Do you often feel sharp, debilitating pain in your ovaries during ovulation? You might wonder if this pain is linked to endometriosis. Many women have this concern because ovulation pain, or Mittelschmerz, can signal endometriosis.
Endometriosis is a chronic, often misunderstood disease. It affects about 1 in 10 women and those assigned female at birth. It happens when tissue like the uterus lining grows outside the uterus, causing inflammation and scarring. This can lead to severe ovulation pain and other symptoms like heavy, painful periods and infertility.
If you have persistent, severe ovulation pain, understanding its link to endometriosis is key. Getting the right medical help can help you manage your pain long-term. In this article, we’ll look into the connection between ovary pain and endometriosis. We aim to give you the info you need to take care of your health.
What Is Ovulation Pain?
Ovulation pain, also known as mittelschmerz, is a common experience during the menstrual cycle. It’s a one-sided, lower abdominal pain that can last from a few minutes to a few hours. Sometimes, it can last up to 48 hours. This pain is linked to the release of an egg from the ovary, a natural process called ovulation.
Symptoms of Ovulation Pain
Ovulation pain feels like a dull, nagging, or cramping sensation in the lower abdomen or pelvis. It usually happens on the same side as the ovary releasing the egg. The pain can switch sides or stay on the same side for months. Sometimes, it’s accompanied by nausea or a mild fever.
Causes of Ovulation Pain
The exact cause of ovulation pain is not fully understood. It’s thought to be due to the growth and rupture of the egg follicle. As the follicle grows, it can stretch the ovary, causing discomfort. The release of blood or fluid from the ruptured follicle may also irritate nearby tissues, adding to the pain.
While ovulation pain is a normal part of the menstrual cycle for many women, severe or persistent pain may signal an underlying issue. This could include endometriosis. If the pain is severe, lasts longer than usual, or is accompanied by other concerning symptoms, seeing a healthcare provider is important.
Ovulation pain affects about one in five women. It usually starts a few years after menstruation begins and can last from a few minutes to 48 hours. In the last six months, 10% of Clue users have reported ovulation pain at least once.
Endometriosis and Its Connection to Ovulation Pain
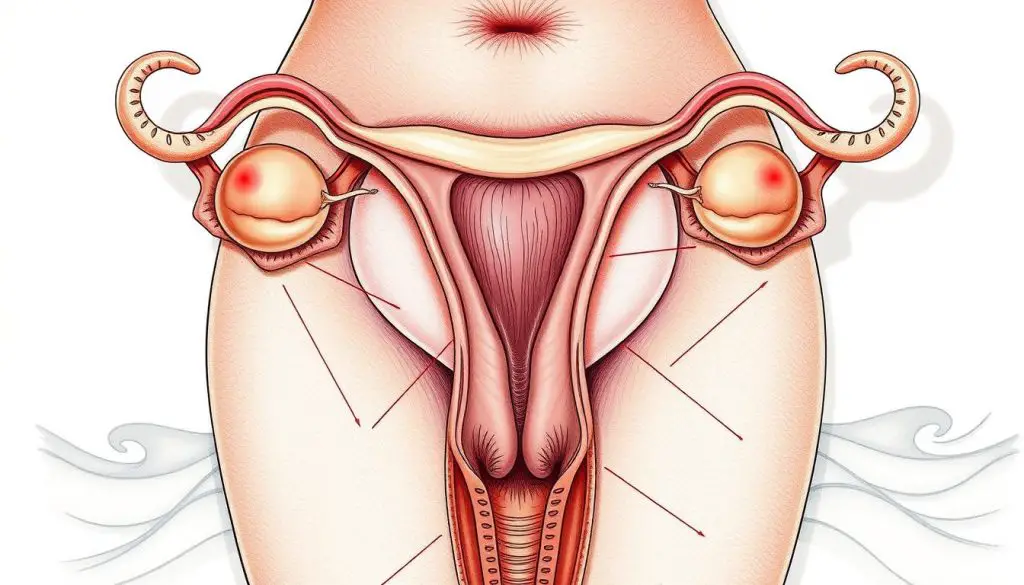
Endometriosis is a chronic condition where tissue like the lining of the uterus grows outside the uterus. It often grows on the ovaries, fallopian tubes, and other pelvic organs. This tissue reacts to hormonal changes, causing inflammation, pain, and heavy periods. For many, this leads to intense pain during ovulation, known as endometriosis ovulation pain.
How Endometriosis Causes Ovulation Pain
Endometriosis can cause painful ovulation in several ways:
- Endometrial lesions or implants on or around the ovaries and fallopian tubes can cause inflammation and pain during ovulation.
- Scar tissue (adhesions) that forms as a result of endometriosis can put pressure on the ovaries, leading to pain during ovulation.
- Endometriomas, or “chocolate cysts,” can develop on the ovaries, further exacerbating ovulation pain.
- Endometriosis-related inflammation can affect the nerves surrounding the reproductive organs, causing referred pain during ovulation.
The pain from endometriosis during ovulation is often worse, lasts longer, and is more severe than normal ovulation pain, or mittelschmerz. People with endometriosis may also feel intense pelvic pain, nausea, vomiting, and diarrhea during ovulation.
It’s important to understand how endometriosis and ovulation pain are connected. This knowledge helps in finding effective treatments and ways to manage the pain. By treating the endometriosis, healthcare providers can help reduce ovulation pain and improve life quality for those affected.
ovary pain during ovulation: A Common Symptom of Endometriosis
Ovary pain during ovulation is a common symptom of endometriosis. This condition is chronic and can be very painful. Around 40% of menstruating individuals feel pain during ovulation, known as mittelschmerz. But for those with endometriosis, this pain is much worse and lasts longer.
Endometriosis happens when tissue like the uterine lining grows outside the uterus. It often grows on the ovaries, fallopian tubes, or other pelvic organs. These growths cause intense pain during ovulation as they rub against the reproductive organs. This leads to inflammation and discomfort.
The pain from endometriosis is usually more severe and lasts longer. It may also come with other symptoms like:
- Heavy, painful menstrual bleeding
- Painful intercourse
- Chronic pelvic pain
- Digestive issues like nausea, diarrhea, and constipation
If ovary pain during ovulation is affecting your daily life, see a healthcare provider. They can find the cause and help manage your symptoms. This can greatly improve your quality of life.
Where Does Endometriosis Pain Occur?
Endometriosis is a chronic condition where tissue like the uterine lining grows outside the uterus. This misplaced tissue can cause severe pain in various areas of the body. These areas include the lower abdomen, pelvis, rectum, and above the groin.
The pain can spread to the buttocks, legs, and hips if the lesions press against nerves in the pelvis.
Duration and Severity of Endometriosis Pain
Endometriosis pain is usually more severe and lasts longer than normal ovulation pain. It often continues for over 48 hours. The pain is intense, long-lasting, and not relieved by interventions.
Other symptoms include painful intercourse, urination, bowel movements, and pain with vomiting or diarrhea.
Unlike normal ovulation pain, endometriosis pain can be debilitating. It can significantly impact a person’s quality of life. The severity of endometriosis pain varies. Some people experience constant pelvic pain, while others only have pain during their menstrual cycle or ovulation.
The duration and severity of endometriosis pain can vary from person to person. Some may have intermittent discomfort, while others have chronic, unrelenting pain. Seeking medical attention is key for proper diagnosis and management of endometriosis-related pain.

Diagnosing Endometriosis: Tests and Procedures
Diagnosing endometriosis is a detailed process. It’s key to getting the right treatment and managing symptoms. Your doctor might suggest several tests and procedures to find endometriosis accurately.
Ultrasound
A pelvic ultrasound is often the first step. It’s a non-invasive test that can spot endometrial implants or cysts on ovaries. These are called endometriomas or “chocolate cysts.” Ultrasound can’t find all cases, but it’s a good start.
Laparoscopy
If your doctor thinks you might have endometriosis, they might suggest a laparoscopy. This surgery lets them see the pelvic organs and find any endometrial lesions or scarring. Laparoscopy is the best way to confirm endometriosis and see how far it has spread.
Other Diagnostic Tests
- Magnetic Resonance Imaging (MRI): This test gives detailed info on endometrial implants, even in hard-to-reach areas.
- Pelvic Exam: Your doctor will do a thorough pelvic exam to look for signs of endometriosis, like tender spots or nodules.
- Blood Tests: There’s no single blood test for endometriosis, but your doctor might do some to check for other conditions or your overall health.
Getting a correct diagnosis is vital for managing endometriosis well. By working with your doctor and doing the needed tests, you’re on the right path to finding the right treatment for you.
Remember, endometriosis is complex, and diagnosing it can differ for everyone. Be patient, stand up for your health, and work with your healthcare team to find the best solution for you.
Treatment Options for Endometriosis-Related Ovulation Pain
If you’re dealing with endometriosis-related ovulation pain, there are several treatment options available. These include medications, hormonal therapies, and surgical interventions. A combination of these approaches may be necessary to find the right solution for your individual needs.
Medication and Hormonal Therapies
Over-the-counter pain relievers, such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs), can help with the pain. Hormonal therapies, like birth control pills, hormonal patches, or intrauterine devices, can also help. They regulate the menstrual cycle and reduce the growth of endometrial tissue, which can reduce pain.
Surgical Interventions
For more severe cases of endometriosis, surgical interventions may be recommended. Laparoscopic surgery can remove endometrial implants, scar tissue, and cysts. This can provide relief from endometriosis-related ovulation pain. In some cases, a hysterectomy (removal of the uterus) with or without the removal of the ovaries (oophorectomy) may be necessary for long-term management of symptoms.
It’s important to note that while surgery can be effective, there is a risk of recurrence. About 20 out of 100 women experience regrowth of endometrial implants within five years post-surgery. Hormone medications prescribed before and after laparoscopy may help prevent endometriosis from recurring.
The choice of treatment will depend on various factors. These include the severity of your symptoms, your desire to have children, and your overall health. It’s essential to work closely with your healthcare provider to develop a personalized treatment plan that addresses your specific needs.

Lifestyle Modifications for Managing Ovulation Pain
If you’re dealing with ovulation pain from endometriosis, making lifestyle changes can help. By tweaking your daily habits, you can ease the discomfort and boost your health.
Start by looking at your diet. Eating foods that fight inflammation can help. Choose whole, unprocessed foods. Also, drink plenty of water and cut down on alcohol and caffeine.
Regular exercise is also key. Yoga, Pilates, or a brisk walk can relax your muscles and improve blood flow. They also release endorphins, which can help with pain.
- Try stress-reducing activities like meditation, deep breathing, or guided imagery.
- Use heat therapy, like warm baths or heating pads, to relax your muscles.
- Consider trying chiropractic care, acupuncture, or supplements like vitamin B1, magnesium, or omega-3 fatty acids.
Everyone’s body is unique, so you might need to try different things to find what works for you. By mixing these strategies, you can manage your endometriosis-related ovulation pain and enhance your life quality.
Other Possible Causes of Pelvic Pain During Ovulation
Endometriosis is a common reason for severe pain during ovulation. But, other conditions can also cause pelvic pain. These include:
- Ovarian cysts: These are “functional cysts” that form as part of the menstrual cycle
- Pelvic inflammatory disease (PID): An infection of the reproductive organs, often from STIs
- Adenomyosis: When endometrial tissue grows into the uterine wall
- Ovarian tumors: Some growths on the ovaries can cause pain during ovulation
- Polycystic ovary syndrome (PCOS): A hormonal disorder with multiple small cysts on the ovaries
- Uterine fibroids: Noncancerous growths in the uterus
- Ectopic pregnancy: A dangerous condition where the fertilized egg implants outside the uterus
A 2013 study showed that 35 percent of women feel pain during ovulation. About 16.6 percent feel pain on one side. A 2014 review found that 5.7 to 26.6 percent of women worldwide have chronic pelvic pain. This pain can be caused by many things, not just causes of pelvic pain during ovulation.
| Condition | Prevalence | Characteristics |
|---|---|---|
| Menstrual cramps | Common | Intense or worsening pain requiring medical attention |
| Mittelschmerz | About 20% of women | Pain experienced during ovulation |
| Endometriosis-related ovulation pain | 5-10% of women | Severe pain requiring medical intervention |
| Ovulation pain | About 1 in 5 women | Mild to moderate pain experienced during ovulation |
If you have persistent or severe ovulation pain other causes, see a doctor. They can find the cause and help you get better.
When to Seek Medical Attention for Ovulation Pain
Ovulation pain, or mittelschmerz, is common among women. Mild pain during ovulation is usually okay. But, if the pain is severe or lasts a long time, it might mean there’s a bigger issue. Here are signs you should see a doctor for ovulation pain:
- The pain keeps you from your normal daily activities
- The pain lasts longer than 48 hours
- The pain gets worse or doesn’t go away with prescribed treatment
- The pain occurs along with vaginal bleeding (more than light spotting)
- The pain is sudden, sharp, and lasts for more than a few hours
- The pain occurs with other symptoms such as fever, nausea, or vomiting
Severe ovulation pain that lasts longer than 48 hours could be a sign of a more serious condition like endometriosis. It’s important to see a doctor to find out what’s causing the pain and get the right treatment.
If you’re experiencing any of these severe symptoms, don’t wait to call your healthcare provider. Getting medical help quickly can help find the cause and improve your health.
Distinguishing Normal Ovulation Pain from Endometriosis
Feeling a bit of discomfort or mild cramping during ovulation is normal. Up to 40% of women and individuals who menstruate experience ovulation pain, known as mittelschmerz. This pain is usually short, lasting up to an hour, and may happen a few days before or after the egg is released. But, if the pain is severe, lasts more than 48 hours, or gets in the way of your daily life, it might be a sign of endometriosis.
Some signs that your ovulation pain could be from endometriosis include:
- Intense, long-lasting pain (over 48 hours)
- Pain with sexual intercourse
- Painful urination or bowel movements
- Pain accompanied by vomiting or diarrhea
- Bleeding during ovulation (more than light spotting)
- Pushing, stabbing, tugging, or pulling pain that is not relieved with interventions
If you’re experiencing any of these symptoms, it’s vital to talk to your healthcare provider. They can figure out the cause and create a treatment plan to help manage your pain and discomfort.
The Impact of Endometriosis on Quality of Life
Endometriosis is a chronic condition that can greatly affect a person’s life. The severe pain during ovulation and menstruation can stop people from doing everyday things. This includes work, school, or social activities.
Endometriosis does more than just cause pain. It can also harm personal relationships and sexual life. The long-term nature of the condition and the hard time getting a correct diagnosis can lead to frustration, anxiety, and depression. These feelings can make a person’s overall well-being worse.
Studies show that about 10-15% of women of childbearing age have endometriosis. It often takes 5 to 10 years to get a diagnosis after symptoms start. Endometriosis can affect women from the start of their periods to after menopause, and sometimes even longer.
It’s important to tackle both the physical and emotional sides of endometriosis with a good treatment plan and support. Understanding the impact of endometriosis and how it affects quality of life helps healthcare providers and policymakers. They can then work on better ways to help those with this condition.
Coping Strategies for Ovulation Pain
Ovulation pain, or mittelschmerz, is common for those with endometriosis. It can be frustrating. But, there are ways to manage this discomfort.
Over-the-Counter Pain Relief
Using over-the-counter pain relievers is a good start. Acetaminophen or NSAIDs like ibuprofen or naproxen can help. They reduce inflammation and ease pain.
Topical pain relievers with ingredients like lidocaine or menthol can also help. They provide quick relief when applied to the pain area.
Complementary and Alternative Therapies
Some people find relief in alternative therapies. Chiropractic care, acupuncture, and supplements like vitamin B1 or omega-3 fatty acids may help. Always talk to your doctor before trying new treatments.
Everyone’s experience with endometriosis is different. Finding the right coping strategies may take time. Be patient, talk to your healthcare team, and explore different options for relief.

Understanding the Menstrual Cycle and Ovulation Process
Ovulation happens about 10-14 days after your period starts. A mature egg is released from an ovary and travels to the fallopian tube. There, it can be fertilized by a sperm. If not, you get your period.
Some people feel a bit of discomfort or notice they’re ovulating. But, if the pain is severe, it might mean you have endometriosis. Knowing about the menstrual cycle overview and ovulation process explanation helps you know when to see a doctor.
- In a 28-day cycle, ovulation is around day 14.
- An egg lives 12 to 24 hours after ovulation. Sperm can last several days.
- Ovulation can happen 14 days before your next period, no matter the cycle length.
- Ovulation kits can tell you when you’re ovulating within 36 hours.
- The best time to get pregnant is one to two days before ovulation and on ovulation day.
| Statistic | Value |
|---|---|
| Ovulation pain experienced by individuals | Up to 40 percent |
| Fertile window (days leading up to and including ovulation) | 6 days |
| Likelihood of pregnancy using fertility awareness methods in a year | 12 to 24 out of 100 people |
| Accuracy of fertility monitors in detecting fertile days | 99 percent |
Knowing when you ovulate is key for getting pregnant or avoiding it. It also helps keep your menstrual cycles regular. By learning about the ovulation process, you can take better care of your reproductive health. And you’ll know when to see a doctor for any symptoms.
Raising Awareness About Endometriosis and Ovulation Pain
Endometriosis is a common but misunderstood condition that can greatly affect your life. By spreading the word about the connection between endometriosis and severe ovulation pain, we can help more people understand the symptoms. This can lead to more research, better diagnostic tools, and more effective treatments.
Also, by educating the public and healthcare providers, we can reduce the stigma and isolation that people with endometriosis often face. It’s important to know that endometriosis affects at least 11% of women in the U.S., or over 6 ½ million women. It’s most common in women in their 30s and 40s.
Raising awareness is key to improving the lives of those with endometriosis. By sharing information about symptoms, risk factors, and treatments, we can help people advocate for their health. Together, we can make a big difference in the lives of those affected by this often-overlooked condition.
Source Links
- https://www.verywellhealth.com/endometriosis-ovulation-pain-7108951
- https://www.fertifa.com/post/endometriosis-pain-when-ovulating
- https://www.mayoclinic.org/diseases-conditions/mittelschmerz/symptoms-causes/syc-20375122
- https://helloclue.com/articles/cycle-a-z/ovulation-pain-101
- https://www.miracare.com/blog/endometriosis-and-ovulation-pain-why-does-it-happen/
- https://flo.health/menstrual-cycle/health/symptoms-and-diseases/endometriosis-ovulation-pain
- https://blog.inito.com/endometriosis-and-ovulation-pain/
- https://www.medicalnewstoday.com/articles/ovulation-cramps
- https://www.parents.com/getting-pregnant/ovulation/ovulation-pain-what-does-mittelschmerz-feel-like/
- https://ocrahope.org/news/5-possible-causes-for-ovary-pain/
- https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656
- https://www.who.int/news-room/fact-sheets/detail/endometriosis
- https://my.clevelandclinic.org/health/diseases/10857-endometriosis
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2880548/
- https://www.ncbi.nlm.nih.gov/books/NBK279498/
- https://www.thewomens.org.au/health-information/periods/endometriosis/treating-endometriosis
- https://www.healthline.com/health/pregnancy/ovulation-pain
- https://www.adorefertility.com/ovulation-fatigue-described/
- https://www.healthline.com/health/womens-health/ovarian-cyst-treatment-at-home
- https://www.medicalnewstoday.com/articles/323572
- https://www.webmd.com/women/mittelschmerz-pain
- https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=abn2771
- https://theluckyegg.com/2023/05/11/ovulation-pain-why-does-it-happen-and-when-should-you-be-concerned/
- https://www.uranj.com/blog/5-reasons-you-have-pain-during-ovulation-what-you-can-do
- https://flo.health/menstrual-cycle/health/ovulation/ovulation-pain
- https://drbrighten.com/is-pain-during-ovulation-normal/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7513434/
- https://academic.oup.com/humupd/article/19/6/625/839568
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10139092/
- https://www.ncbi.nlm.nih.gov/books/NBK549822/
- https://www.healthline.com/health/womens-health/ovulation-cramps
- https://my.clevelandclinic.org/health/articles/23439-ovulation
- https://www.healthline.com/health/womens-health/what-is-ovulation
- https://www.womenshealth.gov/a-z-topics/endometriosis
- https://www.uclahealth.org/medical-services/obgyn/conditions-treated/endometriosis
- https://www.linkedin.com/pulse/endometriosis-awareness-understanding-impact-fertility-9cvnc