Endo vs IBS vs IBD Flare Ups
Some nights, I held my wife’s hand through waves of pelvic pain, whispering that we would learn her patterns and take back a little peace. So when pain spikes, how do you tell an endo vs IBS vs IBD flare apart in real life?
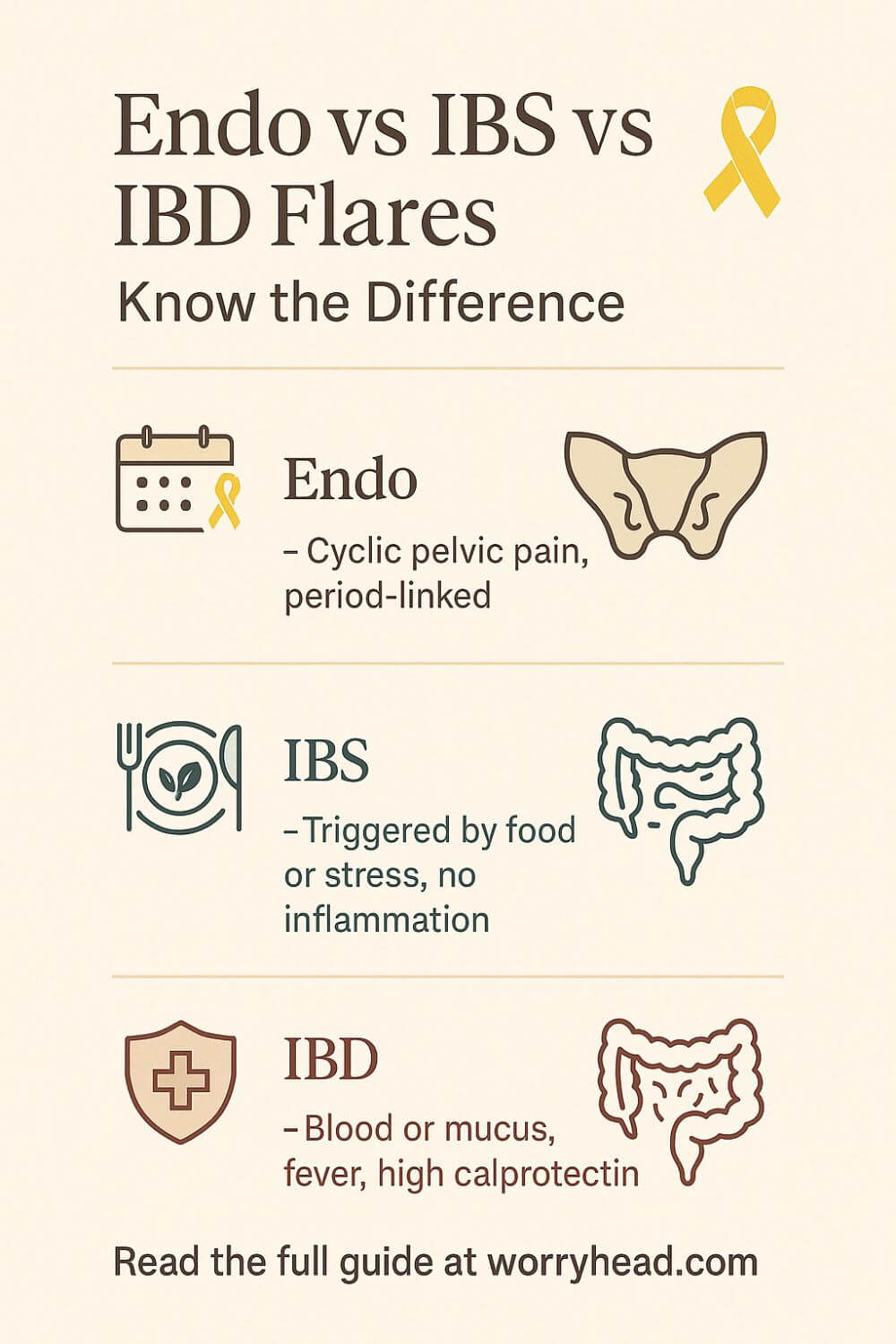
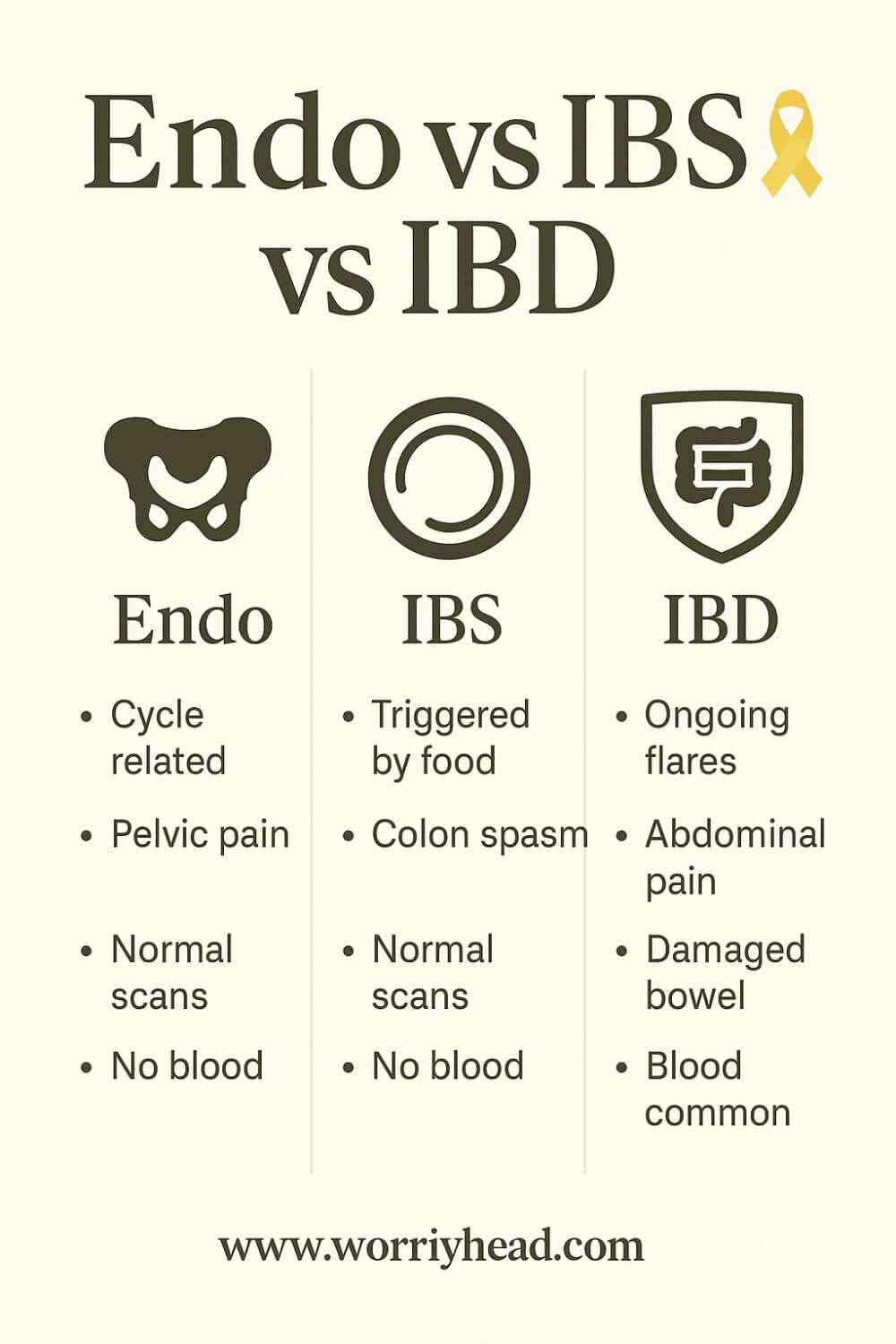
An endo vs IBS vs IBD flare differs by timing, biomarkers, and visible inflammation: endometriosis flares often cluster around menstruation with pelvic pain; IBS flares show gut sensitivity without tissue damage; IBD flares cause inflammatory diarrhea, bleeding, fever, and raised calprotectin.
Patterns matter because gastrointestinal disorders overlap in messy ways. Endo flare-up can look like an IBS flare-up, and IBD can masquerade as IBS when symptoms are mild. I’ve watched how cycle timing, bowel movement remedies, and food choices change the picture, and I want that clarity for you.
Grab a FREE chapter of my eBook to make sense of these patterns, meals, and symptom trackers. By joining our community, you’ll get more freebies, big book discounts, and steady, compassionate emails to help you adjust to the new normal chronic illness brings.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis, and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men

Endo Flare Up
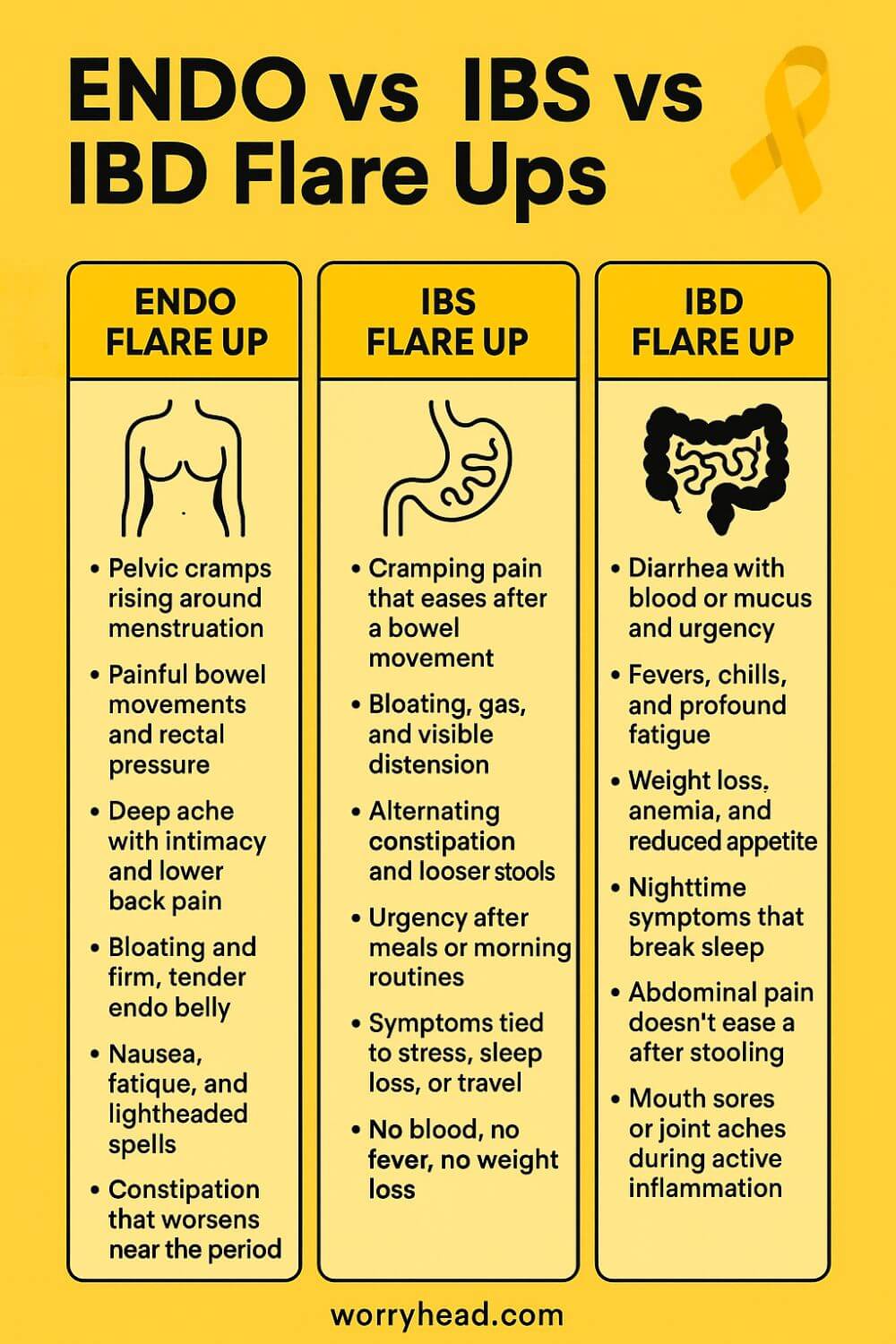
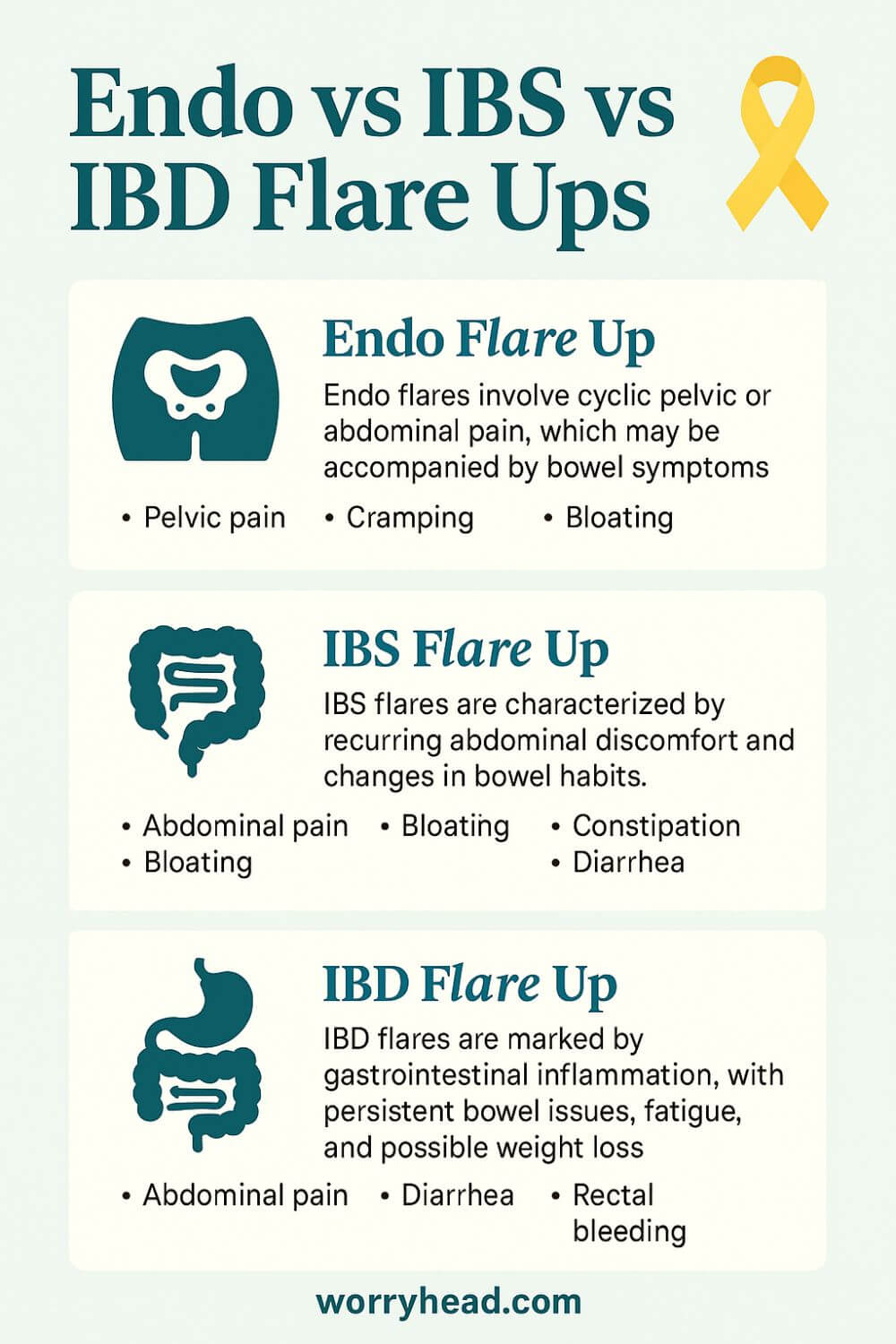
A surge of cycle-linked pelvic pain, bowel cramping, and deep ache around periods; endometriosis can inflame nerves and tissue, stirring endo belly, painful bowel movements, and fatigue. Flares often echo hormones, not food alone, and need calm, tracking, and targeted care. Patterns track cycles.
- Pelvic cramps rise around menstruation
- Painful bowel movements and rectal pressure
- Deep ache with intimacy and lower back pain
- Bloating and firm, tender endo belly
- Nausea, fatigue, and lightheaded spells
- Constipation that worsens during the period
When an endo flare-up rolls in, I look first at the calendar, because timing is a compass. Pain often climbs before bleeding, sharpens during the period, and lingers after, turning the pelvis into a clenched fist. Alongside cramps, there may be rectal pressure, painful bowel movements, deep ache with intimacy, and a swollen, rigid endo belly.
I have watched meals matter, but do not rule the day. A bland lunch can hurt if hormones are pouring petrol on nerves, while a gentle soup can land softly when the cycle is quiet. That is why food logs help, but cycle tracking tells the fuller story. Imaging can guide us, yet bowel endometriosis may sit outside the lumen, so scopes return normal even when pain is real.
During a surge, we simplify routines: heat, hydration, and stillness. We choose IBS-friendly food only because the gut is tender, not because this is IBS. Magnesium baths, soft breathwork, and predictable bedtimes steadied my wife when panic once owned the night. On travel weeks, we protect sleep and pack quiet snacks.
Doubt hurts. When someone calls it “just stress,” I remember the scars of excision and the days she missed from life. Validation is medicine. Clarity lets us act early and keep hope intact even when the body argues back.
IBS Flare Up
A sudden wave of cramping, bloating, and bowel urgency after meals or stress; IBS flares heighten gut sensitivity without structural damage. Symptoms ease with stooling or gentle diet shifts, not antibiotics. Track triggers, support the nervous system, and pace days. Night pain is a red flag. See GP!
- Cramping pain that eases after a bowel movement
- Bloating, gas, and visible distension
- Alternating constipation and looser stools
- Urgency after meals or morning routines
- Symptoms tied to stress, sleep loss, or travel
- No blood, no fever, no weight loss
An IBS flare-up feels like the gut flips its sensitivity dial to maximum, often after a rushed breakfast, broken sleep, or travel. Bloating rises, cramps come in waves, and relief sometimes follows a bowel movement. Unlike irritable bowel disease, there is no tissue damage here, just a nervous system on edge.
What helped were small, kind experiments. We tested IBS breakfast ideas that did not pick fights with her belly, leaned on IBS-friendly meals in steady portions, and kept a short list that matched our kitchen. When stress climbed, symptoms swelled, so we added buffers: earlier dinners, slower mornings, a short walk before emails.
Triggers are personal. Carbonated drinks and fried takeaways were loud; ripe bananas and plain rice were quiet. Soluble fiber and hydration tempered urgency, while grazing made cramps worse. The aim was fewer spikes and steadier afternoons.
I learned to check the clock. Nocturnal diarrhea, blood, fever, or weight loss do not fit IBS and need medical attention. When red flags were absent, simple bowel movement remedies and heat helped. On travel days, we pack snacks, water, and guard sleep.
With time, the body trusted us again. Patterns grew clearer, and confidence replaced fear. IBS asks for gentleness, structure, and listening sooner.
IBD Flare Up
Escalating abdominal pain, diarrhea with blood or mucus, fever, and fatigue signal inflammatory bowel disease in flare. This is immune-driven inflammation that injures tissue, not a functional spasm. Seek medical care; monitor calprotectin, hydration, and anemia risks promptly. Night stools matter!
- Diarrhea with blood or mucus and urgency
- Fevers, chills, and profound fatigue
- Weight loss, anemia, and reduced appetite
- Nighttime symptoms that break sleep
- Abdominal pain that does not ease after stooling
- Mouth sores or joint aches during active inflammation
An IBD flare-up is a different beast: the immune system lights the gut, and tissue shows it. Diarrhea may come with blood or mucus, urgency crowds the day, and fatigue leaks into every corner. Fevers, weight loss, and anemia creep in, shrinking appetite and confidence together.
When these signs appear, we do not self-manage; we call care teams. Hydration, labs, and stool tests like calprotectin tell us what symptoms cannot, and treatment plans follow. An IBD diet supports healing but does not replace therapy; the priority is calming inflammation so the bowel can rest.
At home, we protect energy. Simple meals, electrolytes, and quiet routines reduce strain, and we avoid risky add-ons. Travel needs planning: medication access, safe foods, and rest windows.
Red flags are not stories to tough out. Nocturnal diarrhea, persistent bleeding, rising fevers, or severe cramps demand escalation. Early help shortens suffering and prevents complications.
In the middle of it, love still has room. We sit with tea, name the fear, and measure progress by small markers: one steadier morning, one quiet night. This is irritable bowel disease, yes, but it is also a life, and lives deserve tenderness alongside science.
Understand an Endo vs IBS vs IBD Flare
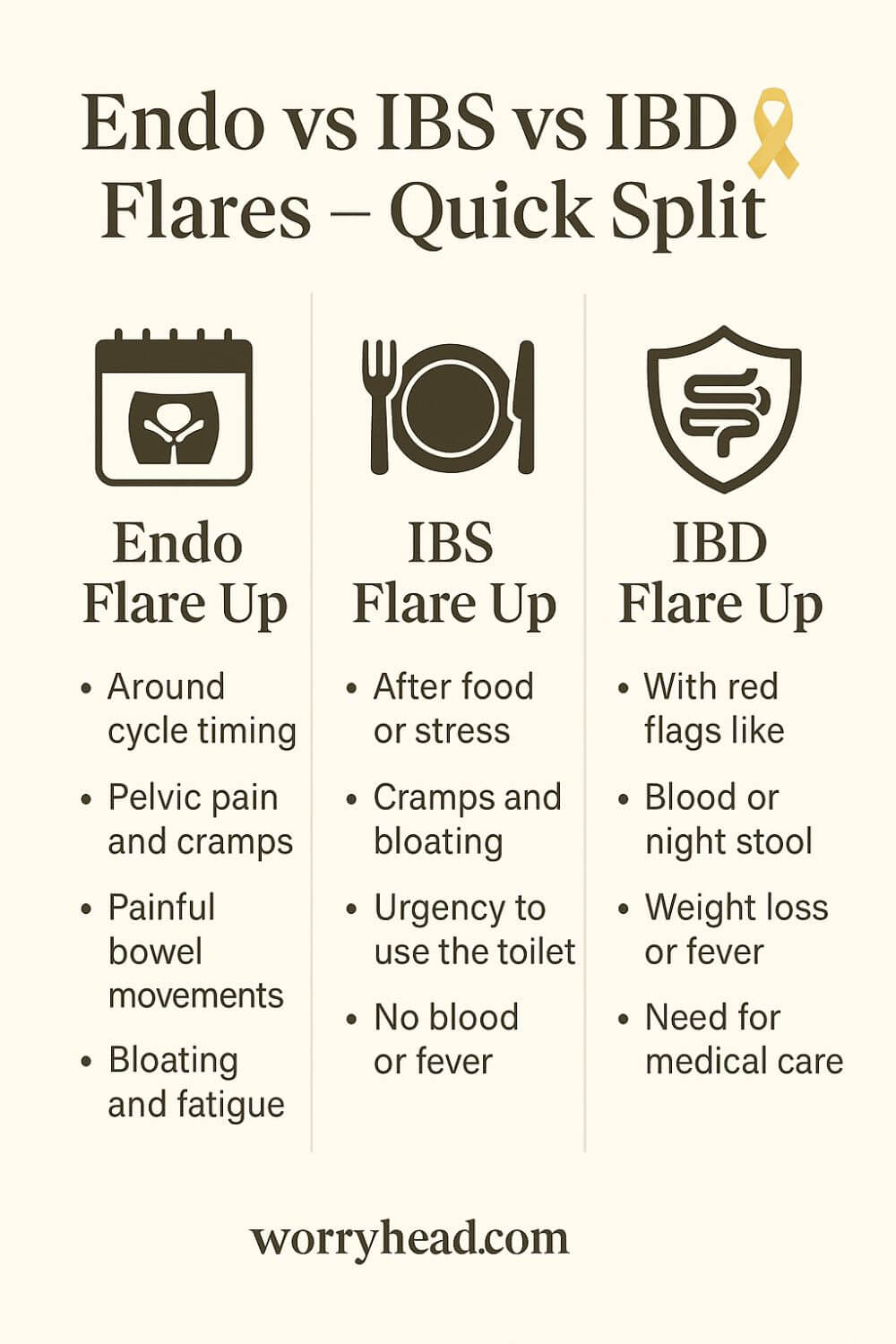
When my wife clutches her belly and breathes through a storm of cramps, I start with patterns. Endometriosis often surges around the menstrual cycle, while IBS changes with meals, stress, sleep, and travel, and IBD carries the heavy footprints of inflammation that do not just pass with time.
I map the days against her cycle and write down symptoms the way a pilot logs weather. Bloating that rises and falls with periods points me to endometriosis, especially when ovarian pain and endo belly arrive like clockwork. If urgency follows breakfast and calms after a bathroom trip, I think about an IBS flare-up and what was on the plate.
Food becomes data, not blame. An IBS meal plan built from IBS-friendly food can soften spasms, while caffeine, alcohol, and ultra-processed snacks can stoke them. Gentle switches toward IBS-friendly recipes and an anti-bloat diet often lower the volume without medication.
Inflammation tells another story. When fatigue deepens, stools loosen with mucus or blood, and weight dips, I worry about irritable bowel disease, and I reach for medical support quickly. That is when an IBD diet is supportive but never a substitute for proper treatment and monitoring.
I learned to read the bathroom like a dashboard. A simple bowel movement chart helps us spot changes long before panic sets in. Small wins, like consistent hydration and fiber the gut actually tolerates, are not glamorous, but they steady the day.
Comorbidities can blur the picture.
With Ehlers-Danlos syndrome or hypermobile Ehlers-Danlos syndrome, pain sensitivity climbs and joints complain, which can make gastrointestinal disorders feel louder than they already are. That is not imagined pain; it is the nervous system trying to protect a body that has been through too much.
Stress matters, but it is not the villain behind every symptom. My wife’s body remembers surgeries, scans, and dismissive rooms, memories that can amplify a flare even when the day is calm. Slow routines, warm pads, and predictable meals put gentleness back in the driver’s seat.
We keep a simple tracker that notes sleep, meals, movement, and symptoms. Over weeks, a pattern forms that separates an endo flare-up from the churn of IBS. That same log helps us see when red flags suggest escalation rather than another round of home care.
Sometimes the picture is mixed. IBS relief techniques soothe cramping, yet cycle-linked pain persists, nudging us to revisit pelvic imaging for endometriosis. When nighttime diarrhea appears or fevers creep in, we move beyond diaries and straight to clinicians.
The phrase endo vs IBS vs IBD flare is not a slogan to me; it is a map I built out of fear and love. It is how I choose the right response at the right time, so my wife does not have to fight every symptom with the same blunt tool. Precision lowers suffering, and that is the point.
Travel adds another layer. Airports, irregular meals, and disrupted sleep can rattle IBS and make IBD management harder, so we plan snacks, fluids, and rest the way other couples plan sightseeing. Safety is romance when illness is your third passenger.
At home, the kitchen is our clinic. We rotate gentle breakfasts, test one new ingredient at a time, and respect the body’s feedback. None of this is dramatic, yet it is how good days quietly multiply.
I have made mistakes, pushing through a flare because a deadline sneered at us. The body always sends the bill. Now we pivot quickly, choosing rest, heat, and foods that ask less of a weary gut.
For anyone navigating similar storms, you are not weak for needing structure. You are wise for listening sooner. Clarity is a kind of mercy we can all afford to give.
| Feature | Endometriosis flare | IBS flare | IBD flare (Crohn’s/UC) |
|---|---|---|---|
| Typical triggers/pattern | Cyclical—often perimenstrual; can follow hormonal shifts. | Food triggers, stress, travel, infections; functional hypersensitivity. | Immune-mediated inflammation; flares/remission course. |
| Pain quality & location | Pelvic ± lower back; dysmenorrhea; pain with sex (dyspareunia) and bowel movements (dyschezia); can mimic bowel cramps. | Crampy abdominal pain with bloating; relieved or provoked by stooling; variable pattern. | Crampy abdominal pain with urgency; often steady/worsening without treatment. |
| Stool findings | Usually no blood (unless bowel endometriosis invades mucosa; uncommon). | No blood (mucus can occur). | Blood and/or mucus common (especially UC). |
| Systemic “red flags” | Typically absent; severe fatigue common but no fever/weight loss from gut inflammation. | Absent (fever, weight loss suggest not IBS). | Fever, weight loss, anemia can accompany flares. |
| Objective tests | Imaging (expert TVUS/MRI) for deep disease; laparoscopy if needed. Colonoscopy often normal because lesions are external to bowel. | Labs/imaging normal; diagnosis by Rome criteria/positive diagnosis after excluding “red flags.” | ↑ Fecal calprotectin/CRP, anemia; endoscopy shows inflammation/ulcers; biopsy confirms. |
| Course if untreated | Pain/disability persists; bowel symptoms may wax/wane with cycle. | Chronic, functional; does not damage bowel. | Progressive inflammatory damage and complications if uncontrolled. |
Before I share what helps us most, know this came from nights when I counted her breaths and prayed the pain would loosen its grip. If that tenderness touches something in you, take these next steps as a hand on your shoulder, not a lecture.
- Track cycles and symptom peaks
- Build a gentle food core
- Use a simple flare log
- Spot red flag patterns early
- Create calm morning routines
- Prepare travel-friendly meals
- Keep heat and rest ready
- Agree on escalation plans
Track Cycles and Symptom Peaks
I learned to mark the calendar the way sailors read tides. When pelvic cramps bite in the luteal phase and ease after bleeding, endometriosis steps forward. If urgency follows breakfast and settles after a bowel movement, an IBS flare-up is more likely. Nighttime diarrhea or bloody stool points to irritable bowel disease and needs swift care.
We write down the small things that are easy to ignore. Was there ovarian pain leaning to one side, or a rigid endo belly that felt tender to touch? Did a gentler dinner bring relief, or did pain ignore food altogether?
Patterns reveal themselves when emotion quiets and data speaks. A simple bowel movement chart beside a cycle log turns fog into shape. Over weeks, the difference between endo flare-up, IBS, and IBD stops being guesswork and starts being a story we can act on.
Build a Gentle Food Core
Food cannot cure endometriosis or IBD, but it can reduce chaos. We built a short list of IBS-friendly foods that landed softly on hard days, then rotated options to avoid boredom. Think oatmeal, rice, poached chicken, ripe bananas, and warm soups that ask less of a tired gut.
For visible bloating, we trialed an anti-bloat diet with fewer carbonated drinks and less fried food. On calmer weeks, we added color back. When a meal stirred cramps, we logged it without blame and returned to the core.
IBS relief often begins in the kitchen, but if blood or fever joins the table, the conversation changes. That is when irritable bowel disease must be ruled in or out, and an IBD diet becomes supportive rather than central. Gentleness is the rule, not restriction for its own sake.
Use a Simple Flare Log
Our log is plain paper, not a fancy app. Morning to night, we note sleep, meals, movement, stress, pain scores, bowel movements, and where the pain sits. Over time, we see whether cramps shadow the cycle, whether urgency follows certain breakfasts, and whether travel unravels everything.
A log does not judge. It gives us proof when a clinician asks what happens during an IBS flare-up versus an endo flare-up. It shows that scopes can be normal when bowel endometriosis lives outside the lumen, and that gastrointestinal disorders overlap in messy ways.
Most of all, it gives back control. With clarity, we plan rest days, choose IBS-friendly meals, and know exactly when to escalate. Fear shrinks when facts grow.
Spot Red Flag Patterns Early
Some signs are a hard stop. Blood or mucus in stool, fever, night waking with diarrhea, weight loss, or worsening fatigue do not belong to IBS. They belong to irritable bowel disease until proven otherwise and deserve prompt assessment and labs.
On those days, I do not troubleshoot recipes. I call for help, collect stool for calprotectin if advised, and watch for hydration and anemia risks. If pain refuses to ease after stooling, we treat it as urgent.
Catching red flags early protects the future. It shortens flares, prevents complications, and reminds us that courage includes asking for care. Precision is love put into action.
Create Calm Morning Routines Daily
Mornings can decide the whole day. We nudge wake time earlier, keep breakfast gentle, and protect a quiet half hour before screens. Warm tea, a heating pad, and slow breaths turn down the noise that makes IBS louder than it needs to be.
When endometriosis is humming, movement stays kind. Short walks loosen the hips, and a soft stretch eases lower back strain that often travels with pelvic pain. Predictability steadies the nervous system and makes IBS symptoms in women less volatile.
This is not performance. It is a humane rhythm that tells the body it is safe enough to digest, rest, and heal.
Prepare Travel-Friendly Meals Ahead
Airports, stations, and late check-ins punish the gut. We pack familiar snacks, electrolyte sachets, and easy proteins so hunger does not push us into a trap. Water beats fizz, and steady bites beat feast or famine.
For long trips, we plan stops, carry medication lists, and keep a card that summarizes endo vs IBS vs IBD flare patterns. If night symptoms or blood appear away from home, we do not wait. We seek care.
Travel can still be joy. With preparation, IBS behaves, endometriosis has fewer excuses, and IBD management stays on track. Safety makes space for wonder.
Keep Heat and Rest Ready
A heating pad is simple but powerful. Heat loosens the clenched fist of pelvic muscles during an endo flare-up and steadies cramps that mimic bowel pain. Short rests between tasks keep the stress curve low, so IBS does not spike after lunch.
We pair warmth with hydration and unhurried meals. On heavy days, we choose soft foods and quiet light. The aim is not to surrender the day but to make it gentler.
Small mercies compound. One restful hour prevents three spirals later. That is a bargain worth taking every time.
Agree on Escalation Plans Early
Before the storm, we agree on thresholds. If there is blood, fever, persistent night diarrhea, or pain that refuses to ease, we escalate without debate. If weight dips or exhaustion deepens, we call the team.
Having a plan removes arguments from bad days. It tells us when an IBD diet is supportive, when bowel movement remedies are enough, and when imaging for endometriosis needs to return to the agenda.
Clarity is dignity. It protects energy, reduces fear, and keeps us on the same side of the problem instead of on opposite ends of the room.
Living with an Endo vs IBS vs IBD Flare
I used to chase one perfect fix, until I learned that patterns decide the plan. Endometriosis demands we respect cycle timing, while IBS listens to routine and gentle food, and irritable bowel disease needs medical escalation when inflammation speaks loudly. The body is a teacher if we are willing students.
On calm weeks, we build strength quietly. We rotate IBS-friendly meals, keep hydration steady, and lean on a simple bowel movement chart so changes cannot hide. When bloating swells into a rigid endo belly with ovarian pain, we shift into endo care without blaming last night’s dinner.
An IBS flare-up often shrinks when mornings get kinder. A short walk, warm tea, and an IBS breakfast ideas list keep nerves from setting the gut on edge. When travel or deadlines crowd the day, we return to an IBS meal plan that feels safe and predictable.
If fatigue deepens and stools change with mucus or blood, I set down the kitchen tools and pick up the phone. That is irritable bowel disease territory, and an IBD diet supports treatment rather than replaces it. Early attention prevents long nights that nobody deserves.
Comorbidities can amplify everything. With Ehlers-Danlos syndrome, pain signaling gets louder, so gentle movement and consistent sleep are not luxuries. They are guardrails that keep gastrointestinal disorders from stealing the whole week.
Some days I forget and push too hard. She tries to smile through an endo flare-up up and I pretend we can outwork biology. We always pay for that, so now we choose rest sooner and let love be practical instead of heroic.
The phrase endo vs IBS vs IBD flare sits on a card in our kitchen to remind us that precision is kindness. It tells us which lever to pull and which to leave alone, so my wife does not have to fight every symptom with the same tool. Clarity is how we protect hope when the body is tired.
Conclusion on the Endo vs IBS vs IBD Flare
I used to believe one plan could soothe every storm, until I watched how my wife’s body spoke three different languages.
Endometriosis arrives with a calendar in its hands, tightening the pelvis and lighting up nerves near the period. IBS responds to rhythm, meals, sleep, and stress, a sensitive gut that calms when mornings are gentle and plates are simpler. Irritable bowel disease is inflammation with consequences, a flare that needs timely care, not a brave face. Learning these differences gave us space to breathe, to choose tools that match each pattern, to protect hope when nights ran long.
We started with a pencil and patience. A cycle log beside a bowel movement chart turned chaos into shape.
When pain sharpened before bleeding, when intimacy ached, when endo belly sat rigid and tender, we called it what it was, an endo flare-up, and we treated it with heat, rest, and compassion. When cramps eased after the bathroom, when bloating rose after travel or rushed breakfasts, we adjusted toward IBS-friendly food, smaller portions, earlier dinners, and the slow mornings that make IBS relief possible.
Red flags demanded a different courage. Blood or mucus in stool, fevers, night waking with diarrhea, weight loss, those were not kitchen problems. They belonged to irritable bowel disease and to clinicians who could check labs, calprotectin, hydration, and anemia. An IBD diet could support recovery, but therapy led the way. Acting early spared us harder days and deeper fear.
None of this made us perfect; it made us kinder. We stopped blaming food when hormones were shouting, stopped ignoring rest when deadlines pressed, and stopped asking one remedy to carry the weight of three conditions.
On good weeks, we rebuilt quietly, planned travel with safe snacks and water, guarded sleep, and let gentle movement loosen hips and back. On hard weeks, we measured success in small mercies, one steadier morning, one softer evening, one honest conversation that reminded us we were a team.
If you are reading this with a tight chest and a tired heart, know that precision is love in action. Endometriosis is not your fault, IBS is not a weakness, and IBD is not a character test. These are gastrointestinal disorders with different rules, and you deserve plans that respect those rules.
Pick up a pen, keep the simplest log you can, choose an anti-bloat diet on fragile days, and ask for help early when the signs are loud. You are not behind; you are beginning again with better maps, and better maps change lives.
A flare does not get the last word. You do, in the steady choices that stack into calmer weeks, in the way you name what hurts and ask for what helps, in the quiet belief that tomorrow can be kinder than today.
In the end, clarity, not perfection, is how families like ours keep going.
Our compass is simple patterns, kind meals, early red flag checks, and honest rest. With those in place, endometriosis softens, IBS steadies, and IBD gets the medical attention it deserves. You can build this, one small choice at a time.
If this helped, leave a comment and tell me where you are in the journey, and grab the FREE chapter of the eBook to keep building clarity, courage, and practical routines together.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MORE