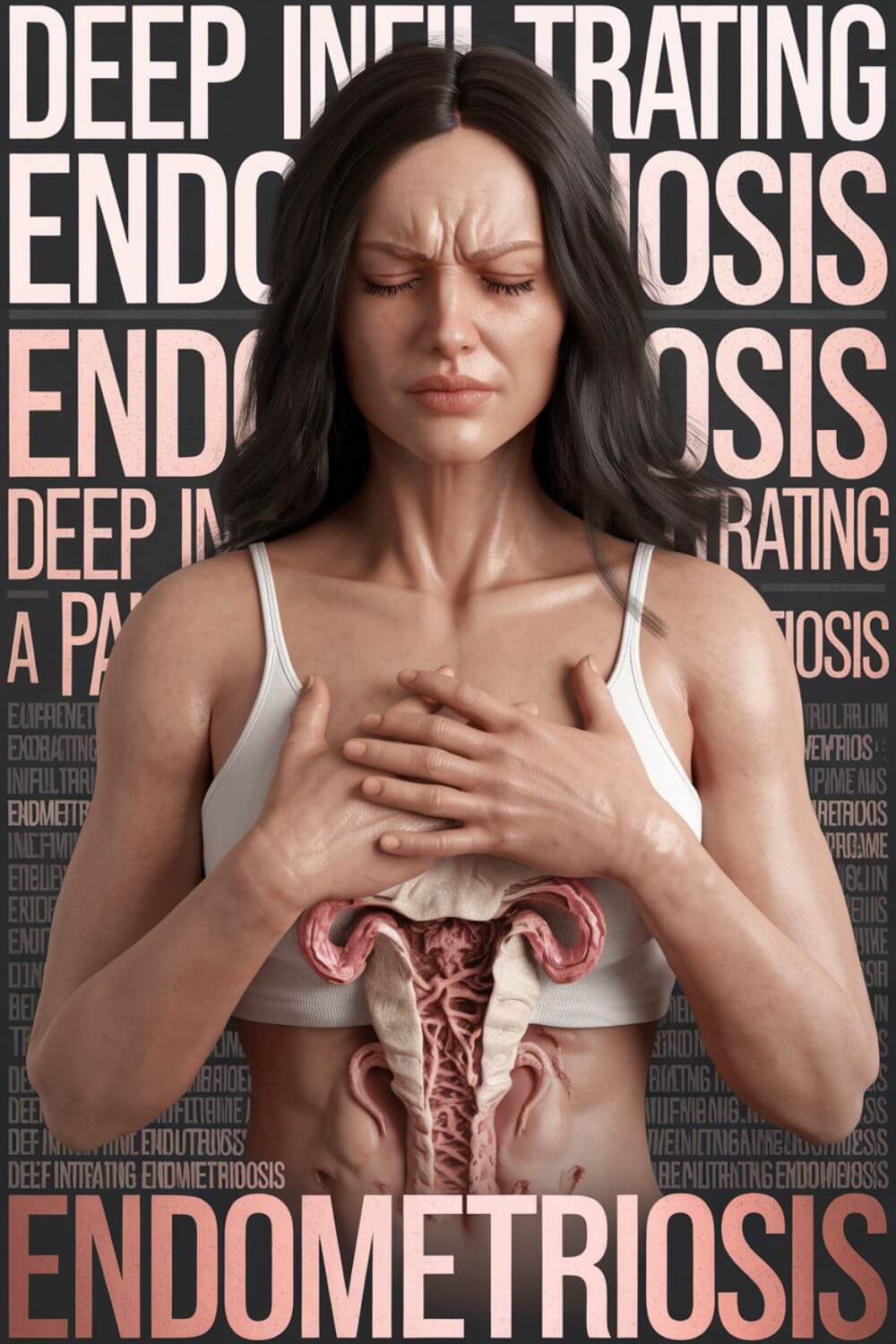
Deep Infiltrating Endometriosis (Updated 5th Dec 2024)
Deep infiltrating endometriosis (DIE) is one of the most severe forms of endometriosis, characterized by the invasion of endometrial-like tissue into organs and structures beyond the pelvic lining. This condition often leads to intense pain, infertility, and significant emotional and physical challenges.
When my wife was diagnosed with deep infiltrating endometriosis, it turned our world upside down.
Her stage IV endometriosis didn’t just affect her body—it reshaped her life, our relationship, and how we viewed the future. As her husband, I struggled to understand the depth of her pain and how to support her effectively. But I learned, slowly and painfully, that my role could be a lifeline for her—and that supporting her was a journey we had to take together.
What does deep infiltrating endometriosis mean for couples like us, and how can partners learn to navigate these uncharted waters together?
- Understanding My Wife’s Journey with Deep Infiltrating Endometriosis
- The Emotional Toll of Deep Infiltrating Endometriosis on Relationships
- Understanding Deep Infiltrating Endometriosis and Its Challenges
- Medical Insights into Deep Infiltrating Endometriosis
- More Medical Insights for Deep Infiltrating Endometriosis
- My Wife’s Battle with Adhesions and Endometriomas
- Repetitive Surgeries for Deep Infiltrating Endometriosis
- The Emotional Weight of Facing Repetitive Surgeries
- Conclusion on Deep Infiltrating Endometriosis
Understanding My Wife’s Journey with Deep Infiltrating Endometriosis
In 2012, shortly after marrying my wife, we received the life-altering diagnosis of deep infiltrating endometriosis. At the time, we barely understood what it meant. Her symptoms had been dismissed for years, chalked up to “normal” period pain. But when we finally learned it was stage IV, the most severe form, we were devastated. This wasn’t just a health condition; it was a force that infiltrated every aspect of her life.
My wife’s endometriosis wasn’t limited to her reproductive system. It invaded her bowel, bladder, and nerves, causing debilitating pain that robbed her of her energy, her joy, and, at times, her will to keep going. She used to be a vibrant dancer, choreographer, and performer. Her career wasn’t just a job; it was her passion, her identity. Losing that part of herself to this disease was a grief I could see in her every day. She wasn’t just battling physical pain; she was mourning the life she’d lost.
Watching someone you love suffer like this is excruciating. As her husband, I felt helpless. There were no guidebooks or support groups for men like me. I didn’t know how to process the impact this had on my mental health or our relationship. But I realized that while I couldn’t take her pain away, I could be her steady foundation when the world felt like it was crumbling around her. This realization became my anchor in the storm.
How Can the Endo-Tool Help Partners Navigate DIE?
When I first began supporting my wife through her battle with deep infiltrating endometriosis, I often felt lost, overwhelmed, and isolated. There was no roadmap to follow, no clear answers to the countless questions I had as a husband. How do I help her manage her pain? How do I navigate the emotional toll on our relationship? How do I cope with my own mental health challenges while being her anchor?
This lack of guidance inspired me to create the Endo-Tool, a resource designed specifically for partners of women living with endometriosis. The Endo-Tool isn’t just a guide—it’s a lifeline for men who, like me, are navigating this journey without a manual. It’s built on my years of personal experience, research, and hard-earned lessons as a husband who has walked this path.
With the Endo-Tool, you’ll find:
- Practical Advice: Learn how to support your partner during flare-ups, manage daily challenges, and advocate for her needs in medical settings.
- Emotional Insights: Understand the mental and emotional toll that endometriosis takes on both of you, and how to strengthen your relationship despite the hardships.
- Personal Stories: Relatable experiences that remind you that you’re not alone in this journey.
- Actionable Tips: Step-by-step strategies to help you cope, communicate, and thrive together as a couple.
If you’re a woman reading this, imagine how much your partner could benefit from having a resource like this. It’s not just about helping men—it’s about creating a stronger, more supportive relationship for both of you.
Let the Endo-Tool guide you through the challenges of deep infiltrating endometriosis and help you and your partner rebuild hope, connection, and strength together.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men
The Emotional Toll of Deep Infiltrating Endometriosis on Relationships
When my wife was diagnosed with deep infiltrating endometriosis, I thought the hardest part would be the physical pain she endured. I quickly learned, however, that the emotional and relational challenges were just as significant—and, in some ways, even more difficult to navigate. This disease doesn’t just affect the person who has it; it ripples through the relationship, testing love, patience, and resilience in ways I never imagined.
As her husband, I’ve witnessed firsthand how endometriosis can rob someone of their self-esteem, their dreams, and their hope. My wife often feels like a burden—a sentiment that breaks my heart every time she expresses it. She’s asked me, more than once, to leave her, believing I’d be better off with someone healthy who could give me children and a “normal” life. Those moments were some of the hardest for me because no amount of reassurance seemed to ease her guilt or self-doubt.
I won’t sugarcoat it—this journey has been incredibly hard. But through the pain and challenges, I’ve learned the power of showing up. Just being there for her, loving her unconditionally, and letting her know she isn’t alone has been the most impactful thing I can do. It’s not always about fixing the problem; sometimes, it’s simply about being present and steady in the face of the storm.
Have you ever wondered how much stronger your relationship could become if both partners understood how to navigate the emotional toll of endometriosis together?
Understanding Deep Infiltrating Endometriosis and Its Challenges
Deep infiltrating endometriosis is one of the most complex and debilitating forms of the condition, impacting not just physical health but every aspect of life. For women, it’s a constant battle with chronic pain, fatigue, and emotional upheaval. For their partners, like me, it brings an entirely different set of challenges—ones we often face silently.
Endometriosis doesn’t just attack the body; it strains relationships, careers, and even self-identity. For my wife, it took away her passion for dance, leaving her to grieve not only her health but the life she once dreamed of. As her husband, I had to learn how to be her rock when it felt like the ground beneath us was constantly shifting.
Why Supporting Men Matters in Endometriosis?
When my wife was diagnosed with deep infiltrating endometriosis, I found that the world was full of resources for her—but there was almost nothing for me. Men in these situations often feel invisible, left to navigate a deeply emotional and complex journey without guidance or support.
That’s why I’ve dedicated myself to helping other men in similar situations. Supporting the men who care for women with endometriosis isn’t just about helping them cope—it’s about strengthening relationships. When we equip men with the tools to better understand and support their partners, we create a ripple effect that benefits both individuals and their relationship as a whole.
The Ripple Effect of Endometriosis on Couples
1. Chronic Pain and Emotional Strain
Living with a partner who has chronic pain means witnessing their struggle daily. It’s heartbreaking to see someone you love suffer, especially when you can’t fix it. This can lead to feelings of helplessness and frustration in both partners.
2. Loss of Intimacy and Connection
Endometriosis often impacts physical intimacy due to pain and fatigue. For many couples, this becomes a source of tension and misunderstanding, highlighting the need for open communication and empathy.
3. Mental Health Challenges
The emotional toll of endometriosis affects both partners. My wife battles depression and anxiety, and I’ve faced my own struggles with stress and burnout. Supporting her has taught me the importance of prioritizing mental health—for both of us.
4. Navigating New Normals
Adjusting to life with endometriosis requires redefining what “normal” looks like. It’s about finding ways to adapt, support each other, and create a life that acknowledges the challenges without being defined by them.
5. Building Resilience Together
Through every setback, we’ve learned to lean on each other and grow stronger as a team. Resilience doesn’t mean pretending everything is fine—it means facing the hard days together and celebrating the small victories along the way.
What Partners Need to Know About Deep Infiltrating Endometriosis?
When I first heard the term deep infiltrating endometriosis, I couldn’t fully grasp its complexity or the profound impact it would have on our lives. Over time, I’ve come to understand that the key to navigating this journey lies in patience, empathy, and a willingness to learn.
If you’re a woman reading this, I encourage you to share these insights with your partner. And if you’re a man like me, know that you’re not alone. With the right tools and support, it’s possible to not only survive this journey but to find moments of joy, connection, and hope along the way.
Medical Insights into Deep Infiltrating Endometriosis
Understanding deep infiltrating endometriosis (DIE) requires a closer look at its medical classifications, including stages and types. These distinctions provide insight into the severity of the condition and the ways it can affect the body. For partners and loved ones, understanding these medical details can foster greater empathy and more informed support.
Stages of Endometriosis
Endometriosis is classified into four stages by the American Society of Reproductive Medicine (ASRM):
- Stage I (Minimal)
- Small lesions and minimal scar tissue (adhesions).
- Limited to the surface of pelvic organs.
- Stage II (Mild)
- More lesions and shallow implants.
- Minimal involvement of deeper tissues.
- Stage III (Moderate)
- Deeper implants and more extensive adhesions.
- Ovaries may have endometriomas (also known as “chocolate cysts”).
- Stage IV (Severe)
- The most advanced stage, with widespread deep implants.
- Large endometriomas and extensive adhesions affecting multiple organs.
Deep infiltrating endometriosis, a hallmark of Stage IV, involves tissue growing deeply into organs, often beyond the reproductive system.
Types of Deep Infiltrating Endometriosis
Deep infiltrating endometriosis (DIE) is a specific form of endometriosis distinguished by the depth of invasion—typically more than 5 millimeters below the surface. This type can severely impact various organs and structures, including:
- Rectovaginal Endometriosis
- Involves the area between the rectum and vagina.
- Can cause painful bowel movements, constipation, or diarrhea during menstruation.
- Bladder Endometriosis
- Affects the urinary bladder.
- Symptoms include frequent urination, painful urination, or blood in urine.
- Intestinal Endometriosis
- Affects the intestines, often the sigmoid colon or rectum.
- Leads to severe gastrointestinal symptoms like bloating, pain, and altered bowel habits.
- Pelvic Endometriosis
- Spreads deeply into the pelvic cavity, involving ligaments, nerves, or muscles.
- Can lead to pelvic pain, nerve pain, and reduced mobility.
- Thoracic Endometriosis
- Rarely, endometrial tissue can reach the diaphragm or lungs.
- May cause chest pain or difficulty breathing, especially during menstruation.
Why Understanding These Details Matters?
When my wife was diagnosed with Stage IV deep infiltrating endometriosis, understanding the stage and type of her condition helped me grasp the magnitude of her pain and the complexities of her treatment. Each stage and type of endometriosis brings unique challenges, and knowing these details has been crucial in advocating for her care and offering the right kind of support.
As partners, we might not feel the pain directly, but understanding the medical intricacies allows us to share in the burden and approach this journey with more knowledge, patience, and compassion.
If your partner has deep infiltrating endometriosis, learning about its stages and types is a vital first step in becoming a more informed and supportive ally.
More Medical Insights for Deep Infiltrating Endometriosis
To truly grasp the impact of deep infiltrating endometriosis (DIE), it’s essential to explore the medical aspects in more detail. This severe form of endometriosis not only causes intense physical pain but also profoundly affects overall health, making medical understanding key to offering effective support.
How Deep Infiltrating Endometriosis Develops?
Endometriosis occurs when tissue similar to the uterine lining (endometrium) grows outside the uterus. In deep infiltrating endometriosis, these tissues invade structures deeper than 5 millimeters, leading to chronic inflammation, adhesions, and scarring. Over time, these lesions can impact the function of affected organs and contribute to significant pain and complications.
Organs Commonly Affected
- Uterus and Ovaries
- Adhesions may distort the reproductive organs, leading to infertility.
- Ovarian cysts (endometriomas) often develop, filled with old, dark blood.
- Bowel and Rectum
- Deep infiltrating endometriosis often invades the bowel, leading to pain during bowel movements, bloating, and even partial obstructions.
- Severe cases may require bowel resection surgery.
- Bladder and Ureters
- Endometrial lesions in the bladder cause urinary symptoms like urgency, pain, and even blood in the urine.
- In rare cases, ureteral endometriosis can lead to kidney damage if untreated.
- Pelvic Nerves
- Lesions can infiltrate pelvic nerves, causing neuropathic pain, numbness, or weakness in the legs.
- Nerve involvement often leads to misdiagnoses, delaying proper treatment.
- Diaphragm and Lungs
- While rare, endometriosis can affect the diaphragm and even the lungs, causing chest pain, shortness of breath, and other respiratory symptoms during menstruation.
Symptoms of Deep Infiltrating Endometriosis
While symptoms vary, common signs of DIE include:
- Chronic Pelvic Pain: Often severe and unrelenting, especially during menstruation.
- Painful Intercourse: Caused by deep lesions in the pelvic cavity.
- Heavy Menstrual Bleeding: Often accompanied by anemia.
- Bowel and Bladder Issues: Painful bowel movements, frequent urination, and bloating.
- Fatigue: Chronic inflammation and pain contribute to debilitating fatigue.
Diagnostic Challenges
Diagnosing deep infiltrating endometriosis is notoriously difficult. Many women, including my wife, suffer for years before receiving a proper diagnosis. Common diagnostic tools include:
- Ultrasound and MRI
- Specialized imaging can detect larger lesions and cysts.
- Laparoscopy
- A surgical procedure that allows direct visualization and biopsy of lesions.
- This is the gold standard for diagnosing DIE.
Treatment Options for Deep Infiltrating Endometriosis
- Medications
- Hormonal treatments, such as birth control pills, progestins, or GnRH agonists, can suppress the growth of endometrial tissue.
- Pain relief medications, including NSAIDs and neuropathic agents, address symptoms but don’t treat the disease.
- Surgery
- Excision surgery is the most effective treatment for deep infiltrating endometriosis, involving the removal of lesions and adhesions.
- For severe bowel or bladder involvement, specialized surgeons may perform complex procedures, such as bowel resection or bladder reconstruction.
- Lifestyle Changes
- Anti-inflammatory diets, physical therapy, and stress management can complement medical treatments.
- My wife has found some relief through dietary changes and mindfulness practices, though these are not substitutes for medical care.
- Fertility Treatments
- For women facing infertility due to endometriosis, options like IVF may be necessary.
The Importance of Early Intervention
Deep infiltrating endometriosis is a progressive condition. Early diagnosis and treatment are crucial to managing symptoms and preventing severe complications. However, many women face delays in diagnosis due to the normalization of symptoms or misdiagnosis.
As a husband, learning about these medical aspects has not only helped me understand my wife’s condition better but has also enabled me to advocate for her care. Knowing the science behind her struggles allows me to stand by her side more effectively, whether during medical appointments or on the toughest days.
Deep infiltrating endometriosis is a complex condition, but with the right information and support, it’s possible to navigate its challenges together.
My Wife’s Battle with Adhesions and Endometriomas
Deep infiltrating endometriosis is a disease of layers—not only does it invade tissues deeply, but it also creates a web of complications that disrupt the body’s natural anatomy. My wife’s case has been particularly severe, and her experience highlights the profound impact this condition can have on the internal structures of the body.
Understanding Adhesions and Their Impact
Adhesions are bands of scar tissue that develop as a result of chronic inflammation caused by endometriosis. In my wife’s case, these adhesions have formed extensively, binding organs together in ways they were never meant to be.
- Ovary Stuck to the Uterus:
One of the most challenging issues my wife faces is that her left ovary is adhered to her uterus. This abnormal connection causes immense pain, particularly during ovulation and menstruation, when the ovary is most active. The pulling and stretching of these adhesions create a sensation she describes as being “torn apart” internally. - Impact on Mobility and Function:
Adhesions don’t just cause pain—they can limit the normal movement of organs, affecting bodily functions like digestion, urination, and even posture.
Endometriomas: Chronic Pain and Inflammation
Endometriomas, often called “chocolate cysts,” are fluid-filled cysts that develop on the ovaries due to endometriosis. My wife has not one but four endometriomas, which add another layer of complexity to her condition.
- Formation of Endometriomas:
These cysts are filled with old blood, giving them their characteristic name. Over time, they grow larger, increasing pressure on the ovaries and surrounding tissues. - Symptoms Caused by Endometriomas:
The presence of these cysts contributes to:- Chronic pelvic pain.
- Heaviness and bloating.
- Hormonal imbalances due to their impact on ovarian function.
- Risk of Rupture:
Endometriomas can rupture, releasing their contents into the pelvic cavity. This can cause sudden, excruciating pain and requires immediate medical attention.
How Deep Infiltrating Endometriosis Complicates Treatment?
For my wife, surgery has been both a diagnostic and therapeutic tool. During her most recent procedure, the surgeon discovered the full extent of the adhesions and the involvement of her organs. These findings included:
- Adhesions tethering her bowel to her pelvic wall.
- Endometriomas that had grown significantly, requiring careful excision to preserve ovarian function.
- Extensive scar tissue that needed to be removed to restore some degree of normal anatomy.
However, excision surgery is not a cure. The adhesions often return, and the endometriomas can reappear. It’s a constant cycle that requires vigilance, ongoing medical care, and, above all, resilience.
The Emotional and Physical Toll
Seeing my wife go through this has been heartbreaking. The pain she feels is not just physical—it’s emotional. She mourns the loss of her mobility, her freedom, and the ability to plan her life without the constant interference of this disease.
As her husband, I’ve learned to offer support in every way I can—whether that’s being by her side during medical appointments, helping her track symptoms, or simply holding her hand on the hard days. Understanding the medical realities of her condition has made me a better advocate and partner.
For partners of women with deep infiltrating endometriosis, learning about adhesions and endometriomas isn’t just about medical knowledge—it’s about empathy. These details help us see the invisible battles our loved ones are fighting and remind us to be their strongest allies.
Repetitive Surgeries for Deep Infiltrating Endometriosis
Surgery is often seen as a lifeline for women with deep infiltrating endometriosis, but it’s not always a straightforward solution. My wife’s journey highlights the difficult realities of repetitive surgeries, including the physical and emotional toll they take. Her first surgery left her with complications that have made her afraid of undergoing a second one—a fear I completely understand and share.
The Reality of Her First Surgery
When my wife underwent her first excision surgery, we were hopeful it would provide relief. Instead, it introduced complications that worsened her situation:
- Adhesions:
The surgery caused extensive scar tissue to develop. Adhesions formed, binding her left ovary to her uterus and limiting the natural movement of her organs. These adhesions are now a source of chronic pain and discomfort that impacts her daily life. - No Lasting Relief:
Despite the invasive procedure, her pain persisted. The same symptoms that brought her to surgery—severe pelvic pain, bowel discomfort, and fatigue—returned within months. - Emotional Impact:
The failure of the first surgery left her disillusioned and emotionally drained. The hope we had invested in that operation made the disappointment even harder to bear.
Why She Fears a Second Surgery?
Now, faced with the possibility of a second surgery, my wife is understandably terrified. The fear stems from:
- Worsening Adhesions:
Adhesions caused by the first surgery have already altered her anatomy and increased her pain. Another surgery could create new adhesions, compounding the problem. - Uncertainty:
There’s no guarantee that a second surgery will help. The risk of recurring symptoms and complications makes the decision feel like a gamble. - Emotional Trauma:
The thought of reliving the aftermath of her first surgery—physically, emotionally, and mentally—is overwhelming.
Is It Worth Repeating?
This is the question we ask ourselves every day. On one hand, surgery is often the only way to remove deep endometriosis lesions and address complications like endometriomas or severe adhesions. On the other, the risks are significant, and the results are unpredictable.
When considering another surgery, we’ve learned to weigh the following factors:
- The Surgeon’s Expertise:
Not all surgeons are equally skilled in dealing with deep infiltrating endometriosis. Finding a specialist with extensive experience in excision surgery is critical to improving outcomes. - Extent of the Disease:
If the endometriosis is causing severe organ damage or impacting basic functions like urination, bowel movements, or fertility, surgery may be unavoidable. - Alternative Treatments:
We’ve explored other options, including hormonal therapies, pain management strategies, and lifestyle adjustments, to delay or avoid another surgery. - Long-Term Goals:
Is the goal to manage symptoms, improve quality of life, or address specific complications? Understanding these goals helps guide the decision.
Balancing Risks and Hope
As her husband, I struggle with this decision too. I want her to find relief and reclaim some normalcy in her life, but I also fear seeing her go through the same disappointment and pain again. Every day, I remind her that this is her decision to make. My role is to support her, no matter what path she chooses.
For now, we’re focusing on gathering as much information as possible, consulting with specialists, and carefully weighing the risks and benefits. It’s not an easy journey, but it’s one we’re facing together.
If you or your partner are considering repetitive surgeries for deep infiltrating endometriosis, know that your fears and doubts are valid. The decision is deeply personal, and it’s okay to take your time to find what feels right for you.
The Emotional Weight of Facing Repetitive Surgeries
Repetitive surgeries for deep infiltrating endometriosis aren’t just medical procedures—they’re deeply emotional decisions that can shape a person’s quality of life and their hope for the future. For my wife, the prospect of a second surgery is fraught with fear and uncertainty, largely because of her experience with the first one.
Surgery as a Double-Edged Sword
When my wife underwent her first surgery, we hoped it would offer relief, a chance to regain some of the life endometriosis had taken from her. Instead, it left her with complications: adhesions that caused her left ovary to stick to her uterus, increased pain, and the heart-wrenching realization that the surgery didn’t help as we had hoped.
This is the cruel reality of endometriosis surgeries—sometimes they do more harm than good. Scar tissue (adhesions) is a common side effect, especially when surgery is performed by a less experienced surgeon or when the body reacts unpredictably to the trauma of the procedure.
How does the Past Shape the Future?
Now, as we consider a second surgery, my wife’s fears are entirely justified:
- Will It Happen Again?
She’s terrified that this surgery might worsen her adhesions or create new complications. The idea of enduring more pain is almost unbearable for her. - Is It Worth the Risk?
The first surgery didn’t provide lasting relief. The thought of undergoing another invasive procedure, with no guarantee of success, weighs heavily on her mind. - The Emotional Scars
The first surgery left her feeling betrayed—not just by the procedure, but by her body and the healthcare system. The emotional toll of hoping for relief and finding more pain is something she’s still healing from.
Seeking Clarity and Hope
To make an informed decision, we’ve focused on a few key steps:
- Finding the Right Surgeon
A highly skilled excision specialist makes all the difference. We’ve learned that not all surgeons are equipped to handle deep infiltrating endometriosis with the precision and care it requires. - Understanding the Risks
We ask hard questions about adhesions, organ involvement, and the likelihood of complications. Knowing the risks doesn’t eliminate the fear, but it helps us prepare. - Exploring Alternatives
Before committing to surgery, we’ve sought out alternative treatments—hormonal therapies, pain management techniques, and dietary changes—to see if they can offer relief without the need for another procedure. - Balancing Risks with Quality of Life
We’ve talked about what she wants to achieve with this surgery. Is it relief from pain, better mobility, or addressing a specific complication? These goals help frame the decision.
My Role as Her Husband
As her partner, this decision is one I support but cannot make for her. My job is to be her advocate and her rock, to listen when she voices her fears and to remind her that her feelings are valid. Watching someone you love face a decision like this is gut-wrenching, but I’ve learned that my presence and patience are the best gifts I can offer.
For any partner reading this, I want you to know how crucial your role is. It’s not about giving answers—it’s about walking beside your loved one as they navigate an incredibly difficult path.
Are repetitive surgeries for deep infiltrating endometriosis worth it? Only you and your partner can answer that question, but know that you’re not alone in facing it. Together, you can weigh the risks, explore the options, and make the best decision for your unique journey.
Conclusion on Deep Infiltrating Endometriosis
Deep infiltrating endometriosis is more than a medical condition—it’s a life-altering challenge that affects not just the woman suffering from it but also her relationships, mental health, and daily existence. For my wife and me, this journey has been filled with pain, fear, and countless unanswered questions. But it’s also been a journey of resilience, love, and learning to adapt to a new normal.
When my wife was first diagnosed, we were overwhelmed by the complexity of her condition. Her Stage IV deep infiltrating endometriosis came with adhesions that tethered her ovary to her uterus, four endometriomas, and debilitating pain that seemed to touch every aspect of her life. The first surgery we hoped would bring relief instead left her with more complications—new adhesions, persistent pain, and emotional scars that deepened her fear of further medical interventions.
Facing the possibility of repetitive surgeries has been one of the hardest decisions we’ve encountered. On one hand, the promise of relief is tempting. On the other, the risks of more adhesions, recurring pain, and disappointment make the decision deeply complex. For now, we’re focusing on finding the right specialists, exploring alternative treatments, and holding onto the hope that there’s a path forward, even if it’s not clear yet.
Through it all, I’ve learned that as a partner, my role isn’t to have all the answers—it’s to be there, unconditionally. I’ve learned to listen to her fears without dismissing them, to be her advocate in medical appointments, and to remind her of her incredible strength on days when she feels defeated.
Final Thoughts on DIE
Deep infiltrating endometriosis tests the limits of what a body and a relationship can endure. But it also shows us the power of love, understanding, and resilience. For any woman reading this, know that your partner’s support can make all the difference. And for the partners, I want you to know that you’re not alone. It’s okay to feel overwhelmed, to ask questions, and to take time to learn how best to support the woman you love.
Together, we can face this journey, one step at a time.
What are your thoughts on facing challenges like deep infiltrating endometriosis as a couple? Share your experiences in the comments below—I’d love to hear your story.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…