Prevalence of Fibromyalgia
When it comes to the prevalence of fibromyalgia, how common is it really?
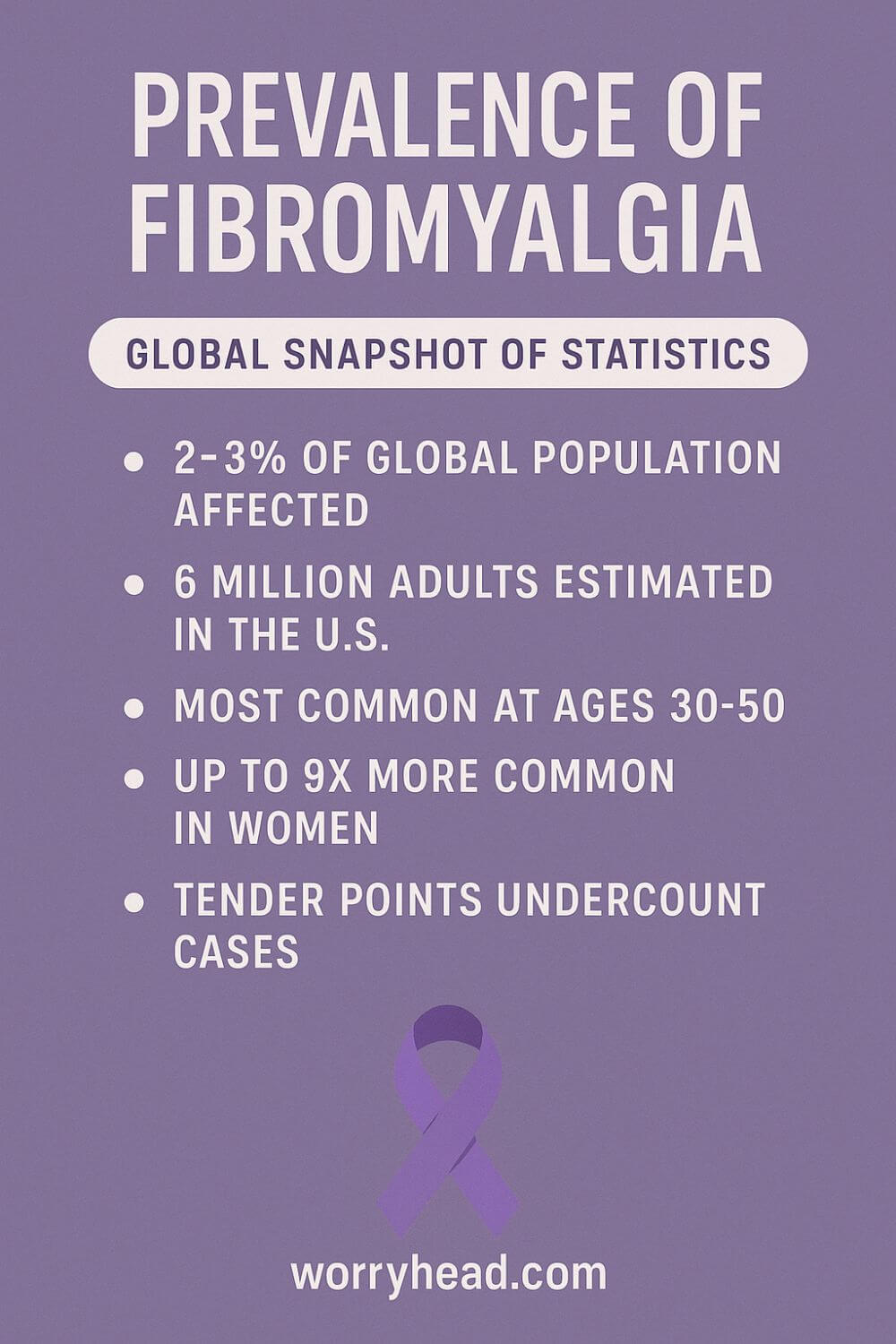
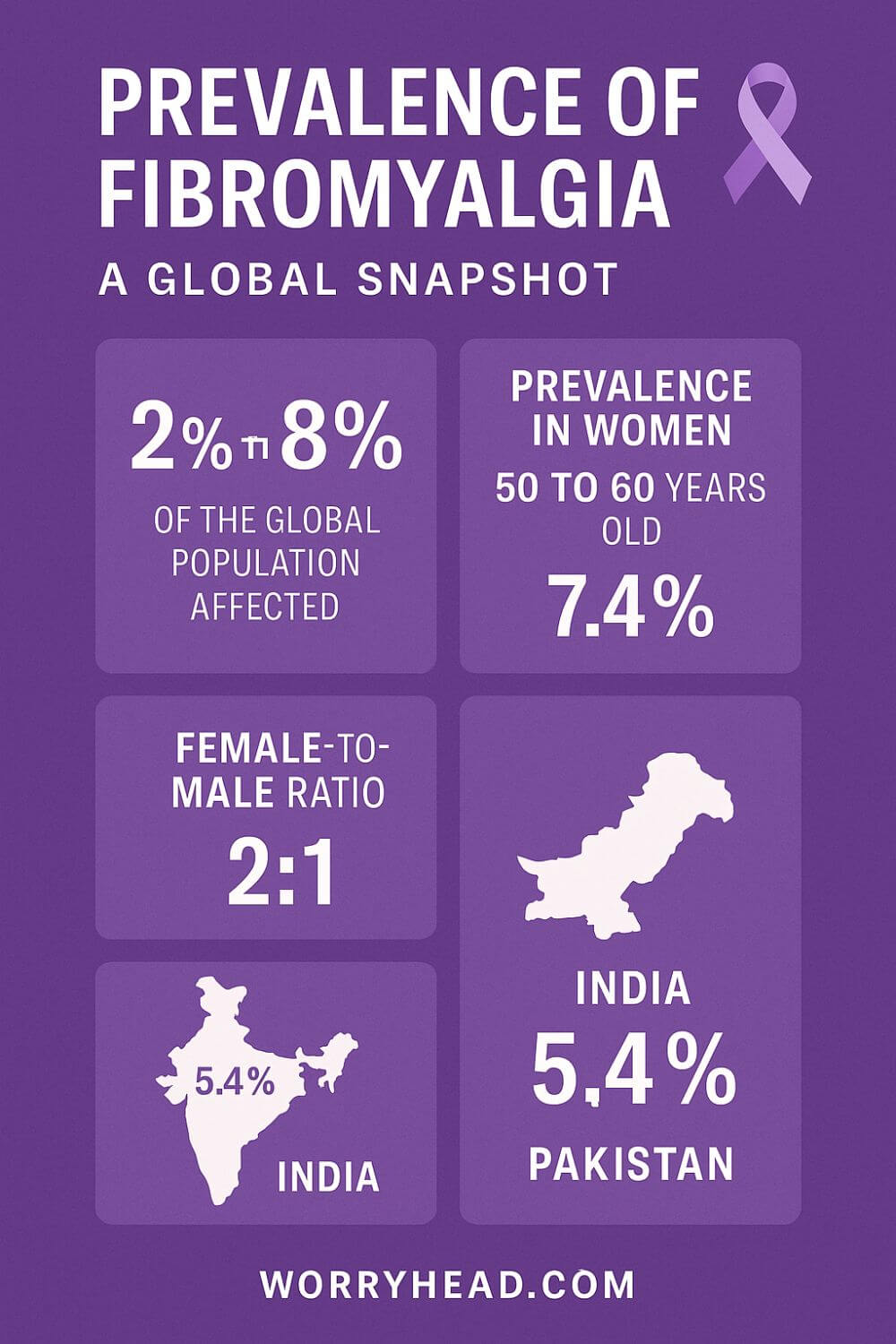
Fibromyalgia affects roughly 2–3% of people worldwide (≈2.7% on average). In the United States, it’s about 2% of adults, around 4 million people. Rates are higher in women, though men are likely underdiagnosed. Prevalence varies by region and evolving diagnostic criteria across studies and years.
Across countries, estimates span from well under 1% to nearly 9% depending on population and methods, with a commonly cited global mean near 2.7%. Newer criteria and “proxy” approaches tend to yield higher counts, and may capture people missed by older methods. That gap matters because service planning follows the numbers.
When my wife’s pain first took over our evenings, I learned how statistics can feel like a lifeline and a dismissal at the same time, proof you’re not alone, yet not nearly enough to unlock timely help. Behind every percentage is a household trying to stay gentle with each other in the dark.
If fibromyalgia is part of your life, you’re welcome in our community. You can grab 3 free chapters of my book “Fibromyalgia for Caring Partners” and, by joining, you’ll also receive more practical freebies, big discounts on our books, and emails designed to help couples adjust to the “new normal” with dignity and hope.
These 3 chapters alone explain how to accept the new normal, understand fibromyalgia, and its diagnosis. They include:
- The new you.
- The new her.
- The new reality.
- Introduction to fibromyalgia.
- What is fibromyalgia?
- The early days.
- When you first realize something is wrong.
- Spotting the signs that something is wrong.
- Coming to terms with a chronic illness.
- The role of a partner in fibromyalgia.
- The process of getting diagnosed.
Get Your 3 FREE Chapters!
Fibromyalgia for Caring Men
Prevalence of Fibromyalgia
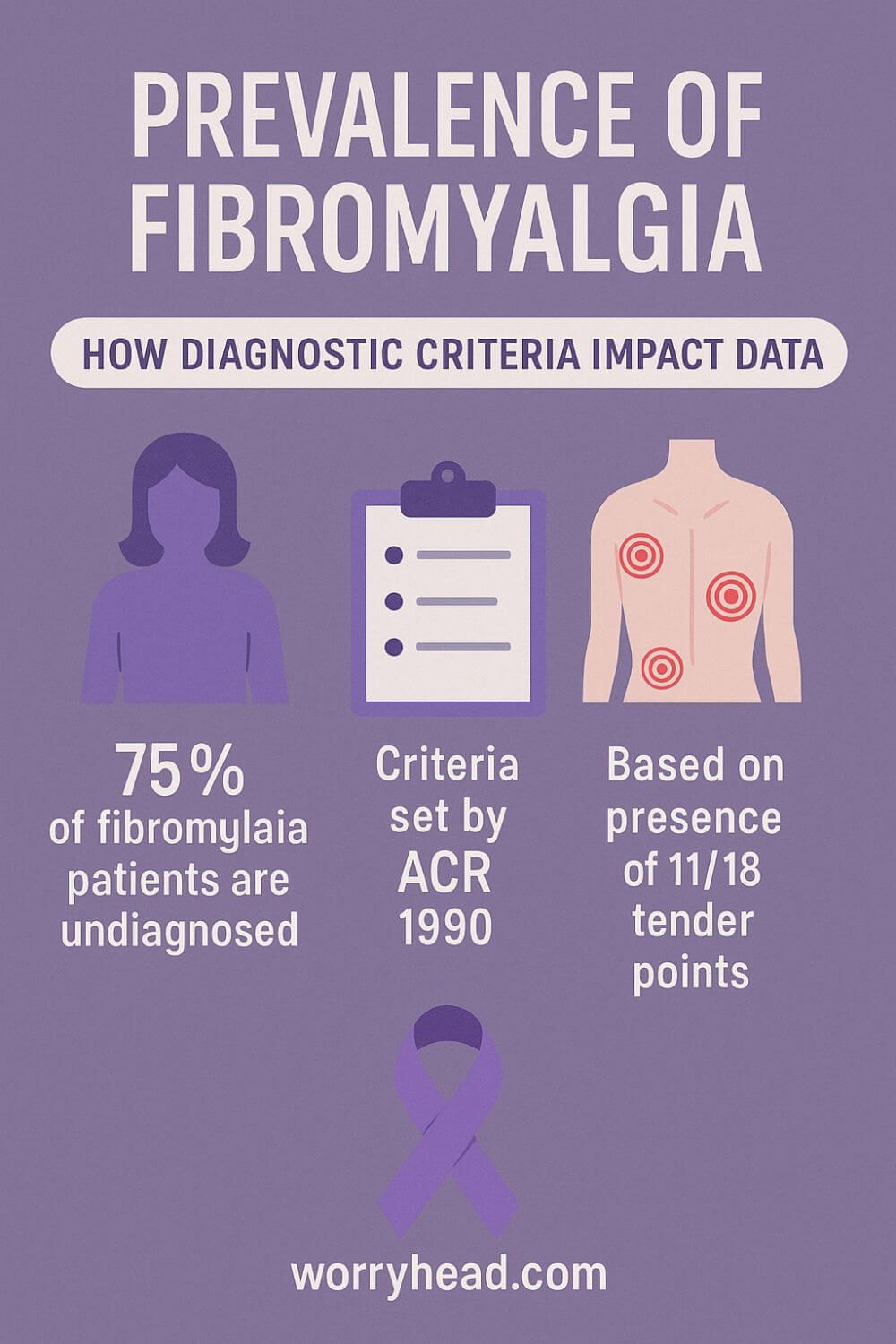
Prevalence estimates shift depending on methods and criteria, but the picture is consistent: fibromyalgia is common, frequently missed, and unevenly counted across countries and health systems.
Global reviews place the mean around 2.7%, with studies ranging from roughly 0.4% to 9.3% because of different sampling frames and diagnostic tools. That widespread isn’t noise, it’s a map of how we look, who we ask, and which yardstick we use.
In the United States, about 2% of adults, around 4 million people, are affected, a figure that anchors planning for clinics, rehab, and community support. Yet even that “steady” number flexes when newer criteria or self-report screens are adopted.
The UK often reports higher figures; a widely cited synthesis estimated 5.4% in the general population, reminding us that case-finding intensity and primary-care behavior shape who gets counted. When clinicians are primed to ask, more people surface.
Sex ratios are also being rewritten. In unbiased community samples using validated self-report criteria, women still predominate, but not by the historic 9:1. Some datasets show ≤60% female, evidence that men are underdiagnosed when identification leans on referral patterns or stereotypes.
Age patterns cluster in midlife, but pain-processing disorders don’t read calendars. What changes with age are labeling, comorbidity burden, and who has access to someone who can name their pain without dismissing it.
Across regions, the numbers move with criteria: the ACR 2010/2016 symptom-based approach and “proxy” methods tend to capture more cases than tender-point exams alone. Where health systems adopt modern criteria in primary care, recorded prevalence rises and waiting rooms suddenly look more honest.
Comorbidity clouds the count. Depression and anxiety are common fellow travelers, and their presence can either speed recognition or bury the signal under other diagnoses, depending on the clinician. Either way, the burden rises even when the incidence does not.
When my wife’s symptoms crescendoed, we learned how a statistic can be a doorway or a dead end. If your GP believes the prevalence is tiny, you get told you’re “unlikely.” If they’ve read the modern data, you get a plan and a little of your life back.
As you read on, here’s what helped us turn numbers into care you can feel. In the next section, I’ll break these into simple, practical steps you can start today:
- Ask which criteria your clinic uses
- Track the symptom severity scale weekly
- Bring a one-page history to appointments
- Screen gently for mood and sleep comorbidity
- Map flares to workload and recovery days
- Advocate for primary-care-led diagnosis
- Seek pacing + graded activity guidance
- Build a home routine for restorative sleep
- Join a peer group that shares tools
Ask Which Criteria Are Used
Before anything else, ask your GP or rheumatology clinic which diagnostic criteria they actually use. If they still rely on tender points alone, you may be undercounted from the start. The 2010 and 2016 symptom and impact criteria capture real-life pain, fatigue, and cognitive fog that tender points can miss.
When I learned to ask this out loud, doors opened. The conversation shifted from “unlikely” to “let’s measure.” Bring a calm, curious tone and write the question at the top of your notes so you won’t forget it when you’re tired.
If the answer is vague, request a symptom checklist and a follow-up plan. Clarity lowers anxiety. Clarity also creates a trail in your records that another clinician can follow if referrals take time.
Track Symptom Severity Weekly
A simple weekly tracker turns noise into signal. Use the symptom severity scale and a brief pain map, plus sleep quality, cognitive fog, and function notes. Keep it to five minutes on Sunday so it becomes a rhythm, not a burden.
Patterns emerge faster than you expect. You start to see how hormones, workload, or a poor night of sleep ripple into tomorrow’s pain. This helps you describe your life in clinical language without losing your humanity.
When my wife and I began tracking, we argued less with memory and more with evidence. That softened the room during appointments and moved care forward.
One-Page History For Visits
Clinics run on minutes. A clean one page history respects that reality and protects your story. List onset, key flare events, tried medications and responses, exercise tolerance, sleep issues, and the three outcomes that matter most to you.
Open with one sentence: what you want from today. Close with a short timeline. Hand it to the nurse and the clinician, and keep a copy for yourself.
That single sheet has saved us from the “start again, tell me from the beginning” spiral. It turns scattered details into a map a busy clinician can follow, which means better questions, fewer assumptions, and fewer tears on the drive home.
Screen Mood And Sleep Gently
Pain changes mood. Mood changes pain. Sleep threads through both. Ask for brief screens for anxiety, low mood, and sleep disturbance, not because labels define you but because treatment often unlocks function.
A ten-minute conversation about nightmares, early waking, or restless legs can be more useful than another blood draw. If stigma creeps in, anchor the talk in function. “When my sleep is steady, I can prepare meals and join family calls.”
We learned that tending to sleep and mood wasn’t admitting defeat. It was choosing less suffering while the broader plan took effect.
Map Flares To Workload
Flares are not random. Draw a two-column map: left side for workload, right side for recovery. Include chores, commutes, childcare, and the invisible labor you shoulder.
Then circle clusters where load outruns recovery. That is where pacing lives. This visual turns “I’m overwhelmed” into “Tuesday needs reshaping.” It also gives partners a clear role.
For us, moving errands and adding one true rest window after heavy days cut the worst spikes. Not heroics. Just honest logistics based on what the map revealed.
Primary-Care-Led Diagnosis
Waiting months for specialty clinics can freeze a life. Ask if your primary care team will lead the diagnosis using symptom-based criteria and clear differentials. Many will, if invited and supported with good documentation.
Offer your one-page history, weekly tracker, and questions. Request a stepwise plan with review dates. This makes progress possible while referrals move in the background.
When our GP stepped in rather than stepping back, we stopped losing seasons to uncertainty. Primary care can be the place where names and plans begin.
Pacing And Graded Activity
Pacing is not giving up. It is choosing where energy goes so you can keep what you love. Start with honest baselines for walking, housework, and screen time. Then layer tiny increases with real rest, not doomscroll pauses.
Graded activity should never ignore pain signals. It should partner with them. If you overshoot, shrink the step and try again next week.
My role was to protect the plan from life’s chaos. Groceries one day, laundry the next. The goal wasn’t athletic glory. It was steadier weeks and fewer collapses.
Restorative Sleep Routine
Restorative sleep begins long before lights out. Guard a wind-down hour: warm shower, low light, no heated debates, consistent bedtime. Keep the room cool and dark. Write tomorrow’s tasks so they stop shouting in your head.
If pain wakes you, plan gentle options in advance: a brief stretch, a heat pack, a sip of water, then back to bed without screens. Consistency matters more than perfection.
When we treated sleep as a shared project, mornings hurt less. We didn’t fix everything. We made enough room for healing to start.
Join A Practical Peer Group
A good peer group gives you shortcuts you won’t hear in a seven-minute visit. Look for communities that swap tools, not just sympathy, and that welcome partners who want to help well.
Bring your maps and trackers. Ask what has worked for others with similar work patterns or hormone cycles. Offer one thing that helped you this month.
Belonging doesn’t erase pain. It erases the loneliness that makes pain louder. For us, that changed the texture of the whole week.
Lived Realities Behind the Prevalence of Fibromyalgia
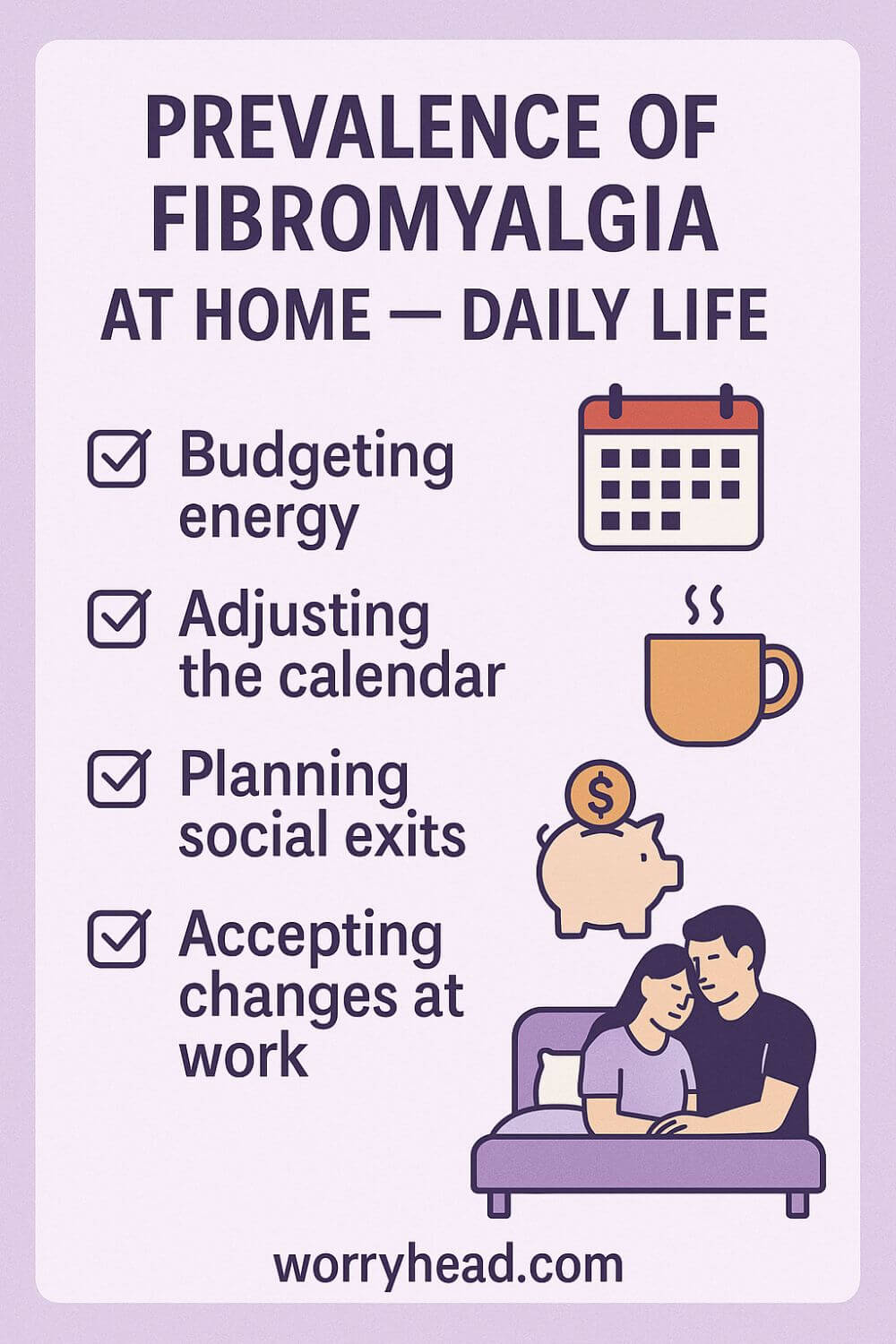
Numbers tell us who might be affected, but daily life reveals how. After diagnosis, families renegotiate chores, calendars, and careers so that pain does not swallow the week. That shift is invisible in any registry, yet it decides whether a home breathes.
Workplaces often mistake perseverance for wellness. Colleagues see a smile and assume recovery, not a cost paid later on the sofa. Without flexible hours and pacing, small victories at noon become crashes at night.
Healthcare moves in appointments, but symptoms move in waves. When access is slow, people learn to self-manage in the margins with sleep routines, food that steadies energy, and gentle movement that does not trigger a flare. Good clinicians join that rhythm instead of fighting it.
Money matters more than most paperwork captures. Missed shifts, extra taxis, co-pays, and trial-and-error therapies nibble at savings. The pressure to “prove” illness in order to keep support in place adds a second weight on already tired shoulders.
Relationships can deepen or fracture. Honest maps of energy and pain protect tenderness. Partners who learn to listen for early signs can reroute a day before it breaks, which often feels like love in its most practical form.
At home, I became the guardrail around her afternoons. I moved errands to quieter days, learned to read the flicker in her eyes, and held my plans loosely so she could hold onto hers. Grief visited, but so did a steadier kind of joy.
There are days when she cannot lift her head, and I make tea, close the curtains, and sit in the quiet so she does not blame herself for needing care. There are days when she laughs, and we walk a little farther than last week. Both are real. Both belong.
The bravest thing I have watched her do is ask for smaller goals without apology. Ten minutes of movement. One friend called instead of three messages. Choosing gentleness over the old habit of pushing through.
What changes everything is being believed. In clinics, at work, at home. When people are believed, they pace before a crash, accept help without shame, and save energy for moments that matter.
If you are reading this in the middle of your own storm, know that your ordinary day counts as progress. You are not late. You are learning a new way to live, and that learning is work.
What does the Prevalence of Fibromyalgia Mean at Home?
The numbers shape policy, but they also shape kitchens, calendars, and the way a couple whispers goodnight. When a condition is common, it hides in plain sight and still feels isolating until someone names it with care.
We learned to budget energy like money. Groceries moved to quieter hours. Social plans came with an exit plan so a good day did not cost the whole week.
I track chores like a coach, not a supervisor. She leads what she can, I catch what falls, and we both practice leaving a little undone so tomorrow is possible.
Work changed from proving resilience to protecting function. Flexible starts, honest check-ins, and a chair that does not punish the body became part of our livelihood, not extras.
Clinics helped most when they accepted the rhythm of flares and remissions. Shorter waits, clear follow-ups, and practical sleep guidance did more for us than another test that could not feel the pain.
Here is where the prevalence of fibromyalgia becomes personal. If many live with it, then systems can be designed around it, and couples like us can stop feeling like exceptions that need to beg for accommodations.
On hard mornings, I make tea, dim the room, and keep the house quiet so she does not spend energy apologizing. On brighter afternoons, we walk to the park and count that as a win without comparing it to anyone else’s pace.
We learned to ask specific favors from friends. A lift to an appointment. Fifteen minutes of company. People show up better when the ask is small and real.
Hope arrived as routine, not miracles. Ten minutes of movement. A consistent bedtime. One warm meal that does not spike symptoms. Small things add up when you give them time.
And love looks like logistics. It is the calendar I adjust, the patience she offers, and the way we both choose gentleness over the old habit of pushing through.
Conclusion on the Prevalence of Fibromyalgia
Numbers never hold the whole story, but they help us see patterns we can plan around.
When I first tried to make sense of my wife’s symptoms, I clung to data like a railing in a dark stairwell. Statistics do not lessen pain, yet they give language to ask for help, to argue for adjustments at work, and to build care that fits a real day. That is what the science ultimately gives us, a shared map for conversations that change lives.
What the global literature shows, across methods and borders, is a common condition that is often unseen until someone knows the right questions to ask.
Diagnostic criteria matter; tender points alone miss people who live with fatigue that crushes mornings, sleep that refuses to repair, and cognition that blurs just when life demands clarity. More modern, symptom-based tools catch those realities and make the invisible legible to systems that need lines and boxes to move.
Prevalence estimates vary by country and clinic, but the lived implications are steady: families renegotiate calendars; employers either become partners in pacing or barriers to recovery; and primary care can, with confidence, make the first call rather than leaving a household in limbo for months.
The lesson underneath the numbers is simple: belief, access, and a practical plan are what change on Tuesday afternoon, not debates about labels that never lead to action.
At home, we learned to budget energy like money and to trade perfection for consistency. Ten minutes of movement most days. A wind-down hour we protect. Meals that stabilize rather than spike. These are not heroic acts; they are routines that, repeated, carve out room for better weeks.
My role is logistics and softness, moving errands, spotting a flare early, holding my schedule loosely so she can hold onto hers. These ordinary choices, multiplied by time, are where hope grows.
So if you are reading this while trying to square the numbers with your reality, take this with you: the data exist to unlock care, not to measure your worth or decide whether you “qualify” to be taken seriously. Bring a one-page history. Track your symptoms. Ask which criteria your clinician uses. Invite your partner into the rhythm of pacing and recovery. And remember that a steady life is built from small, repeatable acts that protect what matters most to you.
The statistics point to a wide community. The work ahead is making that community visible enough that care pathways, workplaces, and homes are designed with it in mind. That is how we turn evidence into easier mornings and kinder weeks, one plan, one conversation, one household at a time.
A shared map of the condition helps us argue for access, shape kinder workplaces, and build home routines that make room for steadier weeks and gentler days, proof that informed care, patient pacing, and partner support can turn hard numbers into real relief.
I’d love to hear your story. Leave a comment below. If this resonates, you can also grab 3 free chapters of my book “Fibromyalgia for Caring Partners.” By joining, you’ll receive practical freebies, big discounts on all our books, and honest emails that help couples adjust to the new normal together.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MOREPrevalence of Fibromyalgia FAQs
1) What is the current prevalence of fibromyalgia worldwide?
Most systematic reviews place the prevalence of fibromyalgia around 2–3% of the global population. Differences in study design, criteria used, and who gets surveyed explain why some papers report lower or higher figures.
2) Why do published estimates of the prevalence of fibromyalgia vary so much?
Estimates shift with methodology: tender-point exams tend to undercount; symptom-based criteria (2010/2016) capture more real-world cases. Sampling (clinic vs. community), age ranges, and response rates also move the numbers.
3) How does the prevalence of fibromyalgia differ by sex and age?
Women are diagnosed more often, but newer community data suggest the gap is smaller than older 9:1 assumptions—partly because men are historically underdiagnosed. Prevalence clusters in midlife yet occurs across adult ages.
4) What do regional studies say about the prevalence of fibromyalgia?
United States estimates hover near 2% of adults. Some UK and European datasets report higher figures, while rates across Canada, Australia, India, Pakistan and other regions vary with diagnostic uptake and primary-care recognition.
5) Is the prevalence of fibromyalgia increasing over time?
Recorded prevalence often rises when health systems adopt modern criteria, improve primary-care identification, or run better community screens. That doesn’t always mean more people are developing fibromyalgia—often, we’re finally counting who was missed.
Prevalence of Fibromyalgia References
https://www.cdc.gov/chronic-disease/fibromyalgia/index.html
https://www.niams.nih.gov/health-topics/fibromyalgia
https://www.ncbi.nlm.nih.gov/books/NBK540974/
https://pubmed.ncbi.nlm.nih.gov/28743363/
https://www.scielo.br/j/rbr/a/cTj6DDGF8gGhMHHNksTMYjR/?lang=en
https://pmc.ncbi.nlm.nih.gov/articles/PMC4575027/
https://pmc.ncbi.nlm.nih.gov/articles/PMC4932255/
https://onlinelibrary.wiley.com/doi/10.1111/1756-185X.15428