10 Interesting Facts About Fibromyalgia (Rare Facts)
Have you ever wondered if the interesting facts about fibromyalgia reveal a biology far deeper than just “sensitivity to pain”?
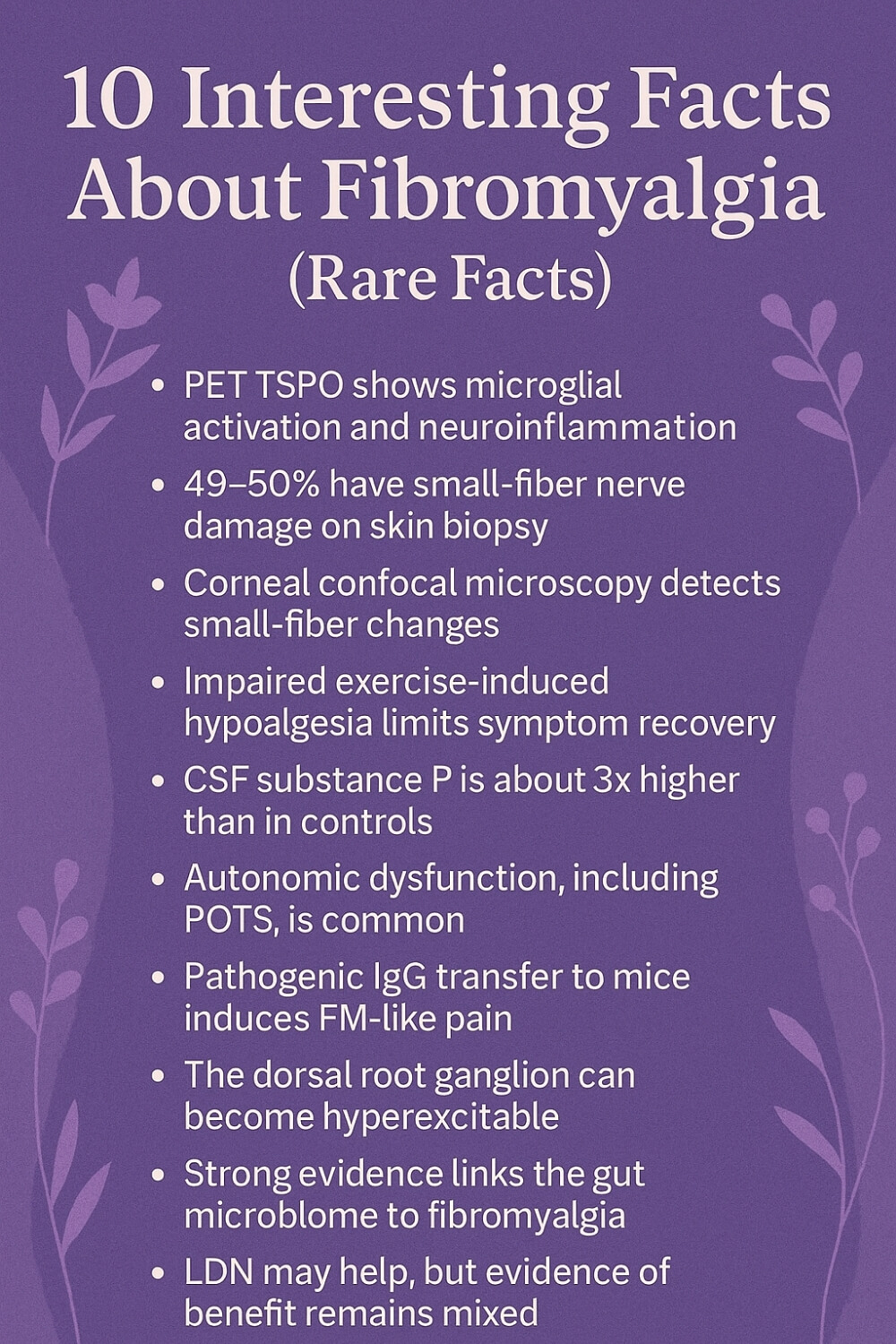
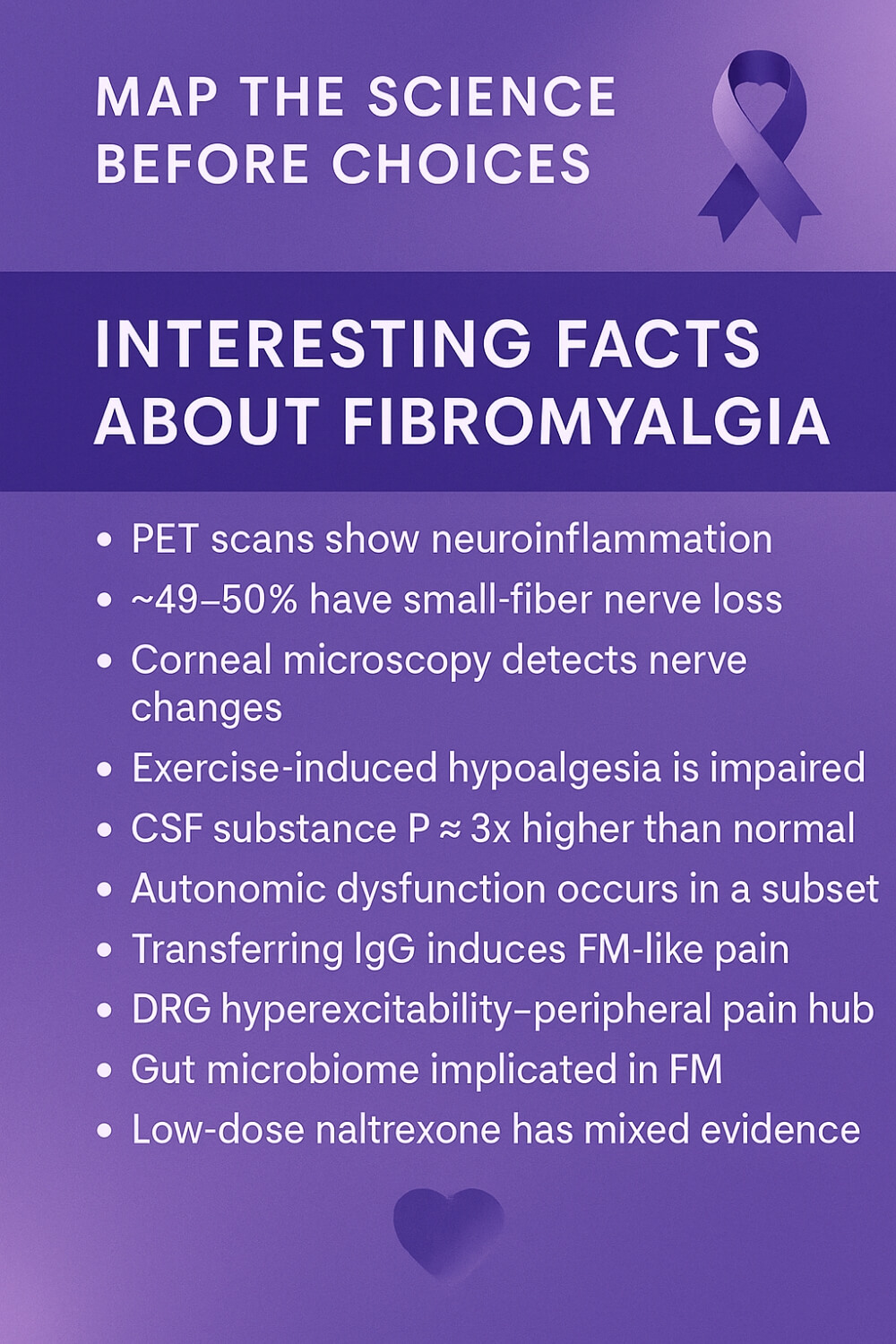
TSPO PET shows microglial activation; ~50% with small-fiber loss on biopsy; corneal confocal microscopy mirrors biopsy; exercise hypoalgesia impaired; CSF substance P ~3×; autonomic dysfunction incl POTS; IgG causes DRG pain; DRG hyperexcitable outside BBB; gut dysbiosis implicated; 2024 LDN RCT negative, meta-analyses mixed.
What surprises researchers today is how these findings connect: immune signals, gut microbes, nerve fibers, and even antibodies forming a web that keeps amplifying pain. New therapies are being tested, and in August 2025 the FDA approved Tonmya, a bedtime sublingual tablet, as the first official drug for fibromyalgia, marking a shift in recognition.
Emerging tools like deep-learning MRI models that replicate PET results are also giving hope for easier, non-invasive diagnostics. These aren’t just lab curiosities, they’re steps toward changing daily life for millions.
For me, this isn’t only about science. It’s about sitting beside my wife on nights when pain robs her of rest, knowing that behind her struggle is evidence, not weakness. Each new discovery gives us words, proof, and a little more courage to demand better care.
If this resonates with you, I invite you to grab 3 free chapters of my book “Fibromyalgia for Caring Partners.” By joining, you also become part of our community where I share more free resources, discounts on all my books, and heartfelt guidance to help couples adjust to the new normal chronic illness brings.
Interesting Facts About Fibromyalgia
When you pull the science together, a clearer picture emerges than the old “it’s just sensitivity” line. Fibromyalgia reflects changes in how the nervous system processes signals, plus immune and autonomic patterns that keep pain switched on.
Authoritative overviews now emphasize central sensitization alongside sleep disruption, cognitive fog, and fatigue, which fits what many of us see at home.
Fresh 2025 news matters for real life. For example, in August 2025 the FDA approved Tonmya, a bedtime sublingual tablet, as the first new therapy for fibromyalgia in more than 15 years, with commercial availability expected by late 2025. Early summaries highlight pain reduction in late-stage trials and a focus on non-restorative sleep.
Researchers are also testing objective markers that could move diagnosis beyond checklists.
Brain PET studies using TSPO tracers visualize microglial activation, and machine-learning MRI approaches are being explored to approximate those patterns without radiation.
This is exciting because it points to measurable biology rather than vague labels. (For background, see major clinical summaries on symptom biology.)
Immune and autonomic threads keep showing up. Meta-analyses and trials around low-dose naltrexone are mixed: a 2024 randomized study of 6 mg daily did not outperform placebo, while pooled reviews suggest possible benefit and good tolerability, so expectations should stay balanced.
Small-fiber pathology is another reproducible finding. Roughly half of patients show small-fiber loss on skin biopsy in pooled cohorts, and corneal confocal microscopy often mirrors biopsy results, raising the prospect of less invasive monitoring.
Autonomic testing, including tilt-table studies for POTS, can explain dizziness and palpitations in a meaningful subset. These are not fringe ideas; they are measurable signals clinicians can act on.
Exercise still helps, but the body’s built-in pain brake, called exercise-induced hypoalgesia, can be blunted in fibromyalgia, which is why graded, compassionate programs outperform “push through it” plans. That nuance can save months of frustration.
I have watched all of this from the side of the bed, one hand on my wife’s back while she tries to sleep. Science gave us language we could bring to appointments and the patience to pace recovery without shame. If you are reading this in the quiet after a hard day, I want you to know that what you feel is real and there are practical steps that help.
Below is the compass I wish we had on day one. It is a short list of rare, precise truths that turn confusion into a plan. These are the fibro facts that will guide the tips and deep dives that follow:
- PET TSPO studies show widespread microglial activation
- Around 49–50% show small-fiber loss on skin biopsy
- Corneal confocal microscopy reflects small-fiber pathology
- Exercise-induced hypoalgesia is impaired
- CSF substance P is about three times higher than controls
- Autonomic dysfunction, including POTS, is common
- Patient IgG can induce FM-like pain and DRG changes in mice
- The dorsal root ganglion can become hyperexcitable outside the BBB
- Gut dysbiosis appears contributory and is a therapeutic target
- Low-dose naltrexone evidence is promising but mixed, with a 2024 6 mg RCT negative
PET Evidence of Neuroinflammation
TSPO PET studies consistently show elevated signal in pain-processing regions, which points to microglial activation rather than a vague, unprovable “sensitivity.”
This matters because inflammation inside the central nervous system can keep the volume knob stuck on loud. When I sit beside my wife at 3 a.m., this is what I remember: the scans match the story her body tells. It also reframes treatment goals.
We look for strategies that calm neuroimmune crosstalk, protect sleep, and reduce triggers that pour fuel on microglia. You are not imagining it, and you are not weak. A brain that has been taught to protect you too hard can be taught, gently and repeatedly, to stand down.
Small-Fiber Loss on Biopsy
Around half of people with fibromyalgia show reduced epidermal nerve fiber density on skin biopsy. That is anatomy you can measure, not a personality trait. It explains burning, tingling, and those odd maps of pain that do not follow classic dermatomes.
For my wife, having a biological explanation reduced the shame that decades of dismissal had built. It also guided care.
Clinicians were more willing to consider neuropathic agents, targeted rehab, and lifestyle levers that support peripheral nerve health. When pain finally made sense, pacing and patience became investments, not punishments, and the house felt less like a courtroom.
Corneal Confocal Microscopy Marker
Corneal confocal microscopy offers a non-invasive window into small-fiber pathology. The cornea is densely innervated, so changes there often mirror what a skin biopsy would show. That opens the door to tracking progression and response without repeated punches to the calf.
It also gives couples like us a way to talk about the condition that is concrete. If a simple eye scan can validate what a patient feels, we can move faster to the right plan. Hope is not a slogan here, it is an evidence trail that helps you and your clinician choose tests wisely and avoid dead ends.
Exercise Pain-Brake is Blunted
In many people with fibromyalgia, exercise-induced hypoalgesia, the body’s internal pain brake, does not kick in properly. This is why “just push harder” often backfires.
We learned to swap heroics for calibration. Short sessions, consistent cadence, and gentle progress protect the nervous system while still unlocking the benefits of movement. The win is not beating yesterday’s numbers. The win is teaching biology to trust activity again.
When my wife trained this way, crashes shortened, sleep deepened, and the next day was not lost. Smart training is not weakness, it is science applied to real life.
CSF Substance P is Higher
Cerebrospinal fluid studies report substance P levels roughly triple those of controls, which fits the lived experience of amplified signaling. This neuropeptide lowers pain thresholds and keeps alarms ringing long after the danger is gone.
Knowing this helped us separate character from chemistry. It is not that she is dramatic, it is that the messenger molecules are loud.
Our plan shifted toward quieting the system: sleep quality first, gentle breath work, temperature therapy, and medications that make sense for central sensitization. When you target the biology, the story stops being self-blame and starts being strategy.
Autonomic Dysfunction and POTS
Autonomic testing frequently uncovers orthostatic intolerance or full POTS, which explains dizziness, palpitations, brain fog, and that strange “I am crashing in the supermarket queue” feeling.
Naming it gives you levers: salt and fluid strategies if appropriate, compression, recumbent exercise, and medication when needed.
For us, recognizing the autonomic piece reduced arguments with our own expectations. We planned morning tasks seated, stacked errands, and placed chairs in every room.
The goal was not to “tough it out” but to keep blood where the brain needs it. Function improved when physiology finally had a seat at the table.
Patient IgG Can Transfer Pain
Experiments that transfer IgG from fibromyalgia patients to mice reproduce pain-like behaviors and dorsal root ganglion changes. That suggests at least a subset has an autoimmune-style driver. It is early science, but it changes the conversation.
You are not “catastrophizing,” your immune system may be mis-teaching your nerves. For couples, this is strangely freeing. We stop fighting ghosts and start tracking flares with infections, stress, and hormonal shifts that modulate immunity.
It also focuses clinic visits on options that cool antibody-driven processes, while keeping lifestyle gentle so the nervous system can relearn safety.
DRG as a Pain Hub
The dorsal root ganglion sits outside the blood–brain barrier and can be primed into hyperexcitability, turning normal signals into pain. Think of it as a crowded train station where alarms keep tripping.
Calming the DRG means reducing bombardment: comfortable clothing, movement that avoids repetitive strain, and treating peripheral inputs like small-fiber loss or joint instability.
In our home, that looked like different chairs, kinder shoes, and micro-breaks on any task that required grip or heat. Small upgrades multiplied, and the noise dropped. The win is not perfection, it is reclaiming enough quiet to live.
Gut Dysbiosis as a Driver
Systematic reviews link altered microbiomes with symptom severity, and mechanistic work points to the gut–brain–nerve axis as a target. Translation for daily life: steady fiber diversity, smart probiotic use when indicated, and gastrointestinal care for IBS-type symptoms can take pressure off the pain system.
We learned to respect the plate as much as the pill.
Regular meals, hydration, and gentle experimentation under guidance gave us fewer flare-gut-flare spirals. It is not a miracle diet, it is reducing one of the loudest amplifiers in a body that already deals with too much noise.
Low-Dose Naltrexone, Mixed Data
Low-dose naltrexone remains promising yet inconsistent.
A well-run 2024 trial using 6 mg daily did not beat placebo, while meta-analyses that pool smaller studies suggest benefit and good tolerability. Here is how we hold that tension at home.
We set realistic expectations, monitor sleep and function, and if we try LDN, we pair it with non-drug strategies and a clear stop rule. Hope is allowed, hype is not. The point is not to collect medications, the point is to collect better days.
When a tool helps, keep it. When it does not, bless it and move on.
Fibromyalgia Facts
The science points to a body trying to protect itself too hard, and our job is to teach it safety again. That starts by mapping patterns without shame. Track sleep depth, food timing, stress spikes, temperature, hormones, and recovery after any activity.
When you see the loops, you can loosen them. Short, regular movement builds a tolerance bank that the nerves can trust. Think five or ten quiet minutes, most days, instead of heroic bursts that steal tomorrow.
Sleep is treatment. Guard a wind-down ritual, dim lights, cool the room, and keep wake times steady. If pain interrupts, rehearse a brief script you can do in the dark: breath work, heat, gentle stretches, and back to bed.
Pain education is not blame. It is learning how nervous systems amplify signals and how attention, fear, and overprotection add volume. When you understand the mechanics, setbacks feel less like failure and more like physics you can nudge.
Nourish the gut and blood volume. Regular meals with fiber variety, hydration salted to your clinician’s advice, and compression on upright days can tame dizziness and brain fog. Treat constipation aggressively so it does not become a daily pain trigger.
Pace life like an athlete with a fragile hamstring. Alternate tasks, change position often, and keep micro-breaks on purpose. Home ergonomics matter more than you think: chair height, foot support, softer fabrics, and tools with larger grips reduce peripheral bombardment.
Build a small team. A primary clinician who listens, a physio who understands central sensitization, maybe a psychologist for pacing and fear of movement, and a pharmacist who simplifies the regimen. Fewer, better levers beat a drawer full of half-measures.
I learned all this beside my wife, counting breaths while she waited for a flare to pass. The day we stopped proving strength and started protecting it, our home got quieter. If you are reading this alone at midnight, you are not failing. You are learning a new language of care, one careful habit at a time.
Understanding mechanisms turned our home into a place where biology sets the agenda and we respond with care, not panic. We learned that small wins compound: a steadier wake time, a calmer wind-down, a shorter walk done more often.
When pain spikes, I don’t push her to “power through.” I lower the noise: dim lights, fewer decisions, gentle heat, and tasks she can do seated. The goal is to teach a jumpy nervous system that it is safe.
Autonomic swings used to blindside us in shop queues and waiting rooms. Now we pre-load fluids and salt as advised, carry snacks, and plan sit-breaks before the dizziness whispers.
Movement is medicine but only when the dose is right. We keep sessions brief, repeatable, and kind, choosing what her body can trust tomorrow, not just survive today.
Sleep sits at the center. We defend it with darker evenings, cooler air, and the same wake time even after rough nights. If pain wakes her, we use a short script—breath, stretch, back to bed—so the night doesn’t unravel.
Food is part of the plan, not a battlefield. Regular meals, fiber variety, and gut-soothing choices prevent that flare-gut-flare loop that used to steal entire weekends.
At my desk I changed the chair, raised the screen, added a footrest, and swapped tight clothes for soft fabrics. Tiny ergonomic edits spared her nervous system a thousand paper cuts a day.
We also track patterns without judgment. If a new symptom lines up with stress, infection, or hormones, we adapt the week instead of blaming the willpower that never caused this.
Most of all, we make room for joy on purpose. A short drive to her favorite view counts. Ten minutes of sunlight counts. When life is measured in energy coins, spending a few on meaning is therapy too.
I carry the lists, ask the questions, and protect the margins so she can keep the parts of life that feel like her. That is what partnership looks like here, informed by the interesting facts about fibromyalgia and translated into ordinary, repeatable care.
Final Word on Interesting Facts About Fibromyalgia
When I first began learning what was really happening in my wife’s body, I expected answers to arrive like switches: off, on, fixed. Instead, understanding came like dawn, quiet, gradual, undeniable.
The science is not a verdict on her character; it is a map of nervous system, immune crosstalk, and small fibers trying to protect her a little too hard. Once we named the patterns, we could work with them.
We stopped asking why she wasn’t tougher and started asking how we could make her days gentler, safer.
Clarity turned appointments into collaborations.
We brought symptom diaries instead of apologies. We timed experiments, adjusted doses, and guarded sleep like a treatment, not a luxury. Movement stopped being a test of grit and became a way to teach her body that the world is mostly safe.
On paper, those are small changes. In our home, they were the difference between spirals and second chances.
There is no single lever to pull. Some days call for pacing and quiet, others for short walks and sunlight. We learned to respect the autonomic system with fluids, salt when appropriate, and seated breaks before standing becomes a cliff.
We learned to protect the gut so it would stop amplifying pain. We chose clothing, chairs, and schedules that do not scrape at the dorsal root ganglion’s patience. Nothing in that list is flashy, yet together they lower the baseline noise so the bright parts of life can be heard again.
I won’t pretend we don’t still have hard nights. We do. But the hard nights no longer define the week. Knowledge made us kinder to each other.
When she wakes me at 3 a.m., I do not reach for speeches; I reach for heat, water, and the breathing routine we practiced on the good days. When she is ready, we walk the hallway, we smile at the cat, we anchor the nervous system to something ordinary.
Love is a plan you rehearse, not a mood you wait for.
If you are reading this because you want that steadiness in your own home, start small and start now. Track patterns without judgment. Pick one habit you can keep on rough days.
Ask your clinician one precise question at the next visit. Build a team that talks to each other. Let progress be quiet and cumulative. There is strength in refusing to rush healing that cannot be rushed.
Most of all, keep room for joy.
Fibromyalgia can feel like a thief, but it does not get to steal everything. A shared breakfast at the window counts. Ten minutes in the garden counts. The choice to rest before the crash counts. The facts in this article were never trivia; they are handles you can grip when the ground shifts.
Hold them, and hold each other. And if today only yields one tiny win, an earlier bedtime, a calmer breath, a kinder pace, that still counts, because consistency teaches the body it can trust you again.
In short: when biology is understood, care gets kinder and outcomes get steadier. You deserve clinicians who listen, plans that fit your life, and days shaped by choices you can keep. Begin with one small, repeatable habit, protect sleep, and let hope be practical.
If this helped, I would love to hear your story in the comments. You can also grab 3 free chapters of my “Fibromyalgia for Caring Partners.” By joining, you become part of our community, where I share more freebies, meaningful discounts on all my books, and real, practical guidance for the new normal.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MOREInteresting Facts About Fibromyalgia FAQs
1) Is fibromyalgia “just sensitivity,” or is there measurable biology?
There’s measurable biology. Brain PET studies using TSPO tracers show widespread microglial activation in people with fibromyalgia—objective evidence of neuroinflammation rather than a purely subjective problem.
2) Are there any truly new treatments?
Yes. In August 2025, the FDA approved Tonmya (sublingual cyclobenzaprine) for adults with fibromyalgia—the first new approval in more than 15 years—aimed at improving non-restorative sleep and reducing pain. Availability is expected by late 2025.
3) What objective tests can support a diagnosis or phenotype?
About half of patients show small-fiber pathology on skin biopsy; corneal confocal microscopy often mirrors biopsy findings and offers a non-invasive option clinicians increasingly consider alongside clinical criteria.
4) Does exercise help or hurt?
Exercise helps when dosed gently and consistently. A known feature of fibromyalgia is impaired exercise-induced hypoalgesia—the body’s “pain brake”—so graded, patient-centred programs typically outperform “push through it” plans that can provoke flares. (Background reviews and trials discuss this mechanism within FM pathophysiology.)
5) What’s the deal with low-dose naltrexone (LDN)?
Evidence is mixed. A 2024 randomized trial of 6 mg/day did not outperform placebo, while meta-analyses suggest possible benefit and good tolerability—so it’s reasonable to consider with realistic expectations and careful monitoring.
Interesting Facts About Fibromyalgia References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6541932/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10502894/
- https://pubmed.ncbi.nlm.nih.gov/30314675/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9139885/
- https://www.nature.com/articles/srep23573
- https://pubmed.ncbi.nlm.nih.gov/26094164/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7523781/
- https://pubmed.ncbi.nlm.nih.gov/7526868/
- https://pubmed.ncbi.nlm.nih.gov/19007537/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8245181/
- https://pubmed.ncbi.nlm.nih.gov/33409721/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11671092/
- https://pubmed.ncbi.nlm.nih.gov/38260871/
- https://www.thelancet.com/journals/lanrhe/article/PIIS2665-9913%2823%2900278-3/abstract
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11450306/
- https://www.reuters.com/business/healthcare-pharmaceuticals/us-fda-approves-tonix-pharmas-drug-manage-pain-related-chronic-condition-2025-08-15/
- https://www.investors.com/news/technology/tonix-pharmaceuticals-fda-approves-fibromyalgia-drug/
- https://www.biorxiv.org/content/10.1101/2024.09.27.615379v1.full-text
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11464731/
Finally! I gave up hope that anyone would actually research FM. Just knowing I’m not crazy is helpful. Now I know better what is happening. I was diagnosed with FM in 1997 and it’s getting worse. My bug phobias don’t help. I’ve decided to try Lion’s Mane tincture as it’s supposed to help repair nerves and good for the immune system. Also, reading this tells me to restart B-complex and D3. Thank you for sharing your knowledge with us.