frequently invisible to colonoscopy, which explains why “your scope was fine” does not end the conversation when bowel pain persists.
Thoracic involvement exists, and it is often right-sided, one reason cyclical chest or shoulder pain deserves a careful, pattern-aware evaluation rather than dismissal.
Pain itself is wired in: lesions sprout vessels and nerve fibers, and inflammatory messengers like NGF and IL-1β vary by subtype, shaping pain severity beyond visible extent.
Hormones complicate the map. Ectopic tissue can synthesize estrogen via aromatase while resisting progesterone, which helps explain mixed responses to standard hormonal therapy.
Immune defenses falter too. Reduced NK-cell cytotoxicity and broader immune dysregulation help ectopic tissue persist, opening doors to new treatment targets.
Add a microbiome dimension, bacterial products like LPS may amplify pelvic inflammation—and you begin to see why simple explanations fail and why multidisciplinary care matters.
I learned this the slow way, beside my wife. What the leaflets missed, the science clarified, and it changed how I protected her energy, which questions I asked, and when we pushed for specialist imaging and referrals. Below are the rare, practical truths I wish we’d been handed on day one, the foundation for the life-useful tips that follow.
- Cancer-driver mutations and clonal spread
- Oligoclonal disease: stage ≠ biology
- Lymphatic/hematogenous routes and nodes
- Colonoscopy can miss bowel disease (~7%)
- Thoracic/diaphragmatic involvement, often right-sided
- Neuroangiogenesis and inflammatory pain drivers
- Aromatase activity and progesterone resistance
- Imaging can diagnose deep disease (TVUS/MRI)
- NK-cell dysfunction and immune targets
- Microbiome/endotoxin contribution to inflammation
Cancer-Driver Mutations and Clonal Spread
Endometriosis isn’t just “tissue out of place”, some lesions carry cancer-driver–type mutations such as KRAS, PIK3CA, or ARID1A even when there’s no cancer present. That matters because identical mutations can appear in lesions at different sites, implying a shared cellular origin and clonal spread.
This helps explain why symptoms can migrate or reappear after incomplete excision. We are not dealing with isolated islands but with connected outposts seeded from the same epithelial clones.
For care, it means pathology and surgical strategy should consider biology, not only location. When I learned this standing beside my wife, it reframed setbacks: a “new” nodule wasn’t a failure of willpower, it was how this disease behaves, complex, cellular, persistent.
Knowing that changed the questions we asked and the specialists we sought.
Oligoclonal Disease, Stage Not Biology
Traditional staging leans on anatomy, how many lesions, how deep, which organs. Yet genetic profiling shows oligoclonality: lesions in one person can be genetically related, but not identical, reflecting multiple evolving clones.
This means a low anatomic stage can still produce severe, neuropathic pain, while a “high” stage might be quieter. Biology drives burden.
Clinically, it argues for individualized plans: precise imaging, targeted excision by an expert team, and adjuvant approaches that address inflammation and nerve ingrowth. For us, abandoning the idea that “stage equals suffering” was freeing.
It validated my wife’s pain on days when scans looked “mild” and gave us a roadmap that prioritized function, not just pictures.
Lymphatic and Hematogenous Dissemination Routes
Reports of nodal involvement and case-mapped tracks along lymphatic channels suggest the disease can travel beyond local peritoneal spread. Hematogenous routes likely explain distant sites like thorax, diaphragm, even rare brain or skin deposits.
This doesn’t mean malignancy; it means endometrial-like cells can hitch a ride in the body’s highways.
Why it matters: surveillance and symptom-pattern awareness should reach beyond the pelvis when red flags appear, cyclical chest pain, shoulder tip pain, unusual coughs around menses. In our journey, recognizing these routes prevented gaslighting.
When my wife described right-sided chest tightness once a month, we had language and a mechanism to push for the correct referrals.
Colonoscopy Can Miss Bowel Disease
Bowel endometriosis typically grows from the outside inward, affecting the serosa and muscularis before ever touching the mucosa. Colonoscopy inspects the lumen; if the mucosa is intact, findings can be “normal.”
Sensitivity estimates as low as ~7% have been reported, which is why a negative scope cannot rule out disease.
What helps instead? Expert transvaginal ultrasound with bowel prep or high-resolution pelvic MRI interpreted by specialists. For my wife, normal scopes once shut doors. Later, targeted imaging showed deep nodules the camera could never see.
The lesson: the right tool for the right layer, and a second opinion when symptoms and tests don’t match.
Thoracic Involvement Frequently Right-Sided Predominance
Thoracic and diaphragmatic endometriosis can cause catamenial pneumothorax, hemothorax, or cyclical shoulder and chest pain. Strikingly, the pattern is predominantly right-sided, likely due to peritoneal fluid dynamics and diaphragmatic fenestrations.
Because it’s rare, it’s often dismissed as anxiety or “costochondritis.”
If symptoms flare within 24–72 hours of menses, ask for imaging timed to your cycle and thoracic surgical input familiar with endometriosis. We learned to track dates, triggers, and side.
When my wife’s shoulder ached like clockwork, that diary carried more weight than any single X-ray, opening a path to clinicians who recognized the pattern.
Neuroangiogenesis and Inflammatory Pain Drivers
Lesions recruit blood vessels and sprout nerve fibers, neuroangiogenesis, turning biological noise into a pain amplifier. Molecules like NGF and IL-1β vary by lesion subtype, shaping sensitivity and flare intensity.
This is why pain can be disproportionate to what’s visible during surgery, and why it can feel electric, burning, or radiating.
Care that targets nerves and inflammation, precise excision, pelvic floor therapy, neuropathic agents, lifestyle anti-inflammatory strategies, can downshift the volume.
With my wife, pacing, heat, and nerve-savvy physiotherapy were not “soft” add-ons; they were part of rewiring a system that had been hijacked.
Aromatase Activity and Progesterone Resistance
Ectopic lesions can synthesize their own estrogen via aromatase while resisting progesterone’s calming signals due to epigenetic changes. That combo fuels growth and blunts response to some hormonal therapies.
It explains why two people on the same regimen can have opposite outcomes—and why trials of therapy need time and backup options.
When a treatment failed, we stopped blaming ourselves. We asked instead: is this a pharmacologic mismatch to the lesion biology?
That shift led us to specialists who could adjust modalities, consider add-backs, or pivot entirely, treating us as partners rather than a protocol to be forced.
Imaging Can Diagnose Deep Disease
Expert transvaginal ultrasound (with bowel prep when indicated) and pelvic MRI can map deep infiltrating disease with high accuracy. Done by the right hands, imaging becomes a surgical blueprint rather than a vague suggestion.
It can identify bowel, bladder, ureteral, and compartment involvement before the operating room-reducing surprises and incomplete excision.
For us, getting to an imaging team that speaks the language of compartments changed everything. The report read like a plan, not a mystery. It guided referrals, protected fertility considerations, and set expectations honestly, one of the most compassionate forms of care we experienced.
NK-Cell Dysfunction and Immune Targets
Immune surveillance is blunted in endometriosis, with reduced NK-cell cytotoxicity and other dysregulations that let ectopic tissue persist. This isn’t weakness but a specific immune phenotype.
Understanding this opens doors to trials exploring immunomodulation and explains why infections, stress, or sleep loss can magnify symptoms.
We built an “immune-friendly” routine: regular sleep, stress buffering, gentle movement, nutrition that tames inflammation.
None of it was a cure, but together they raised the floor. On crash days, remembering there’s an immune reason, not a moral failing, kept our hope intact and our plan steady.
Microbiome and Endotoxin-Driven Inflammation
The pelvic environment is not sterile. Studies implicate dysbiosis and bacterial products like LPS in amplifying inflammation, the bacterial contamination hypothesis.
Evidence is mixed but increasingly compelling.
Practically, that means gut health can be a lever: fiber diversity, targeted probiotics when appropriate, and care for coexisting IBS-like symptoms.
When my wife’s flares paired with gut upheaval, we treated the axis, not just the pelvis, hydration, low-FODMAP trials under guidance, and steady, realistic nutrition.
No miracle cures, just small, evidence-respecting steps that, combined with surgical and medical care, made the bad weeks less devastating.
Interesting Facts About Endometriosis
Endometriosis is now framed as a chronic inflammatory disease, not just “tissue out of place”, with cells similar to the uterine lining found outside the uterus and capable of driving pain, fatigue, and fertility challenges.
Around one in ten women and people with female reproductive systems are affected worldwide, a scale that explains why so many families feel its impact across work, relationships, and plans for the future.
Delays remain stubborn because research groups still report multi-year diagnostic journeys, though new work aims to shorten this with smarter pathways and potential non-invasive tests under investigation.
Treatment is evolving, too. In England, a combined daily pill (relugolix-estradiol-norethisterone) was approved for selected patients, offering a home-use option that may avoid injection visits and hasten symptom control for some.
Behind the headlines, big data studies and molecular profiling are mapping patterns, who gets which subtype, why pain can be severe despite “minimal” imaging, and how biology should steer care instead of anatomy alone.
For my wife, those shifts weren’t abstract. A precise definition of the disease validated her symptoms when routine tests looked normal, and knowing that better diagnostics and therapies exist helped us ask for the right referrals at the right time.
We learned to track cycles, triggers, and “odd” symptoms like shoulder-tip pain, because awareness, paired with knowledgeable clinicians, can catch extra-pelvic disease that standard pathways miss.
We also learned that progress rarely comes from one lever. It’s the mosaic: specialist imaging, evidence-based medical options, targeted surgery when indicated, pelvic floor rehab, pain-science-informed strategies, and lifestyle changes that lower the inflammatory load.
On hard days, the goal wasn’t perfection; it was protecting her energy budget and preserving the parts of life that make her feel most herself. That meant pacing, kinder schedules, and building a work-from-home rhythm that didn’t punish her body for trying.
If you’re reading this as a partner, know that your steadiness matters. Ask better questions. Keep records. Help translate science into appointments and daily choices. It won’t fix everything, but it will move you both from confusion toward a plan.
Final Word on Interesting Facts About Endometriosis
Stepping back from the science, what these rare, precise truths really give us is a map, a way to see the whole terrain instead of a handful of road signs that never quite explained your pain.
When I first learned that lesions can share the same mutations across different sites, that anatomy alone can miss the biology, that bowel disease can hide from a colonoscope, something clicked.
We weren’t chasing ghosts; we were dealing with a cellular, immune, and neurological problem that behaves exactly as the research predicts.
That understanding didn’t erase my wife’s pain, but it turned guesswork into strategy.
Knowing that lesions wire themselves into nerves helps make sense of why pain feels electric or out of proportion to what a scan shows.
Recognizing aromatase activity and progesterone resistance explains mixed responses to medications and stops the spiral of self-blame when a standard approach falls flat.
Realizing that thoracic or diaphragmatic involvement can be right-sided and cyclical gives language to symptoms that too often get dismissed as anxiety. Each piece replaces doubt with vocabulary you can bring into the clinic, the imaging suite, or the operating room.
And then there’s the quiet power of timing and tools. Expert ultrasound and MRI, when read by people who speak this disease, can sketch a surgical blueprint in advance.
That alone can spare you partial answers and repeated procedures. Pair those images with immune-aware living, adequate sleep, stress buffering, movement paced to your reality, nutrition that calms rather than inflames, and you build a floor under the hard days.
It’s not a miracle; it’s what consistent, humane care looks like when biology leads.
As a partner, I learned to measure progress in smaller wins: a flare cut shorter, a week with fewer spikes, a day she could keep the plans that matter. I learned that love looks like record-keeping, like refusing to accept “normal tests” as the end of the conversation, like making home a place where her nervous system can stand down.
The facts in this article aren’t trivia. They’re handles you can hold when the system feels slippery, evidence that your experience isn’t an outlier, it’s a pattern we can prepare for.
If you’ve carried doubt because your story didn’t match the brochure version of this condition, take these findings as permission to advocate without apology.
Ask for cycle-timed imaging. Query right-sided chest pain. Push for teams who treat biology, not just pictures. You deserve care that is as sophisticated as the disease itself, and a life that leaves room for joy in spite of it.
In short: precision isn’t cold; it’s compassionate. It gives you words, choices, and the confidence to build a plan that protects your body and your future.
Your story matters, and you’re not alone. Keep going, one informed decision, one kinder day, one brave appointment at a time.
If this resonated, I’d love to hear your voice below. Leave a comment. And if you want more practical, compassionate guidance, you can grab a FREE chapter of my “Endo-Tool: Endometriosis for Men.”


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MOREInteresting Facts About Endometriosis FAQs
1) Can endometriosis be diagnosed without laparoscopy?
Yes. In skilled hands, transvaginal ultrasound and pelvic MRI can map deep disease, including bowel, bladder, or ureter involvement. Imaging does not treat the condition, but it can guide the right team and surgical plan when needed. For us, expert imaging turned confusion into a clear next step.
2) Why did my colonoscopy come back normal if I have bowel symptoms?
Bowel endometriosis usually grows from the outside of the bowel inward, so the inner lining that a colonoscope sees can look normal. Sensitivity of colonoscopy for this is very low. Ask for specialist pelvic imaging, ideally ultrasound with bowel prep or dedicated pelvic MRI read by an endometriosis-experienced radiologist.
3) My scans say “minimal disease,” yet my pain is severe. How is that possible?
Anatomy does not always reflect biology. Lesions can be genetically related, wire into nerves, and secrete inflammatory signals that amplify pain. That is why small-appearing disease can still be disabling. Validating this mismatch helped me advocate better for my wife and push for care that treated the biology, not just the picture.
4) Can endometriosis affect the chest or shoulder, and why is it often right-sided?
Yes. Thoracic and diaphragmatic involvement can trigger cyclical chest tightness, shoulder tip pain, or even pneumothorax around menstruation. Right-sided patterns are common, likely related to fluid flow and tiny openings in the diaphragm. If symptoms cluster around your cycle, ask for evaluation by clinicians familiar with thoracic endometriosis.
5) Do hormone treatments always work if lesions make their own estrogen and resist progesterone?
Not always. Some lesions express aromatase and show progesterone resistance, which can blunt response to standard regimens. That does not mean there are no options. It means therapy may need adjusting or combining, guided by symptom tracking, side-effect tolerance, and imaging findings, with surgical consultation when appropriate.
interesting facts about endometriosis References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5555376/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10240146/
- https://www.sciencedirect.com/science/article/pii/S0015028222003399
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4408473/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6684338/
- https://www.jmig.org/article/S1553-4650%2821%2900384-8/abstract
- https://www.eshre.eu/-/media/sitecore-files/Guidelines/Endometriosis/ESHRE-GUIDELINE-ENDOMETRIOSIS-2022_2.pdf
- https://www.nice.org.uk/guidance/ng73
- https://www.nice.org.uk/guidance/ng73/resources/visual-summary-on-first-presentation-initial-management-diagnosis-referral-and-ongoing-care-of-pdf-13559822461
- https://www.mdpi.com/2218-273X/14/5/583
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4880704/
- https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1657605/full
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5902457/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10265574/