Research & Future of Endometriosis
Research & future of endometriosis — where is it truly heading?
Rigorous research shows endometriosis is a systemic, chronic disease; near-term progress centres on earlier, imaging-based diagnosis, hormone-modulating therapies (including new NHS-approved options), and targeted trials like DCA, while major funding gaps still slow truly curative breakthroughs.
Behind the headlines, two forces reshape care: better imaging in expert hands and smarter, targeted medicines. Experienced sonographers can now map deep disease that once required diagnostic surgery. Meanwhile, trials explore metabolic and cannabinoid pathways, and surgical innovation (from precision robotics to nerve-sparing techniques) aims to reduce harm and recurrence. Together, these trends push us toward earlier detection, personalised therapy, and fewer lost decades.
My wife’s story is why I obsess over the evidence. When pain steals days, you stop caring about hype and start chasing what is proven to help: faster diagnosis, compassionate care, and treatments that let love and work reclaim space in your home.
If endometriosis is part of your life, you can grab a free chapter of my “Endo-Tool: Endometriosis for Men.” By joining, you’ll also enter our community where I share more freebies, meaningful discounts on all our books, and honest emails that help couples adjust to the “new normal” with strength and hope.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis, and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men


The Research & Future of Endometriosis
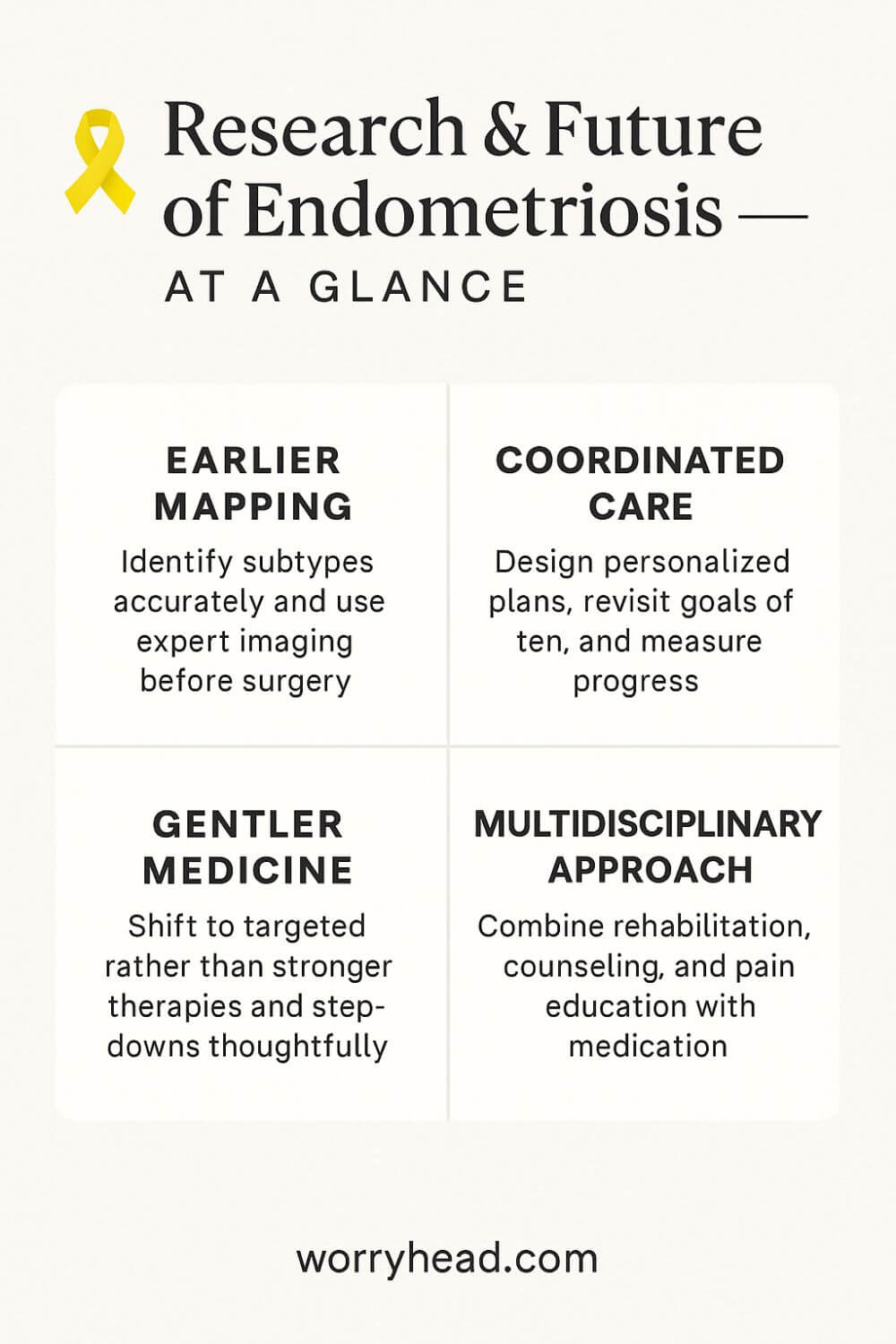
Progress is finally becoming practical. We’re seeing earlier recognition of red-flag symptoms, better non-invasive mapping of deep disease, and a calmer, kinder approach to pain that treats a whole person, not just a pelvis. Clinicians are comparing outcomes by subtype, so treatment plans don’t feel like guesswork.
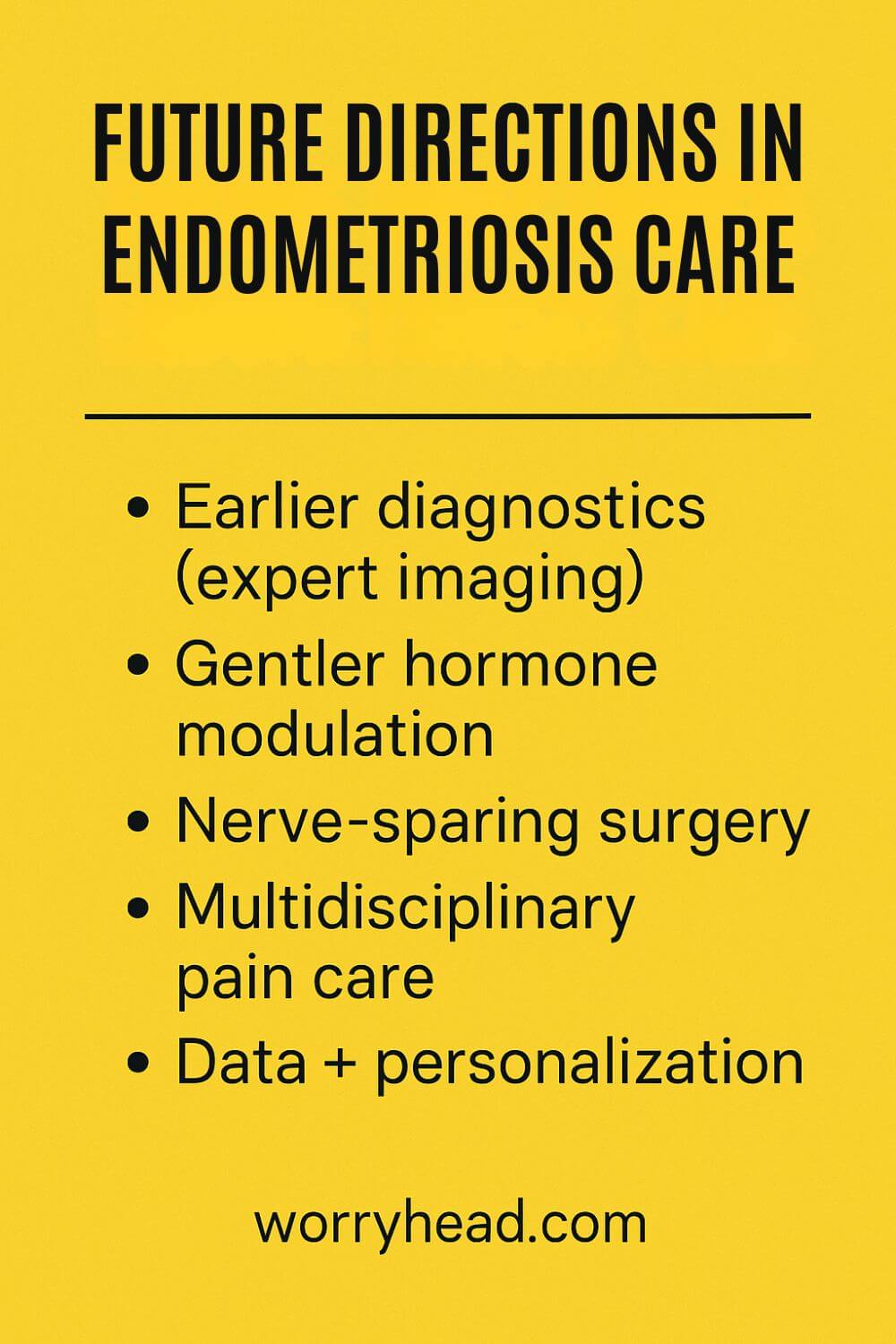
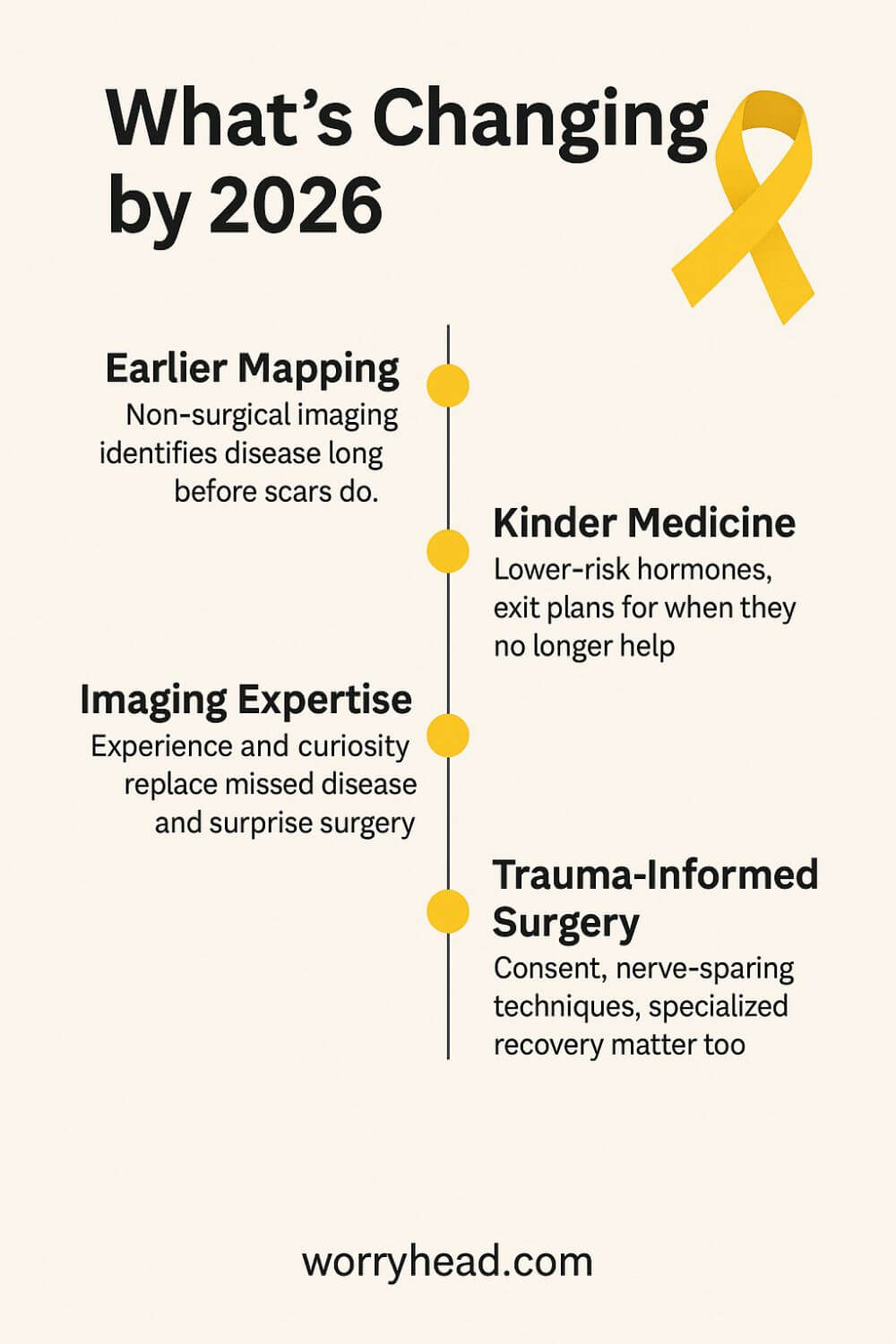
Specialist imaging is stepping up where diagnostic surgery once stood alone. Skilled sonographers can identify bowel, uterosacral, and diaphragmatic involvement with detail that actually changes the plan, not just the report. That spares patients from years of limbo and fast-tracks them to the right hands.
Medical therapy is getting smarter rather than simply stronger. Instead of swinging a hammer at hormones, research is moving toward tailored modulation, paying attention to side-effect burden, bone health, and mental well-being. For many, success looks like fewer flares, steadier energy, and space to live.
Surgery still matters, but the aim is precision and preservation. Teams are learning to operate with a narrower footprint: nerve-sparing techniques, meticulous excision, and realistic conversations about recurrence. Quality of life, fertility goals, and trauma-informed care sit at the center of decisions.
Scientists are also looking beyond the lesions to the biology that drives them. Immune signaling, neuroinflammation, and pain processing are no longer afterthoughts. This opens doors to therapies that calm the system, not just prune the tissue, and to rehabilitation that rebuilds capacity, not just tolerance.
Personalised pathways are becoming the north star. The same diagnosis can carry different genetics, different pain wiring, and different futures. That means tracking what actually works for an individual and adjusting quickly, rather than waiting years to confirm a hunch. Data is only useful if it shortens suffering.
Lifestyle isn’t a cure, but it is leverage. Thoughtful changes to movement, sleep, stress, and nutrition can soften the edges, especially when paced and sustainable. The point isn’t perfection; it’s building a body and life that are less combustible so medical gains can stick.
Most importantly, care is finally widening its circle. Partners, employers, and schools are being invited into the plan because accommodation is treatment when it protects energy, income, and dignity. Healing accelerates when a life has room for it.
I write this with my wife in mind, remembering nights we measured time in breaths and mornings we celebrated simply being upright. We learned that hope is not optimism; it is a plan that fits a person you love. If you’re ready for practical steps, the next section offers a handful we lean on when days get rough:
- Track patterns to personalise care
- Seek expert imaging before big decisions
- Ask for trauma-informed, nerve-sparing surgery
- Co-create a medication plan with exit ramps
- Build a gentle movement and pain-education routine
- Protect sleep with non-negotiable boundaries
- Design work and home around flare-friendly pacing
- Involve your partner and one trusted clinician
- Review what’s working every 8–12 weeks
Track Patterns to Personalise Care
Start with a simple system you can keep on hard days, for instance: a one-line daily log of pain location, intensity, bleed pattern, bowel/bladder changes, mood, sleep, and what helped. Keep it honest, not perfect. Trends beat anecdotes because they survive memory and bias.
After 2–3 weeks, translate the log into patterns: cycle-linked pain vs. constant, food triggers vs. stress triggers, movement that soothes vs. movement that spikes. Bring this to appointments as a single-page summary. It turns a vague story into actionable data.
Use it to test mini-experiments—one change at a time, for two weeks, with a planned review. That’s how you swap uncertainty for clarity and build a plan that fits the person you love, not the average in a study.
Get Expert Imaging First
When surgery or major medication is on the table, push for mapping by someone who does this all day, an expert transvaginal ultrasound or MRI read by a specialist. The goal isn’t just pictures; it’s a surgical roadmap that prevents surprises mid-procedure.
Ask specific questions:
- Can you see the uterosacral ligaments, bowel, bladder, and diaphragm?
- What’s likely superficial vs. deep disease?
- What else could explain these symptoms?
A good imager welcomes that curiosity and translates findings into plain language. Great imaging shortens the path to the right team, avoids repeat procedures, and sets expectations you can actually plan your life around.
Ask for Nerve-Sparing Surgery
If surgery is indicated, look for a specialist surgeon who will prioritise function, not just clearance. Nerve-sparing techniques, multidisciplinary planning, and consent that names risks you care about, sexual function, bowel/bladder outcomes, recurrence, are signs you’re in safe hands.
Bring your goals to the table: pain relief, fertility, athletics, and work demands. Ask how each step of the proposed operation protects those goals. High-quality surgeons talk in probabilities and options, not guarantees.
Insist on trauma-informed care from consult to recovery. Soft landings, warmth, choice, and clear explanations reduce postoperative stress and can improve how the nervous system remembers the experience.
Co-Create Medication Exit Ramps
Medications are tools, not identities. Build a shared plan that includes start criteria, dose ceilings, side-effect watch-outs, and exit ramps. Knowing how you’ll step down is as calming as knowing how you’ll step up during flares.
Track benefit vs. burden every few weeks using the same one-page summary. If sleep tanks or mood frays, pivot early rather than gritting teeth for months. Your body is giving you information; answer it.
Pair pharmacology with skills, heat, pacing, relaxation, pelvic physio, so relief doesn’t depend on a single lever. That redundancy is what resilience feels like.

Gentle Movement, Pain Education
When pain teaches avoidance, the body gets smaller. Reverse that carefully. Start with breath-led mobility and short, regular walks, then sprinkle in strength with long rests. The win is consistency, not heroics.
Layer in pain-science education: how sensitive nerves amplify normal signals, why graded exposure lowers alarms, why crash-and-burn cycles keep them high. Understanding changes fear, and fear is half the load.
Celebrate capacity, not numbers. If ten minutes today means twelve next month, that’s a life expanding again.
Guard Sleep with Boundaries
Sleep is a treatment. Create a pre-bed ritual you could follow in a hotel: dim lights, warm shower, screens down, same wake time. Protect it like a medicine schedule.
If pain barges in at night, prepare for it in daylight: heat pad by the bed, gentle stretches you can do under the covers, a script of calming thoughts you’ve practised when you weren’t exhausted. Small wins compound.
Ask others to honour the plan. The world can wait; healing can’t.
Design Flare-Friendly Work at Home
Make rooms serve energy, not aesthetics alone. A supportive chair, adjustable desk, task lighting, and heat/cold within reach change hours, not just vibes. Put frequently used items within a single slow walk.
At work, negotiate rhythm: flexible start times, remote days around cycle peaks, outcome-based goals. Stability is productivity when symptoms swing.
Create “low-power modes” for chores, batch cooking, deliveries, shared lists, so life doesn’t collapse when a flare hits.
Involve Partner and One Clinician
Choose one clinician to anchor the plan and one partner to help carry it. Too many voices breed confusion; two aligned voices build momentum. Share summaries, not raw emotion, in appointments so you’re heard clearly.
At home, agree on signals and scripts for tough moments. A word that means “I need quiet” can prevent a spiral. A planned hug can turn an argument back into a team.
You’re not codependent; you’re coordinated. That’s how families do hard things.
Review Progress Every 8–12 Weeks
Put reviews on the calendar like any other commitment:
- What improved?
- What stalled?
- What side effects crossed your line?
Keep what works, retire what doesn’t, and choose one new experiment.
This cadence stops drift and prevents “good enough” from becoming the ceiling. Progress in chronic illness is a staircase, not an escalator; reviews are the handrail.
When the plan respects reality, hope stops feeling like guesswork and starts feeling like craftsmanship.
More on the Research & Future of Endometriosis
Progress will hinge on how quickly we turn pattern-spotting into practice. The more precisely we describe subtypes, the less we rely on trial-and-error and the more we protect bodies from avoidable harm.
Data will help, but only if it shortens the distance between symptoms and certainty. When clinical notes, imaging, and lived experience speak the same language, treatment stops feeling like roulette and starts feeling like a plan.
Diagnostics will keep moving earlier. Instead of proving disease in an operating theatre, we’ll map it first, decide deliberately, and reserve scalpels for when they serve clear goals, pain relief, fertility, function, not vague hope.
Therapies will grow gentler and smarter. Rather than “stronger hormones,” we’ll see right-sized modulation, combination strategies, and careful step-downs that respect bone health, mood, and the nervous system’s tendency to guard.
Pain care will become multidisciplinary by default. Pelvic physio, pacing, trauma-informed counselling, and education about sensitised nerves will sit beside medicine and surgery, not beneath them, because capacity, not just pain scores, decides how a life feels.
And the science will widen its lens. Immune signalling, metabolism, and neuroinflammation aren’t side quests; they’re the map that explains why two similar scans can produce two very different Tuesdays.
For us, this isn’t abstract. I’ve watched my wife brace against mornings that should have been ordinary, and I’ve learned that love is logistics, appointments prepared, choices explained, rooms adjusted so her body has a softer place to land. The future I want is one where fewer couples become experts out of desperation and more become experts by design.
Your Care in Real Life
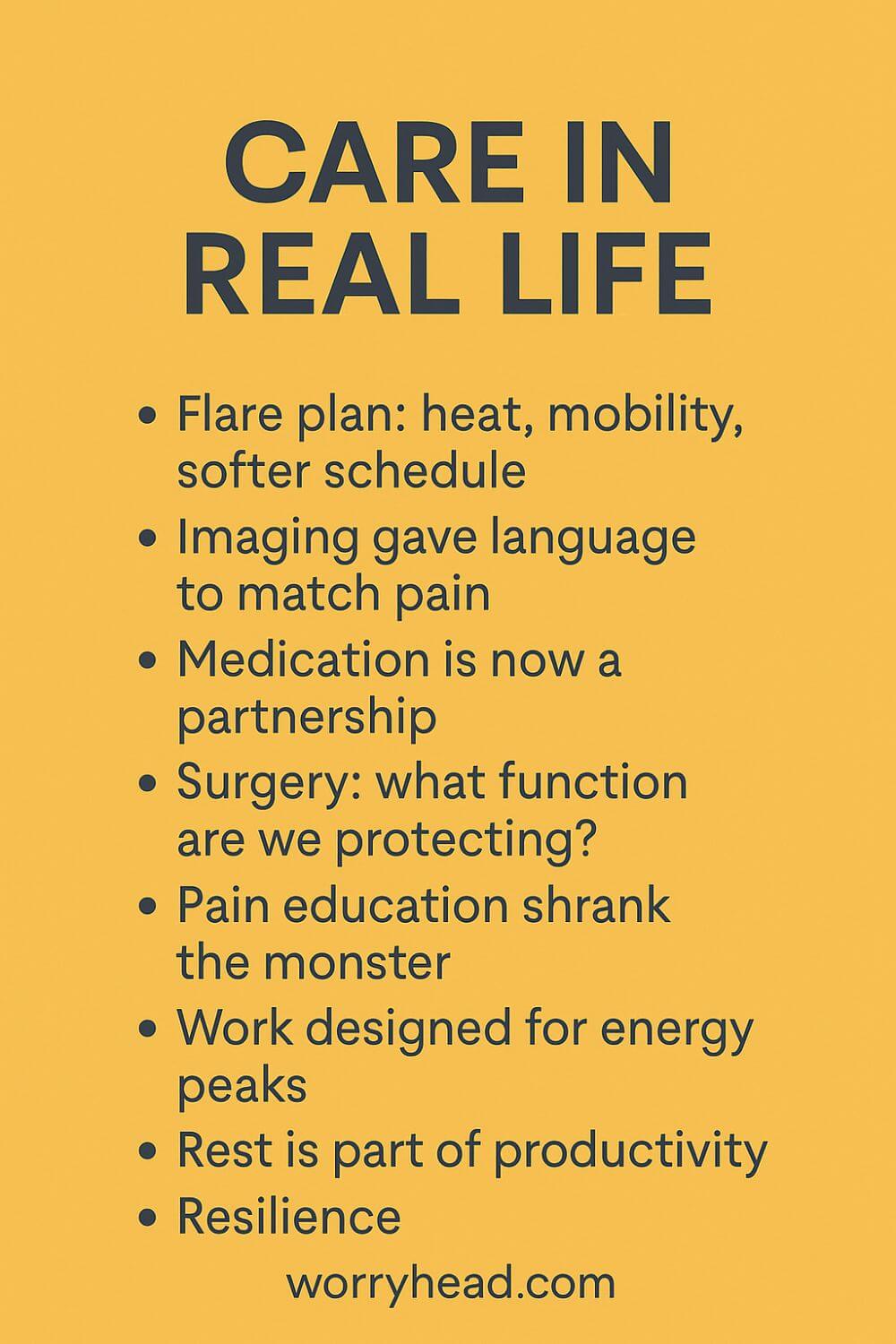
We learned that progress isn’t only a journal headline; it is a morning that hurts less and an evening that still has room for laughter. On our best weeks, small adjustments stack up into a day that feels like ours again.
When a flare threatens, we use the map we’ve built: early heat, gentle mobility, a softer schedule, meals that don’t pour petrol on the fire. Those choices are unglamorous, but they keep the floor from falling away.
Specialist imaging gave us language that finally matched her pain, and with that language came better decisions. Knowing which structures are involved helps me plan the house, meals, and travel so her body doesn’t pay interest on every errand.
Medication is a partnership now, not a battle. We set start rules and exit ramps together with the clinician, and I keep notes so we can pivot before side effects steal the wins.
Surgery taught us to ask different questions:
- What function are we protecting?
- Who will be in the room?
- How will recovery feel at home?
That mindset made us less afraid and more precise.
Pain education shrank the monster by naming it. When she understands why a nervous system can stay loud, she blames herself less, and I stop making rescues that accidentally feed fear.
Work also changed. We designed her days around energy peaks, built a desk that forgives long hours, and agreed that rest is part of productivity, not the price of it.
Some nights are still hard. On those nights, my job is to make the room kinder, keep stories light, and hold the line that tomorrow deserves another try.
Together, we measure success in capacities: a walk that used to be impossible, a meal shared without bracing, a plan made without a backup plan for pain. That is what the research & future of endometriosis looks like when it lands in a living room.
Conclusion on the Research & Future of Endometriosis
If I have learned anything from the quiet hours beside my wife’s bed, it is that progress is not an abstract promise. It is the difference between bracing through another morning and getting one back.
The science is moving, and it is moving in ways that matter: earlier recognition, expert imaging that informs real decisions, medications chosen for the person not the average, and surgery that protects function as much as it removes disease. None of this is flashy.
All of it is life.
What gives me hope is the shift from single answers to coordinated plans. When clinicians listen to patterns, when imaging is done by people who do it every day, when surgeons talk about nerves and recovery just as clearly as margins, the room changes.
You feel it.
Fear steps back because you can see the path. For us, the most important gains came from combining careful diagnostics with honest goals we revisited often. We kept what worked, retired what didn’t, and refused to accept that suffering was the price of being believed.
I also believe the next wave will come from looking beyond lesions. Pain lives in tissues, but it is shaped by the immune system, the nervous system, and the stress of surviving years without an answer.
That is why gentle strength training, pelvic physiotherapy, pain education, sleep boundaries, and unglamorous pacing now sit beside prescriptions in our house. None of those are cures. Together, they are momentum, and momentum is how couples climb.
There is a hard truth here. Some days remain heavy. Treatments carry trade-offs. Health systems are uneven, and waiting lists do not care about your courage. But there is another truth that kept us going. When you assemble a team that treats a person rather than a diagnosis, progress compounds. The days do not just hurt less. They start to belong to you again.
If you are standing where we once stood, I want you to hear this. You are not behind. You are not failing. You need a plan that fits your body and your life, built with people who will keep adjusting it with you. The research is catching up to what patients have known for years: dignity and data go further together than either goes alone.
That is the horizon I can see from our kitchen table, where love and logistics meet, and tomorrow keeps finding a way in.
A future worth fighting for is not one without pain. It is one with choices, capacity, and days that make sense again. That is enough to begin.
A life with endometriosis can become steadier when earlier mapping, kinder medicine, trauma-informed surgery, and practical habits work together. Progress is not linear, but momentum is real. Build a plan you can live with, review it often, and protect hope with evidence and teamwork.
I’d love to hear your story in the comments. If you want practical help, you can also grab a free chapter of my book for partners; it comes with our community, more freebies, and meaningful discounts that support your journey.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MOREResearch & Future of Endometriosis FAQs
1) Will there be a cure for endometriosis?
A true cure isn’t here yet. The field is moving toward earlier diagnosis, targeted medicines, and gentler, nerve-sparing surgery. For now, most people do best with a personalised combination: expert imaging, thoughtful medication, skilled surgery when needed, and rehabilitation that protects capacity.
2) Are sonographers really becoming the “gold standard” for diagnosis?
Skilled pelvic sonographers can map deep disease (e.g., bowel, uterosacral, bladder) with impressive accuracy, often replacing the need for diagnostic surgery. It’s operator-dependent, though—results are best in experienced hands and should guide, not replace, clinical judgement.
3) What new treatments are researchers exploring?
Beyond hormone modulation, trials are probing immune, metabolic, and neuroinflammatory pathways. You’ll see studies on selective progesterone strategies, pain-neuroscience-informed rehab, and metabolic approaches like dichloroacetate in select settings. Most are early-stage; benefits and risks must be weighed with a specialist.
4) How do I know if surgery is the right next step?
Use expert imaging first to define goals (pain relief, fertility, function). Seek a surgeon who discusses nerve-sparing techniques, complication risks, and recovery. Good plans include non-surgical supports (pelvic physio, pacing, sleep, pain education) so progress doesn’t rely on one intervention.
5) What can I do while waiting for appointments or trials?
Track symptoms in a simple daily log, protect sleep, introduce graded movement, and identify work/home adjustments that conserve energy. Bring a one-page summary to visits. These steps don’t cure endometriosis, but they make medical care more effective—and they gave my wife back pieces of her day.
Research & Future of Endometriosis References
https://www.nice.org.uk/news/articles/nice-updated-guideline-to-improve-the-diagnosis-of-endometriosis
https://www.nice.org.uk/guidance/ng73/resources/visual-summary-on-first-presentation-initial-management-diagnosis-referral-and-ongoing-care-of-pdf-13559822461
https://www.ncbi.nlm.nih.gov/books/NBK604070/
https://pmc.ncbi.nlm.nih.gov/articles/PMC8951218/
https://onlinelibrary.wiley.com/doi/10.1002/sono.12402
https://www.researchgate.net/publication/383660530_Are_sonographers_the_future_%27gold_standard%27_in_the_diagnosis_of_endometriosis
https://www.clinicaltrials.gov/study/NCT04046081
https://reproductive-health.ed.ac.uk/news/2024-news/endometriosis-action-month-2024
https://pubmed.ncbi.nlm.nih.gov/40704733/
https://www.ucsf.edu/news/2025/07/430471/big-data-begins-crack-case-endometriosis
https://www.contemporaryobgyn.net/view/new-research-aims-to-transform-endometriosis-diagnosis
https://www.theguardian.com/society/2025/mar/13/first-of-a-kind-daily-pill-for-endometriosis-treatment-approved-for-nhs-in-england
https://www.thetimes.co.uk/article/endometriosis-drug-ryeqo-nhs-pill-ztc3frqqj
https://www.sciencedirect.com/science/article/pii/S1472648325000379