Comorbidities of Endometriosis
What are the comorbidities of endometriosis, and how do they shape a woman’s body and daily life?
Endometriosis is linked to a higher prevalence of migraine, irritable bowel syndrome, bladder pain syndrome, anxiety/depression, allergic and autoimmune disorders (including thyroid disease), and, in some studies, greater cardiometabolic risk. Associations vary by study design, severity, and age.
Newer data-driven analyses have begun to map even wider patterns, confirming known overlaps like migraine and allergic disease while surfacing possible associations with respiratory infections and sciatica that deserve careful study.
Major guidelines now frame endometriosis as a chronic, inflammatory condition that often coexists with systemic issues, which is why multidisciplinary care matters from day one. You will see this thread through the evidence, and we will separate what is well established from what is still emerging.
My wife lives with this reality. Pain is only one part of the story; fibromyalgia, the exhaustion, the brain fog, the stomach flares, and the anxious nights are the quieter companions that most people never see. I built our work-from-home life so she could heal at her own pace and still feel safe, creative, and valued.
If endometriosis touches your relationship, you are not alone. You can grab a free chapter of my “Endo-Tool: Endometriosis for Men.” By joining, you’ll also step into our community for more freebies, meaningful support, big discounts on all our books, and honest emails that help you both adjust to the new normal with hope and practical care.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis, and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men

- Comorbidities of Endometriosis
- Track Symptom Clusters on One Timeline
- Screen Early: Gut, Bladder, Migraine
- Ask About Dizziness and POTS-Like Signs
- Check Thyroid and Autoimmune Panels
- Protect Sleep as Core Therapy
- Liveable Anti-Inflammatory Daily Routine
- Coordinate Truly Multidisciplinary Care
- Plan Fertility, Menopause, Bone-Heart
- Build Compassionate, Flexible Work-Life
- More on Comorbidities of Endometriosis
- Living with the Comorbidities of Endometriosis
- Final Word on the Comorbidities of Endometriosis
- Comorbidities of Endometriosis FAQs
- Comorbidities of Endometriosis References
Comorbidities of Endometriosis
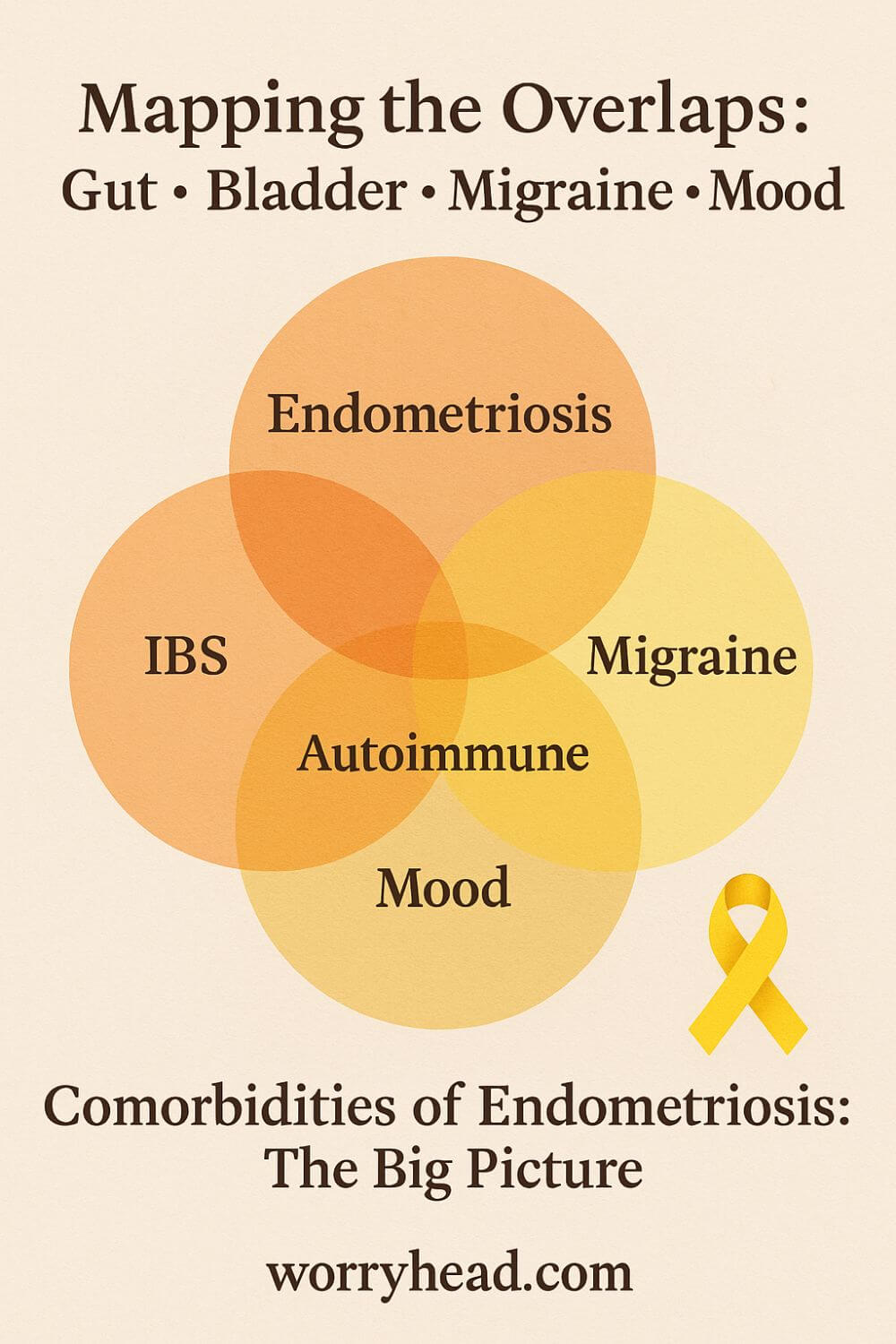
Endometriosis rarely travels alone; it clusters with overlapping pain conditions, gut and bladder disorders, migraine, mood symptoms, allergic/autoimmune tendencies, and in some cohorts, cardiometabolic and early-menopause risks. These patterns aren’t random; they reflect shared biology: neuro-immune activation, hormonal signaling quirks, and nervous-system sensitization.
Large reviews and guidelines increasingly define endometriosis as a chronic inflammatory disease, which helps explain why irritable bowel syndrome (IBS), bladder pain syndrome/interstitial cystitis (BPS/IC), and migraine so often show up together.
When inflammation, pelvic nerves, and the brain’s pain circuits stay “switched on,” symptoms spread beyond the pelvis into digestion, urination, and the head.
Population data consistently find higher odds of IBS and BPS/IC in people with endometriosis, with some analyses suggesting a several-fold increase for bladder pain. Migraine also appear more frequently, and in new data-driven maps of health records, headache disorders were present in about 29% of those with endometriosis versus 17% without.
Autoimmune and allergic patterns are reported as well—think autoimmune thyroid disease, asthma, eczema, and general atopy. These links don’t always mean causation, but they echo immune dysregulation seen in lesions and blood: cytokine shifts, altered NK-cell function, and neuro-angiogenic signaling that make pain louder and flares more likely.
Mood symptoms are not “in your head” – chronic pain rewires stress, sleep, and cognition. Anxiety and depression track with pain intensity, sleep fragmentation, and the unpredictability of flares, creating a feedback loop that magnifies suffering unless we interrupt it with validation, pacing, and multidisciplinary care.
Autonomic problems can also ride along. Studies of overlapping pelvic pain syndromes describe patterns that look like dysautonomia, orthostatic intolerance, and POTS-like symptoms in some patients, hinting at a nervous-system piece we shouldn’t ignore during assessment.
There’s an ongoing debate about cancer and cardiovascular risk. The absolute risk of ovarian cancer remains low, yet some recent analyses suggest a higher relative risk, especially with severe or deep disease, so vigilance and individualized counseling matter. Cardiometabolic risk signals are emerging and need careful, bias-aware replication.
Another fresh finding: earlier menopause risk may be higher, especially surgical menopause driven by treatment decisions, so we have to weigh pain control against long-term bone and heart health, and plan proactive monitoring where appropriate.
All of this is why I speak about comorbidities of endometriosis as part of the condition, not an afterthought. When my wife’s pelvic pain flares, her gut, bladder, head, and sleep often flare with it; once we named those links, our plan got kinder and smarter.
We built a life that flexes with those layers: work-from-home rhythms, gentler mornings, food routines that calm her gut, and appointments that actually talk to each other. It still hurts sometimes, but the map is clearer now, and that brings courage.
Before we go deeper, here are the practical moves that changed our days and may change yours; in the next section, I’ll unpack each one with step-by-step detail:
- Track clusters (pain, gut, bladder, headache) on one timeline
- Screen early for IBS, BPS/IC, migraine, and mood
- Ask about dizziness, palpitations, and POTS-like symptoms
- Run a thyroid and autoimmune check when symptoms fit
- Protect sleep as a core treatment, not a luxury
- Use an anti-inflammatory routine that you can actually live with
- Coordinate care across gynecology, gastro/urology, neurology, and mental health
- Plan fertility, menopause, and bone-heart health proactively
- Build a compassionate, flexible work-life setup

Track Symptom Clusters on One Timeline
When you chart symptoms together, patterns stop hiding. Put pelvic pain, bowel changes, bladder urgency, headaches, fatigue, and mood on the same daily line, morning to night. Note cycle day, sleep hours, stressors, food, and meds.
Two weeks later, you’ll start seeing pairings: gut cramps flaring the day before bleeding, migraine shadowing sleepless nights, bladder urgency tracking coffee or ovulation.
This is not busywork; it’s a map. With my wife, that timeline ended arguments with ourselves about “is it real today?” It showed us Tuesday mornings were danger zones after late Mondays.
Bring the log to appointments. You’re not guessing anymore; you’re showing a story in time. That’s how you earn targeted testing, not scattershot trials that drain hope and money.
Screen Early: Gut, Bladder, Migraine
Don’t wait for symptoms to “get bad enough.” Ask directly about IBS traits (pain that eases after a bowel movement, bloating, stool changes), bladder pain features (urgency, frequency, pain easing after voiding), and migraine patterns (one-sided throbbing, light sensitivity, nausea).
If boxes tick, request focused questionnaires or a referral. Early naming reduces fear.
With my wife, putting a name to the bladder pain softened the shame of bathroom maps and constant planning. It let us try pelvic floor therapy sooner instead of another round of painkillers that never touched urgency.
Screening isn’t labeling you forever; it’s opening doors. Once you identify neighbors to endometriosis, you can treat them in parallel, and sudden flares feel less like chaos and more like levers you can adjust.
Ask About Dizziness and POTS-Like Signs
If standing makes your heart race, if showers or hot rooms knock you flat, if brain fog blooms after small exertion, tell your clinician clearly. Note pulse changes from lying to standing, new palpitations, near-faints, and salt cravings.
We learned to measure heart rate at home and record it beside symptoms.
Simple supports, slow position changes, fluids, salty snacks if appropriate, compression tights, can change mornings. For my wife, cooling the bedroom and pacing chores cut those “I might pass out” spikes.
If patterns persist, ask about dysautonomia assessment. Even when it’s not formal POTS, autonomic fragility is common with chronic pain and poor sleep. Naming it guides kinder routines and prevents the spiral where fear of dizziness causes more deconditioning and worse symptoms.
Check Thyroid and Autoimmune Panels
Thyroid swings mimic everything: fatigue, hair changes, mood dips, palpitations, bowel slowdowns. Autoimmune screens can flag conditions like thyroiditis that often travel with allergic tendencies.
Ask for a sensible panel when symptoms fit, not a fishing expedition. Share family history and your timeline so testing is justified.
When my wife’s low-grade exhaustion refused to lift, checking thyroid and ferritin gave us solid ground. Correcting deficiencies didn’t cure endometriosis, but it raised the floor we stood on.
Results also shape safer choices in surgery, hormones, and pregnancy planning. Clarity beats guesswork. Even normal labs are useful; they let you focus on what’s actually driving pain rather than chasing ghosts.
Protect Sleep as Core Therapy
Sleep is not a luxury line item; it’s pain processing, hormone balance, and memory repair. Start with rhythm: consistent wake time, light in the morning, screens down before bed, and a cooler, darker room.
Treat pain before bedtime, not after you’re desperate. Guard naps so they help, not hijack the night.
For us, earlier dinners, warm showers, and a tiny wind-down routine softened the edges of flares. On bad weeks, dividing the night, her first stretch alone, my quiet check-in at two made mornings gentler.
If insomnia bites hard, ask about cognitive behavioral strategies and whether meds are worsening sleep architecture. Each percent of better sleep lowers pain reactivity; it’s the cheapest anti-inflammatory you have.
Liveable Anti-Inflammatory Daily Routine
Grand overhauls collapse; choose small changes you can repeat. Anchor meals around colorful plants, omega-3s, gentle protein, and steady fibers your gut tolerates.
Test triggers one at a time, not ten. Hydrate. Move most days, even if it’s five minutes and a stretch.
We built a rotation of calm breakfasts and freezer-friendly dinners, so flares didn’t mean chaos. On high-pain days, we shrink portions of life, not nutrition.
Supplements should be chosen for a reason, tracked for effect, and pruned if they do nothing. The goal isn’t perfection; it’s lowering inflammatory noise so treatments and sleep can work. Habits that survive real life beat elaborate plans abandoned by Thursday.
Coordinate Truly Multidisciplinary Care
One clinician can’t hold the whole picture. Invite gynecology, gastro or urology, pelvic physio, pain, and mental health into the same conversation, even if you are the bridge.
Share your one-page timeline and your goals for the next three months. Ask each specialist how their plan fits with the others.
When we aligned pelvic floor therapy with bowel care and sleep work, pain shrank on more days than it surged. That wasn’t magic; it was fewer mixed messages to a nervous system already on edge.
Coordination prevents drug interactions, duplicated tests, and burnout. It also builds trust, because everyone is rowing the same direction: function, dignity, and steadier days.
Plan Fertility, Menopause, Bone-Heart
Think ahead even while managing today. If fertility is a hope, ask early about options and timelines so surgeries and medications support that path.
If hormones are part of care, discuss bones, lipids, and mood in the same breath; prevention is lighter than repair.
We keep a simple calendar: scans when due, vitamin D checks, exercise we actually do, and questions to raise before any change.
Planning doesn’t force choices; it protects them. When menopause questions arrive, naturally or surgically, you’ll decide with context, balancing pain control with long-term strength, rather than sprinting through decisions in the fog of a flare.
Build Compassionate, Flexible Work-Life
Health needs room. If you can, reshape work to match energy: later starts, remote options, batch tasks on good days, buffer meetings with breathers.
At home, create quiet corners, go-bags for appointments, and permission to cancel without guilt. Love is logistics; it reduces friction so tenderness can breathe.
Our home office wasn’t just décor; it was safety. She could rest between tasks, dim the lights when headaches crept in, and still keep her sense of purpose.
Flexibility is not weakness; it’s a strategy. When life flexes, flares don’t automatically steal meaning. That steadiness becomes its own medicine, for both of you.
More on Comorbidities of Endometriosis
What I wish someone had told us early on is that the body keeps score in clusters: pelvic pain rarely sits alone; it travels with gut urgency, bladder burning, migraine, poor sleep, and a nervous system on edge. Large reviews and guidelines now frame endometriosis as a chronic inflammatory disease, which helps explain these overlaps and why single-organ fixes often fall short.
Population studies repeatedly show higher odds of IBS and bladder pain syndrome/interstitial cystitis in those with endometriosis, pain and urgency easing after voiding, bloating that swells with the cycle, and bowel habits that swing in step with hormones.
Headache disorders, especially migraine, are also enriched; data-driven analyses and clinical cohorts confirm the pattern, reminding us that trigeminal pain and pelvic pain can be different faces of the same inflamed circuitry.
Autoimmune and allergic tendencies (thyroiditis, asthma, eczema) show up more often too, echoing the immune dysregulation seen in lesions and blood—another reason to screen wisely rather than dismiss “too many symptoms.”
There are debated but important long-term signals: some studies suggest increased relative risk of certain ovarian cancers (though absolute risk stays low), which calls for nuanced counseling rather than fear.
Fresh research also flags earlier menopause, especially surgical menopause linked to treatment decisions, so bone, heart, and cognitive health should be part of the conversation from the start.
When clinicians connect these threads, plans change: gastro and urology input arrives sooner, pelvic physio isn’t an afterthought, migraine prevention gets tailored, and sleep is protected like a prescription.
This is why I talk about comorbidities of endometriosis as core to management, not side notes; if we treat the satellites, the planet calms.
In our home, naming the bladder pain stopped the shame of mapping toilets; spotting the migraine–sleep link cut ER visits; and pacing mornings softened those dizzy, fast-pulse moments that once felt like failure.
What looked like chaos became a map: fewer mixed messages to a sensitized nervous system, more days where she could work from our quiet office, cook a simple meal, and still have energy to laugh.
That’s the power of pattern-spotting and team care, less heroic willpower, more aligned biology.
It doesn’t make the condition easy; it makes it understandable, and that’s the first step toward kinder, smarter control.
Living with the Comorbidities of Endometriosis
Some mornings begin with quiet hope and a plan, then a single trigger topples the bridge between us and the day. Pelvic pain nudges the gut, the gut provokes the bladder, and soon sleep debt and headache join the queue. I have learned to read that chain and respond in order, not in panic.
When my wife’s energy dips, I slow the home first: dimmer lights, softer tasks, shorter to-do lists. Breakfast shifts to what her body trusts, and I guard her meds and heat pack like anchors. Kind logistics make room for courage.
By noon, I check the signals that often go ignored. If she is dizzy on standing, we pace chores, add fluids, and keep the room cool. If urgency rises, we map breaks into everything so her day feels possible, not punished.
Afternoons are our decision point. Do we push or pivot? Pushing used to cost us tomorrow, so now we ask what small win keeps dignity intact without borrowing from the next day.
I carry a quiet grief for the life we planned, and a louder gratitude for the one we’ve built. She carries pain I cannot feel, and I carry the world around it so it weighs less. That is how we meet in the middle.
Evenings belong to recovery. We prepare calm food, line up sleep rituals, and agree that rest is progress, not retreat. When fear of the night creeps in, I remind her that better sleep is treatment, not a treat.
On appointment weeks, I become her translator and witness. I bring timelines, questions, and what actually helped, so each clinician sees the whole picture. Good care multiplies when stories are clear.
Work bends to health because love gave us that choice. Our home office is not just a desk; it is safety, light control, and a door that closes when a migraine whispers. Purpose survives because the environment protects it.
I keep my own steadiness on purpose. I lift, cook, plan, and listen, but I also breathe and step outside when I need to reset. Caring works best when the carer is not running on fumes.
On the rare easy days, we don’t sprint. We savor them, bank gentle movement, and leave a little energy unspent so tomorrow has a chance. Progress is not dramatic; it is earned in ordinary hours.
Final Word on the Comorbidities of Endometriosis
What I have learned, standing beside my wife through years of flares, scans, sleepless nights, and small victories, is that clarity is a form of care. Names matter because they turn chaos into a map.
Pelvic pain that echoes into the gut, a bladder that shouts at the wrong time, headaches that dim a day, anxiety that grows in the dark, these are not random visitors. They are signals that the body is trying to coordinate more than one battle at once. When we treat each signal in isolation, we miss the choir. When we step back and listen for themes, real progress begins.
Our turning point was deceptively simple. We tracked symptoms on one page and brought that page to every appointment. Patterns emerged. Pain and sleeplessness talked to each other. Certain foods were fine on calm weeks but unhelpful during hormonal peaks.
Hydration, pacing, and pelvic floor therapy worked better when we protected sleep first. Once we could show time-anchored evidence, clinicians responded with targeted plans rather than generic advice. That lifted our hope, which lifted our effort, which lifted her days.
Kind logistics have been medicine. A home office that dims when a migraine whispers. Meals that are calm and repeatable.
A morning routine that starts slowly if dizziness greets us at the door. Short walks that steady the nervous system without stealing tomorrow. These are not extras. They are the practical architecture of dignity. They let treatments land, and they give love somewhere to live on hard mornings.
I learned to ask different questions. Not only what is wrong, but what is helping, even a little. Not only what should be removed, but what should be protected. We protected sleep and the right to cancel. We protected protein and hydration on flare days. We protected the truth that progress often looks like fewer crashes, not zero pain. That truth kept us steady when the calendar said we should be further along.
There is room here for science and softness at the same time. Evidence informs the plan. Story sustains it. You deserve both. If you are reading this in the middle of your own storm, take one small step that reduces friction today. Note one pattern. Ask for one referral that fits your map.
Place one gentle habit where it can survive real life. Then measure the day in ordinary moments, a laugh during dinner, a morning with a little less fear, the walk that did not cost the next day. This is how healing feels when it is honest, not dramatic, and it is enough to keep going.
You are not broken; you are managing a complex set of signals that deserve a coordinated plan. Map patterns, protect sleep, simplify food, hydrate, pace activity, and bring a single clear page to every appointment. Small, repeatable choices reduce noise so treatment can work and hope can breathe.
Have a question or a story to share? Leave a comment below, and if endometriosis is part of your life, grab a free chapter of my “Endo-Tool: Endometriosis for Men.” You will also join our community for more freebies, big book discounts, and real help for your new normal.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MOREComorbidities of Endometriosis FAQs
1) What conditions most often occur alongside endometriosis?
The most frequently reported companions include irritable bowel syndrome (IBS), bladder pain syndrome/interstitial cystitis, migraine, anxiety and depression, allergic/atopic tendencies, and autoimmune thyroid disease. Some patients also report features of dysautonomia (like POTS-like symptoms) and widespread pain consistent with fibromyalgia. These aren’t random add-ons; they share inflammatory, hormonal, and neuro-immune pathways. Naming them early helps you treat in parallel rather than chasing symptoms one by one.
2) How do I tell an endometriosis flare from IBS or bladder pain—and can endometriosis cause ulcerative colitis?
Endometriosis pain often tracks the cycle and may radiate to the back or legs; IBS adds bowel habit change and pain eased by a bowel movement; bladder pain syndrome causes urgency/frequency that improves after voiding. They can overlap on the same day, which is why a single timeline is powerful. Endometriosis doesn’t cause ulcerative colitis, but the two can co-exist; persistent bleeding, weight loss, or night-time diarrhea warrants gastroenterology review. Imaging and targeted testing, not guesswork, should guide care.
3) Is there a connection between endometriosis, fibromyalgia, and POTS-like symptoms?
Yes—many people with endometriosis report widespread pain, fatigue, non-restorative sleep, and sensory sensitivity that mirror fibromyalgia biology (central sensitisation). A subset also experiences orthostatic intolerance—light-headedness, fast heart rate on standing, heat intolerance—suggesting dysautonomia. While mechanisms differ, chronic inflammation, pain amplification, sleep loss, and deconditioning can intertwine. Screening and gentle, staged strategies (hydration, salt as appropriate, compression, pacing) can stabilise mornings and make other therapies work better.
4) Are autoimmune conditions like Hashimoto’s or lupus linked to endometriosis?
Autoimmune thyroid disease (especially Hashimoto’s) and general atopy/allergy appear more common in those with endometriosis, and some studies note associations with systemic autoimmune disorders. Correlation isn’t destiny, but unexplained fatigue, palpitations, hair/skin changes, or temperature intolerance justify thyroid labs; rashes, joint swelling, mouth ulcers, or photosensitivity merit autoimmune screening. Clear results—positive or negative—help tailor hormones, surgery timing, pregnancy planning, and bone-heart monitoring.
5) Do lifestyle pivots really help—sleep, diet, and blood sugar?
They don’t replace medical care, but they lower “inflammatory noise” so treatment lands. Protecting sleep (regular schedule, darker/cooler room, analgesia before bed) measurably reduces pain reactivity. A calm, anti-inflammatory pattern—fibre you tolerate, omega-3s, steady protein, and mindful carbs to stabilise blood sugar—can soothe gut and energy swings; test changes one at a time. Add gentle, repeatable movement and stress-down tools; the goal is consistency, not perfection.
Comorbidities of Endometriosis References
- ESHRE guideline: endometriosis (2022) — full text (PMC)
- NICE guideline NG73: Endometriosis, diagnosis and management (last reviewed 2 September 2025)
- Unveiling endometriosis’s hidden comorbidities using a data-driven approach (Nature, 2025)
- The association between endometriosis and migraine (The Journal of Headache and Pain, 2025)
- A systematic review and meta-analysis of the comorbidities in endometriosis (2021)
- Burden of endometriosis: infertility, comorbidities, and costs (2022)
- Association of endometriosis with interstitial cystitis in chronic pelvic pain (2021)
- Living with endometriosis: comorbid pain disorders and quality of life (2022)
- Shared molecular genetic mechanisms underlie migraine and endometriosis (2020)
- Association between endometriosis and type and age of menopause, pooled cohort analysis (Human Reproduction, 2025)
- Endometriosis typology and ovarian cancer risk (JAMA, 2024) — full text (PMC)
- Endometriosis and comorbidities: molecular mechanisms and clinical implications (2025)