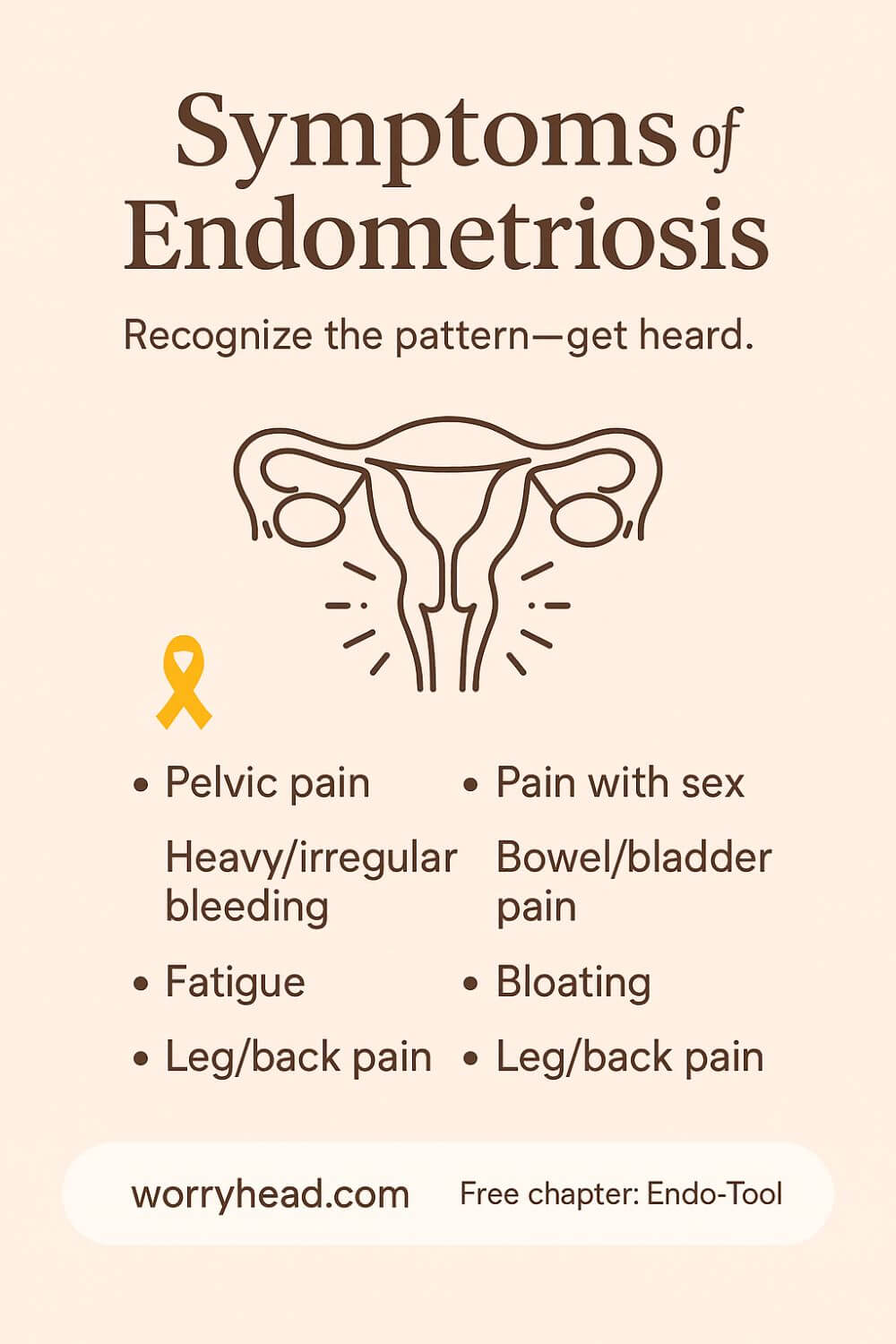
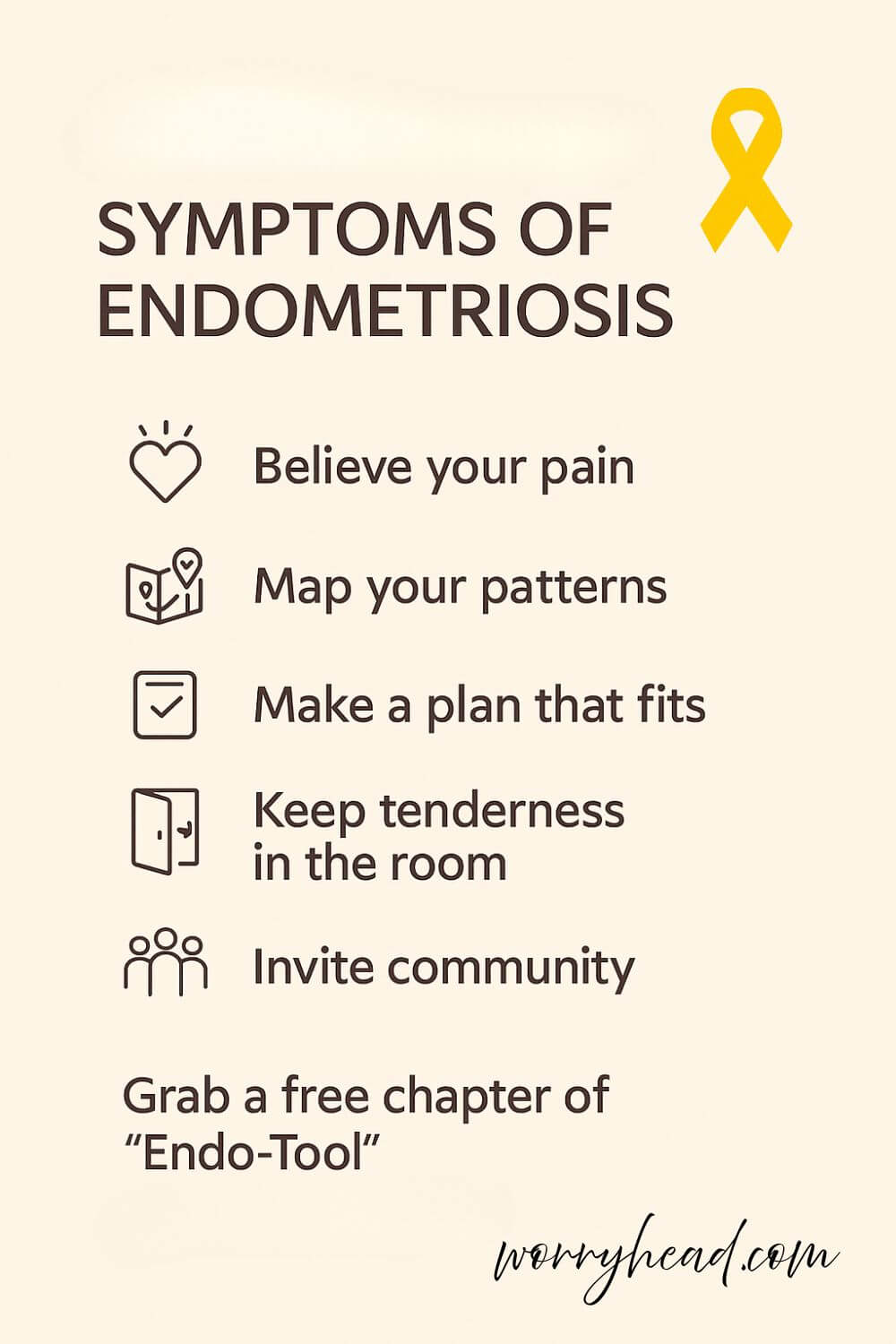
Symptoms of Endometriosis
What are the symptoms of endometriosis, and how can you tell when “bad cramps” are something more serious?
Endometriosis most often causes pelvic pain that worsens around periods, but it can also bring heavy or irregular bleeding, pain with sex, bowel or bladder pain, fatigue, bloating, leg pain, and fertility problems; symptoms vary widely, and severity doesn’t always match what you feel in daily life.
Beyond the usual pelvic pain, endometrial-like tissue can irritate nearby organs and nerves, so symptoms sometimes show up as bowel or bladder pain, rectal bleeding, or even chest and shoulder pain if the diaphragm is involved.
Some people have minimal pain yet struggle with heavy bleeding or fatigue; others have severe pain with few findings on scans. Symptoms can start in adolescence and, while they often ease after menopause, they can persist. In the UK, many wait years for a diagnosis, which is why early, attentive listening to patterns and triggers matters so much.
When my wife first described her pain, it wasn’t just “period pain.” It was waves that stole her breath, bowel pain that made her fear meals, and fatigue that blurred whole days. Loving her meant learning her patterns, believing her the first time, and pushing until someone finally listened.
If endometriosis is part of your story, you can grab a free chapter of my “Endo-Tool: Endometriosis for Men.” By joining, you’ll also become part of our community where I send real help, more freebies, and big discounts on all our books to support you both as you adjust to the new normal chronic illness brings.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis, and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men

- Understanding the Symptoms of Endometriosis
- Track Your Cyclical Pain Patterns
- Log Bowel and Bladder Changes
- Note Ovulation Versus Period Pain
- Map Your Endometriosis Bloating Triggers
- Record Leg, Hip, and Back Pain
- Document Bleeding, Clots, and Spotting
- Capture Fatigue, Mood, Sleep Dips
- Screen for Pelvic Floor Tension
- Prepare a Symptom Timeline Summary
- Making Sense of Symptoms of Endometriosis
- Building a Life Around the Symptoms of Endometriosis
- Living With the Symptoms of Endometriosis
- Final Word on Symptoms of Endometriosis
- Symptoms of Endometriosis FAQ
- Symptoms of Endometriosis References
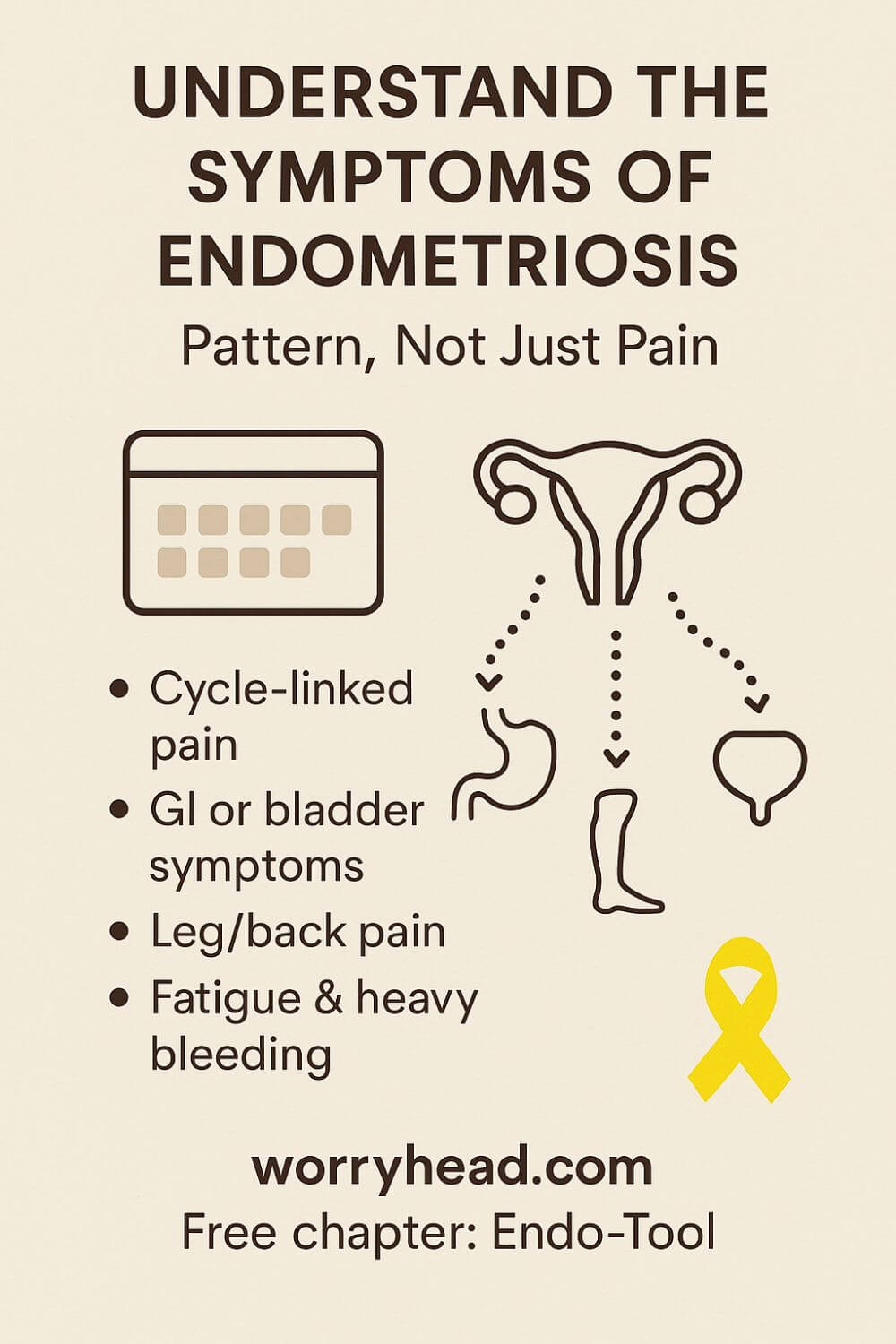
Understanding the Symptoms of Endometriosis
When people ask me what the symptoms of endometriosis look like in real life, I tell them they can be a shape-shifter that refuses neat boxes. One month, the pain limps in like a dull ache; the next, it roars, sharp and burning, stealing posture and breath.
Some women feel it mainly around periods as painful periods that build before bleeding and linger after. Other women notice mid-cycle flare-ups around ovulation that make routine tasks weirdly hard.
Intimacy may sting or feel deep, dragging, a pain with sex that can turn connection into fear. Bowels and bladder often join the story, so bathroom trips come with cramping, urgency, or pain when passing stool or urine.
That is why people are sometimes told it is IBS or endometritis when the real issue sits outside the organs, irritating them. The gut can bloat hard like a drum, what many call endometriosis bloating, and clothes that fit in the morning feel tight by evening. Some feel aches that shoot into the lower back, hips, or thighs; endometriosis pain in the legs is a clue that nerves may be involved.
Fatigue is not just tiredness; it is bone-deep, the kind that makes simple plans feel heavy.
Bleeding patterns can change, from spotting to heavier flow, and clots can appear without warning. When the disease touches the bowel, rectal bleeding can appear with periods; when the bladder is involved, blood in urine may show up rarely.
A few even feel shoulder or chest discomfort when the diaphragm is irritated, one of those uncommon symptoms that sounds unreal until it happens.
Fertility questions often surface long before anyone says the word clearly, and hope starts wrestling with worry. Conditions like adenomyosis, fibroids, and pelvic inflammatory disease can mimic parts of this picture, so careful history and exam matter.
What helps is pattern-spotting over time, because what organs endometriosis affects varies, and your map of pain tells the best truth.
With my wife, mapping those patterns changed everything. We moved from doubting ourselves to bringing a clear timeline to appointments, and suddenly, doors opened that had been closed for years. To make that shift easier for you, the next section breaks down simple, life-useful steps we use during flares and between them:
- Track cyclical pain patterns
- Log bowel and bladder changes
- Note ovulation versus period pain
- Map endometriosis bloating triggers
- Record leg, hip, and back pain
- Document bleeding, clots, spotting
- Capture fatigue, mood, sleep dips
- Screen for pelvic floor tension
- Prepare a symptom timeline summary
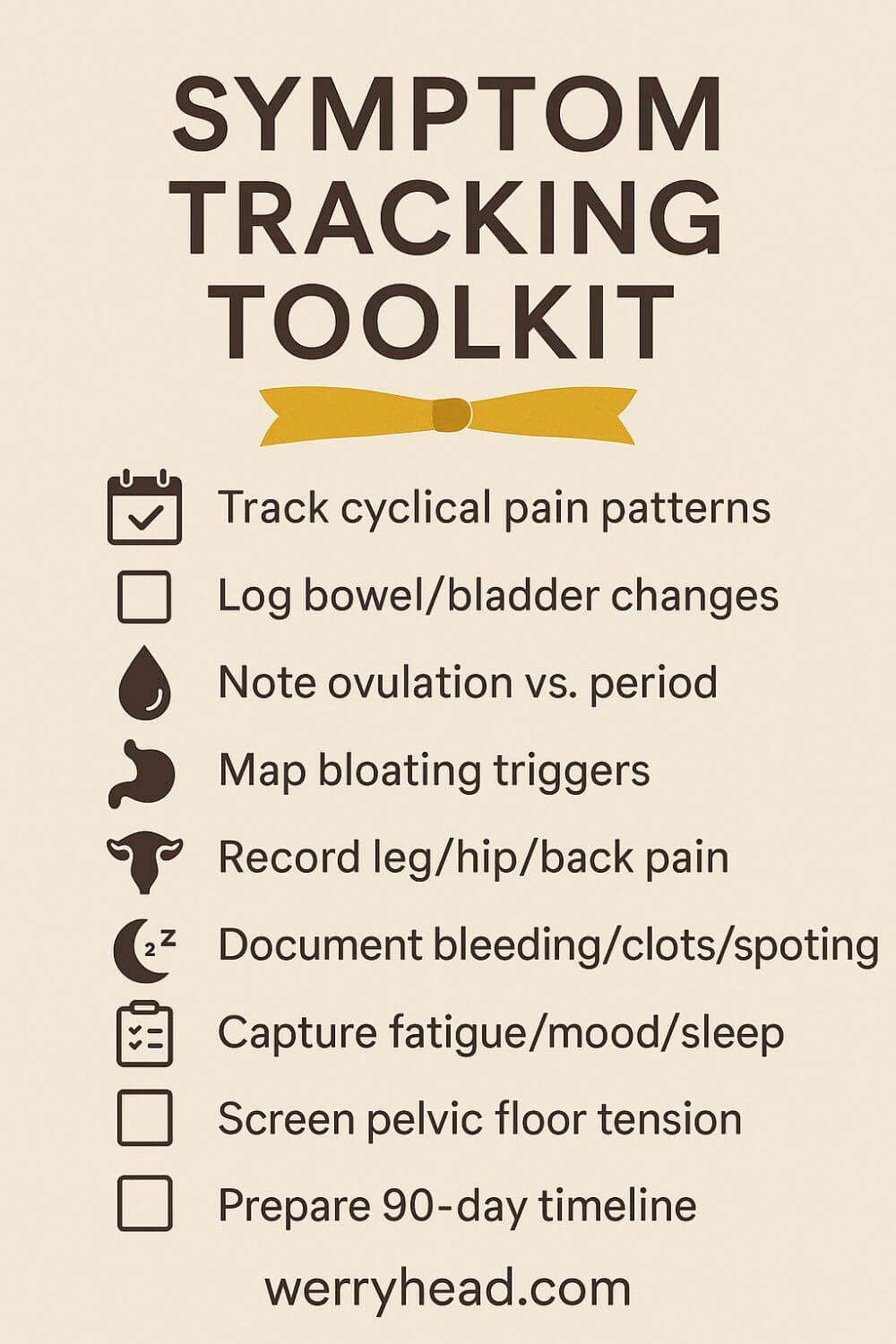
Track Your Cyclical Pain Patterns
Start with a simple calendar and commit to recording pain intensity twice a day. Give each area its own row: pelvis, lower back, hips, legs, bowel, bladder, and headaches. Add a short note for context, such as a stressful day, a long drive, or a heavy workload, because triggers often stack and blur the signal.
Within two cycles, you will see patterns that memory easily loses. Flares that seemed random often cluster in the days before bleeding or during ovulation. Noting the start and end of each symptom teaches you how long a wave lasts, which is vital for endometriosis management and pacing daily plans.
When my wife and I mapped this way, we gained language for appointments and a plan for endometriosis pain relief. Instead of saying it hurts, we could say deep pelvic pain rises on day minus two and eases on day three, with bowel cramping on day one. That clarity reduces doubt and invites better care.
Log Bowel and Bladder Changes
Use a discreet note on your phone to track bowel movements, urgency, constipation, diarrhea, and any rectal pain. Pair it with what you ate and when, since fiber, caffeine, or ultra-processed foods can nudge symptoms. Add water intake, any medications, or supplements on that day.
Flag bowel cramps tied to the cycle, because inflammation can irritate the bowel even without visible disease inside it. For bladder, note frequency, burning, pelvic pressure, or blood in urine; endometriosis can rarely cause these symptoms, especially around periods. Describe the quality of pain: sharp, burning, ache, or spasm.
This log helped my wife separate food triggers from hormonal flares. Once we saw patterns, small choices like warm breakfasts, gentler fiber, and timed hydration reduced fear of leaving the house. The point is not perfection but confidence that builds when your body’s messages finally have a paper trail.
Note Ovulation Versus Period Pain
Mark ovulation days on your calendar using symptoms like clear stretchy mucus, mittleschmerz twinges, or an inexpensive LH strip. Then watch what shifts: for some, ovulation brings knife-like pain, while periods bring a deep, dragging ache. Different peaks hint at different pain generators.
If ovulation is the spike, talk with your clinician about options that blunt that mid-cycle inflammation. If the period is the storm, heat, pacing, and targeted endometriosis pain relief might matter most in that window. The distinction will also change how you plan travel, intimacy, and workload.
We learned to schedule big tasks outside my wife’s red zones. Guarding those days protected dignity and peace at home. It is not giving in; it is a strategy, the same way athletes plan around recovery because they respect their bodies and want a longer, steadier season.
Map Your Endometriosis Bloating Triggers
Endometriosis bloating can feel like a balloon inflating under the ribs and pelvis by late afternoon. Keep a short list of foods and contexts for a week: high salt meals, carbonated drinks, tight waistbands, heavy sitting, or high stress meetings. Each one can amplify fluid shifts and gut sensitivity.
Add timing to your notes, morning flat, evening drum, or constant distension. Pair patterns with your cycle data to see whether the luteal phase magnifies bloat. Gentle adjustments help: slower meals, warm teas, looser clothes, short walks after eating, and an endometriosis diet that centers on simple, soothing foods.
When my wife stopped blaming herself for a body that changed shape by dinner, shame faded and practical steps took its place. We learned to keep soft waist trousers at hand, plan lighter dinners on flare days, and move in ways that reduce pressure rather than push against it.
Record Leg, Hip, and Back Pain
Pain that travels to the legs, hips, or back can point to nerve irritation or deep pelvic structures. Draw a stick figure and shade where it travels, front, side, or back, and whether it is pins and needles, burning, or dull. Note positions that worsen it, like prolonged sitting or bending.
Alternate heat and gentle mobility during spikes, and record what helps. Ten minutes of floor stretches, a warm bath, or short walks can interrupt the loop when used early. If pain shoots down the leg or numbness appears, bring that map to your clinician since targeted therapy or pelvic floor care may help.
For us, naming the path of pain made it less scary. We learned to swap chores on bad days, choose chairs with support, and change posture before the ache shouted. Those tiny adjustments protect energy and keep hope alive during long investigations and referrals.
Document Bleeding, Clots, and Spotting
Track flow with simple labels, light, moderate, heavy, and add start and end times. Note clots, their size, and whether cramps worsen just before they pass. Record any spotting between periods or after sex, because patterns guide next steps and help rule out mimics like adenomyosis or fibroids.
If rectal bleeding appears with periods, write it plainly and seek timely advice. The same goes for any urinary blood, especially with pelvic pain. Data reduces the burden of memory and prevents the minimizing that so often happens after a hard week when you just want to move on.
My wife’s notes turned vague frustration into clear evidence. With pages in hand, appointments felt less like auditions and more like teamwork. The record did not cure the problem, but it accelerated useful conversations and shortened the distance between symptoms and care.
Capture Fatigue, Mood, Sleep Dips
Fatigue in endometriosis is more than being tired; it is energy loss that changes how you live. Rate daily energy on a ten-point scale and pair it with bedtime, wake time, and night awakenings. Add mood words like calm, anxious, low, irritable, and note if pain and sleep are tracked together.
Small routines help buffer the crash. Preparing simple breakfasts, breaking tasks into chunks, and building a ten-minute wind-down preserves capacity when inflammation spikes. If low mood clusters with pain, consider telling your clinician; support for anxiety or depression is part of endometriosis treatment, not an extra.
With my wife, honoring fatigue reduced the guilt that once followed rest. We began to plan gentle weekends after hard cycles and to celebrate quiet wins. That shift rebuilt trust in her body and in us, which is medicine you cannot bottle, but you can practice daily.
Screen for Pelvic Floor Tension
Pelvic pain can recruit the pelvic floor into constant guarding, which adds burning, pressure, or pain with sex. Notice if inserting a tampon is hard, if sitting on firm chairs hurts, or if bowel movements feel incomplete. These clues suggest muscles are overworking to protect you.
Ask your clinician about pelvic floor physiotherapy with someone who understands endometriosis. Gentle down training, breath work, and coordination can create space again so nerves calm down. At home, try diaphragmatic breathing, soft hip openers, and avoid straining on the toilet with a footstool and relaxed posture.
The day my wife learned her pain was not her fault but her muscles trying to help, everything softened. Naming muscle tension removed shame and opened a door to targeted care. Progress is not linear, yet each small release brings back pieces of life that pain once crowded out.
Prepare a Symptom Timeline Summary
Every ninety days, compress your notes into a one-page timeline. Include the first day of your last three periods, key flares, bowel and bladder notes, bleeding changes, and what actually helped. Add questions on endometriosis you want answered, from imaging options to endometriosis management choices.
Bring two copies to appointments so you can talk while your clinician reads. This simple sheet turns a rushed visit into a focused collaboration and guards your voice when energy runs low. It also helps you notice wins, fewer pain days, better sleep, and more stable moods, which deserve space in the story.
For us, the timeline stopped the cycle of forgetting. It proved patterns we felt and highlighted the next right step. That sense of traction is powerful when living with endometriosis feels like walking uphill; it reminds you that the map is yours and the path is real.
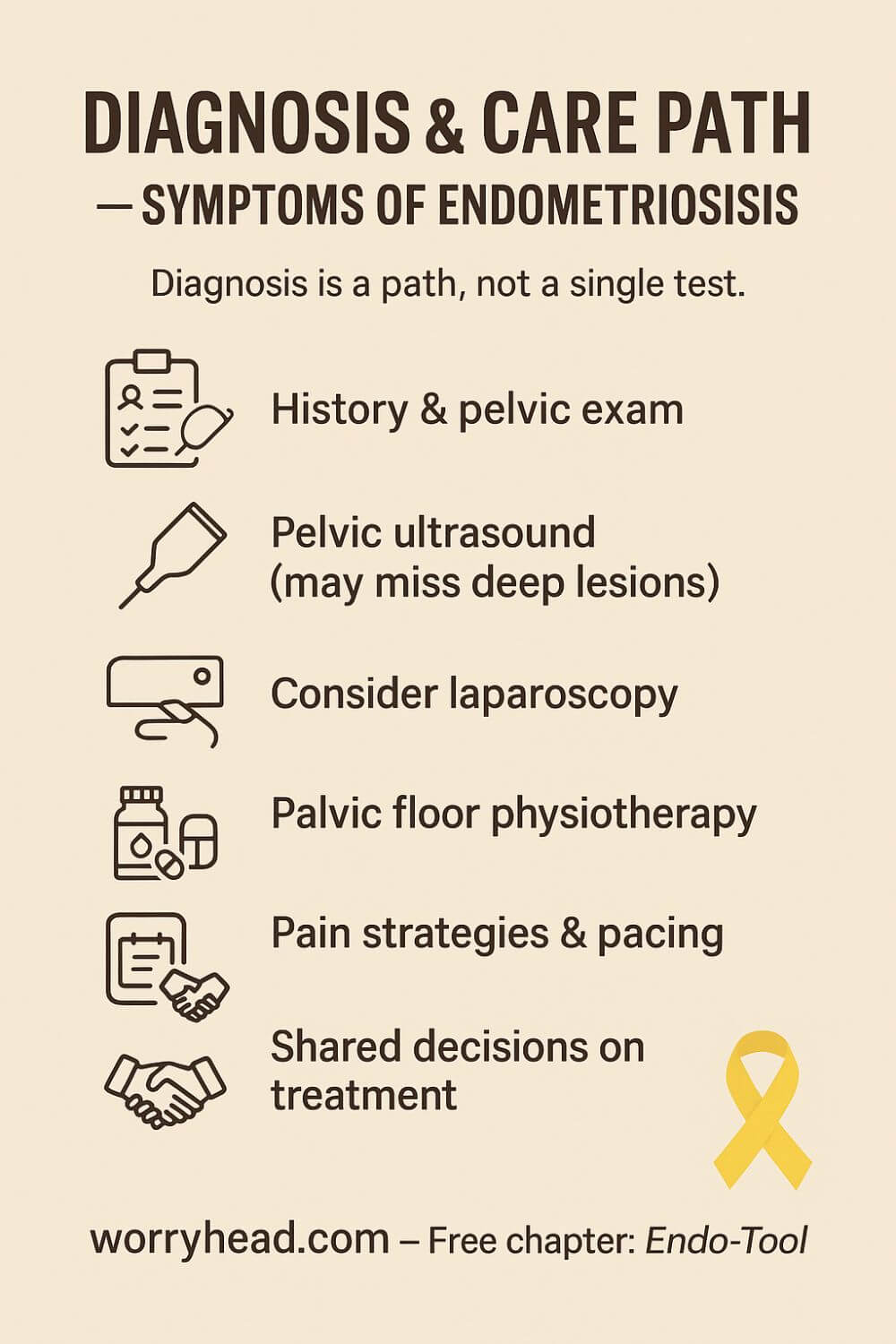
Making Sense of Symptoms of Endometriosis
Understanding the symptoms of endometriosis is less about a single list and more about a pattern that shifts with hormones, stress, and life. Your body is not confusing; it is communicating through cycles, triggers, and the way pain moves. When you learn that language, appointments stop feeling like trials and start to feel like teamwork.
Pain often begins in one place and teaches neighboring tissues to guard. Nerves get louder, muscles brace, and the pelvis holds its breath. This is not a weakness; it is a protective reflex that makes perfect sense until it starts to run the whole show.
Overlap with other conditions can cloud the picture, so you are not “dramatic” if bowel or bladder symptoms sit beside pelvic pain. Imaging may be normal even when life is not, which is why history, examination, and a clear symptom map matter. The goal is not to catch you out but to see the whole pattern you live with.
Diagnosis is a path, not a single test. A careful exam and pelvic ultrasound can find some clues, yet small or deep lesions may hide from scans. Laparoscopy can confirm and sometimes treat, but the right timing depends on your story, your goals, and the balance between relief, risk, and recovery.
Treatment is not a scorecard of how tough you are. It is a toolbox that can include symptom diaries, pelvic floor therapy, pain strategies, and medical options chosen for your body and your plans. The best plan changes as you do, and that is a sign of wisdom, not failure.
I remember the first appointment where my wife was truly heard. She cried from relief more than pain, and I did too, quietly, in the corner of that room. Someone finally mirrored back her reality, and in that moment, hope felt heavier than fear.
At home, we made space for the hard days and stopped apologizing for them. We learned to protect energy like a budget, to choose comfort over pride, and to celebrate the soft wins that never make headlines. Healing did not mean pretending; it meant being believed.
If you are reading this and wondering whether your story is “bad enough,” your story is enough because it is yours. Bring your maps. Bring your questions. We will keep walking until the picture makes sense and the next step is clear.
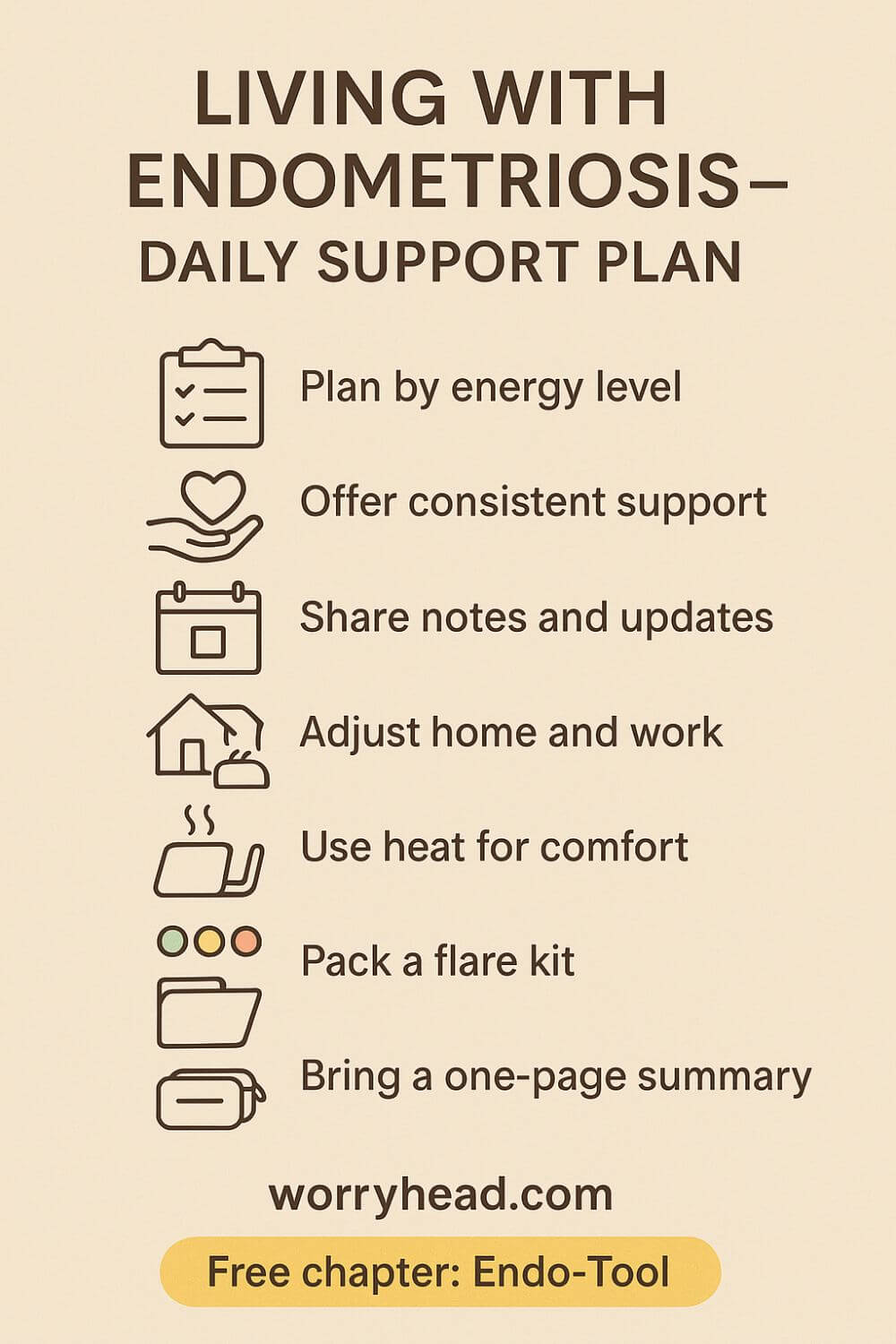
Building a Life Around the Symptoms of Endometriosis
Once we had a name, we started planning care like project managers with heart. We listed the symptoms of endometriosis that hit hardest and matched each one to a simple, first response we could try at home. That shift turned chaos into steps we could take, even on bad days.
Before appointments, we chose three goals and one decision we hoped to make, then wrote the shortest story that could guide the visit. We brought recent records in a clear folder and agreed on one question we would not leave without answering. Clarity protected energy when time felt tight.
At work, we asked for flexibility that actually helps, quiet start-of-week mornings, longer breaks during pain spikes, and the option to work from home after procedures. We framed it as performance protection, not special treatment, because stability is good for everyone. The right chair and heat access were small, powerful wins.
At home, we learned a new language for intimacy that honors comfort and desire at the same time. We named green, yellow, and red days so closeness never felt like a test. When fear softened, tenderness grew in all the places pain had tried to close.
We built a flare kit that waited for us instead of the other way around: heat, gentle stretch cards, soft clothes, easy meals, and a short list of meds to discuss with a clinician. We set thresholds for seeking urgent help so we would not argue with pain at midnight. Plans calm the room even when symptoms do not.
Travel became a ritual of care, booking seats near aisles, packing warm layers, spacing activities, and scheduling a recovery day on return. We learned that joy lands deeper when the body is respected. Saying no was not losing life; it was choosing the pieces that matter most.
There are nights I hold her while the room goes quiet and the future feels heavy. I still whisper the same promise I made at the start, that we will keep learning, keep adjusting, keep finding pockets of light. Love did not cure pain, but it made a wide enough place for hope to live.
Living With the Symptoms of Endometriosis
On quiet mornings, we plan the day by energy, not ambition. She names one non-negotiable need; I name one way I’ll carry the load so her body has room to breathe.
We keep a shared notes doc with medication changes, side effects, and questions to ask, so neither of us has to hold it all in our head. During flares, I switch from problem-solver to steady presence by offering short choices that feel doable right now.
We budget for care like other families budget for holidays, setting aside for scans, pelvic floor physio, and travel cushions, because safety has a cost. Friends know our green, yellow, red system and step in with school pickups or soup when the color turns.
Intimacy stays kind because we center comfort, using heat, pacing, and slow check-ins, and we give ourselves permission to try again tomorrow without guilt. When fear rises, we anchor to three truths we say aloud: she isn’t broken, I’m not going anywhere, and together we’ll choose the next tiny step.
On clinic days, we bring a one-page summary and agree on the single outcome that would make the visit a win, whether that’s trialing a new endometriosis pain relief option or clarifying the plan after imaging. Naming roles helps too; she tells her story, I handle logistics, and advocate if the room drifts.
Most of all, we remember that the symptoms of endometriosis affect two lives but one partnership, so we schedule joy on purpose, celebrate the quiet victories, and keep a little room ready for hope.
Final Word on Symptoms of Endometriosis
Living with this disease taught us something I wish someone had told us at the start: progress feels like a mosaic, built from tiny tiles of noticing, naming, and choosing. No single appointment fixed everything. What changed our days was learning the pattern, preparing for hard moments, and defending the pieces of life that make it worth living.
We learned to lead with belief. When pain spiked, we treated her story as data, not doubt. We captured timings, triggers, and what actually helped, then carried that map into the room so care could meet reality. Clarity turned visits into decisions instead of debates.
At home, we practiced gentleness that looks like strength. Heat before tasks. Meals that soothe. Rest without apology. We adjusted work where we could, asked for practical flexibility, and set boundaries that protect energy the way a budget protects savings. Dignity loves foresight.
Intimacy changed shape, yet it never left. We made green, yellow, and red days our shared language so touch stayed kind and pressure had no seat at the table. We kept tenderness in the room even when romance needed a rain check, because love is bigger than any bad day.
Hope grew when we stopped measuring worth by productivity. We celebrated quiet wins: a shorter flare, a calmer night, a clear scan, or simply laughing together after a storm. Those moments are not small. They are proof that joy can live beside pain without asking permission.
We built a support circle that understood the rhythm. Friends learned how to help, not with grand gestures but with soup, rides, and space. Clinicians who listened became partners. Therapy made room for grief and gave us tools for fear. None of this is weakness. It is a strategy.
If you are early on the road, start simple: notice, record, bring your one-page summary, ask one clear question, and decide on one next step. If you are further along, keep revisiting what matters now. Plans change, and that is allowed. Wisdom is iterative.
Through it all, I have watched the person I love show courage in ordinary ways. She keeps going, not because pain is light, but because her life is bigger. I stand next to her, not as a hero, but as a husband who promised to stay. Together, we keep choosing light.
If you ever doubt yourself, remember that the symptoms of endometriosis can be loud one month and whisper the next, and both deserve care. Your story is valid on the days you work and on the days you rest. Pain does not make you less; asking for help does not make you weak; choosing joy is not denial, it is resilience.
In short, you deserve care that sees the whole picture, and you are allowed to build a life that fits your body. Let this be your reminder to start where you are, use what you have, and take the next honest step. That is how we move from surviving to living.
You deserve care that believes your story and a plan that fits your body. Start small: map patterns, bring a one-page summary, ask one clear question, and decide on one next step. Protect energy, keep tenderness, invite help. You are not a burden. You are building a life where hope and joy have room to stay.
Have a question or a story to add? Leave a comment below, and if you’d like deeper support, grab a free chapter of my “Endo-Tool: Endometriosis for Men.”


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MORESymptoms of Endometriosis FAQ
1) Is endometriosis cancer?
No. Endometriosis is a benign condition, though a small, overall low increase in ovarian cancer risk is reported. The disease can also form ovarian cysts (endometriomas) and adhesions that drive pain without being malignant.
2) Do symptoms always ease after menopause?
Often—but not always. Many people notice improvement, yet pain and other symptoms can persist or recur, especially with hormone therapy or if deep disease remains.
3) Can symptoms affect places beyond the pelvis (legs, chest, shoulder)?
Yes, though it’s uncommon. Nerve involvement can refer pain into the back, hips, or legs; diaphragmatic disease can cause chest/shoulder pain or even bleeding with periods. If you spot these patterns, document timing and seek review.
4) Do you need surgery to diagnose it?
Laparoscopy is the only way to confirm endometriosis with certainty, but many clinicians begin treatment based on history, exam, and imaging while discussing if/when to pursue surgery. Bring a one-page symptom timeline to guide that decision.
5) What else can mimic these symptoms?
Common look-alikes include pelvic inflammatory disease, ovarian cysts, irritable bowel syndrome, adenomyosis, and fibroids. Careful pattern-tracking plus targeted exams and imaging help tell them apart.
Symptoms of Endometriosis References
- https://www.nhs.uk/conditions/endometriosis/
- https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656
- https://womenshealth.gov/a-z-topics/endometriosis
- https://www.nichd.nih.gov/health/topics/endometri/conditioninfo/symptoms
- https://www.who.int/news-room/fact-sheets/detail/endometriosis