Impact of Endometriosis
What is the true impact of endometriosis on a woman’s life?
Endometriosis affects ~1 in 10 women worldwide; its impact spans chronic pain, infertility, fatigue, and mental-health strain, lowering quality of life and work productivity and imposing major economic costs. Earlier recognition, multidisciplinary care, and access to effective treatments reduce avoidable harm.
Beyond the headlines, studies show women lose hours each week to absenteeism and presenteeism, and households shoulder far more indirect than direct costs. Diagnostic delays remain common, compounding pain and financial stress. New options like linzagolix on the NHS widen choices but aren’t a cure.
I’ve watched my wife fight through days when pain steals her breath and nights when anxiety won’t let her rest, and I learned that love means becoming a student of this disease, not a bystander.
If endometriosis is part of your story, you can grab a free chapter of my book, “Endo-Tool: Endometriosis for Men.” In addition to joining us, you’ll also become part of our community where I share more freebies, big discounts on all our books, and practical, compassionate emails that help couples adjust to the new normal chronic illness brings.
The first chapter alone contains all the comprehensive medical knowledge about endometriosis, including:
- What is endometriosis?
- What are the symptoms?
- What causes endometriosis?
- What does endometriosis look like?
- What are the stages?
- What are the types?
- What is adenomyosis, and how is it related to endometriosis?
- Why do some women develop severe endo and others don’t?
- Does endometriosis cause infertility?
- How is endometriosis diagnosed?
- Do types and stages affect the treatment?
- Recurrence of endometriosis after excision surgery.
FREE Chapter of “Endo-Tool”
Endometriosis e-Book for Men

True Impact of Endometriosis
Pain doesn’t just live in the pelvis; it ripples through careers, relationships, and plans for the future, turning ordinary routines into obstacle courses. For many, quality of life drops sharply as pain, fatigue, and invasive symptoms stack up against limited treatment access and long diagnostic delays.
At work, the disease quietly drains hours. Studies across multiple countries show women lose around a day each week to absenteeism and, even more, to “presenteeism”, being at work but functioning through pain, which accounts for the majority of productivity loss. Those hidden losses add up to thousands per person each year.
Mental health rarely gets charted on clinic forms, yet depression, anxiety, and stress are consistently higher in those affected. The strain isn’t only biological; it’s the relentless uncertainty: when will the next flare hit, will a plan fall apart, will anyone believe me? Evidence continues to confirm the mind–body toll and the benefit of truly holistic care.
Fertility questions haunt many couples long before they start trying. The condition can obstruct anatomy and alter pelvic biology in ways that make conception harder, and even when surgery or medication helps with pain, choices must weigh future family goals. Emerging data continue to refine what improves outcomes and when.
Then there’s time, the years lost to referrals and misdiagnoses. In the UK, the average wait to get a name for this pain is still close to nine years, a delay that compounds physical symptoms, financial burden, and self-doubt. Every month without answers is another month of avoidable harm.
The economic picture is sobering. Beyond hospital bills, most of the cost sits in lost productivity, two-thirds or more in many analyses, dragging household budgets and career trajectories off course. This is not a “period problem”; it’s a public health and economic issue.
For us, these numbers are not abstract. I’ve watched my wife push through meetings with a brave smile, only to collapse afterward, and I’ve learned to build a life that flexes with her pain, work-from-home, slower mornings, backup plans, so we can still dream, travel, and protect joy.
As you read on, I’ll share what helped us turn chaos into a kinder rhythm, simple, evidence-led shifts you can try today.
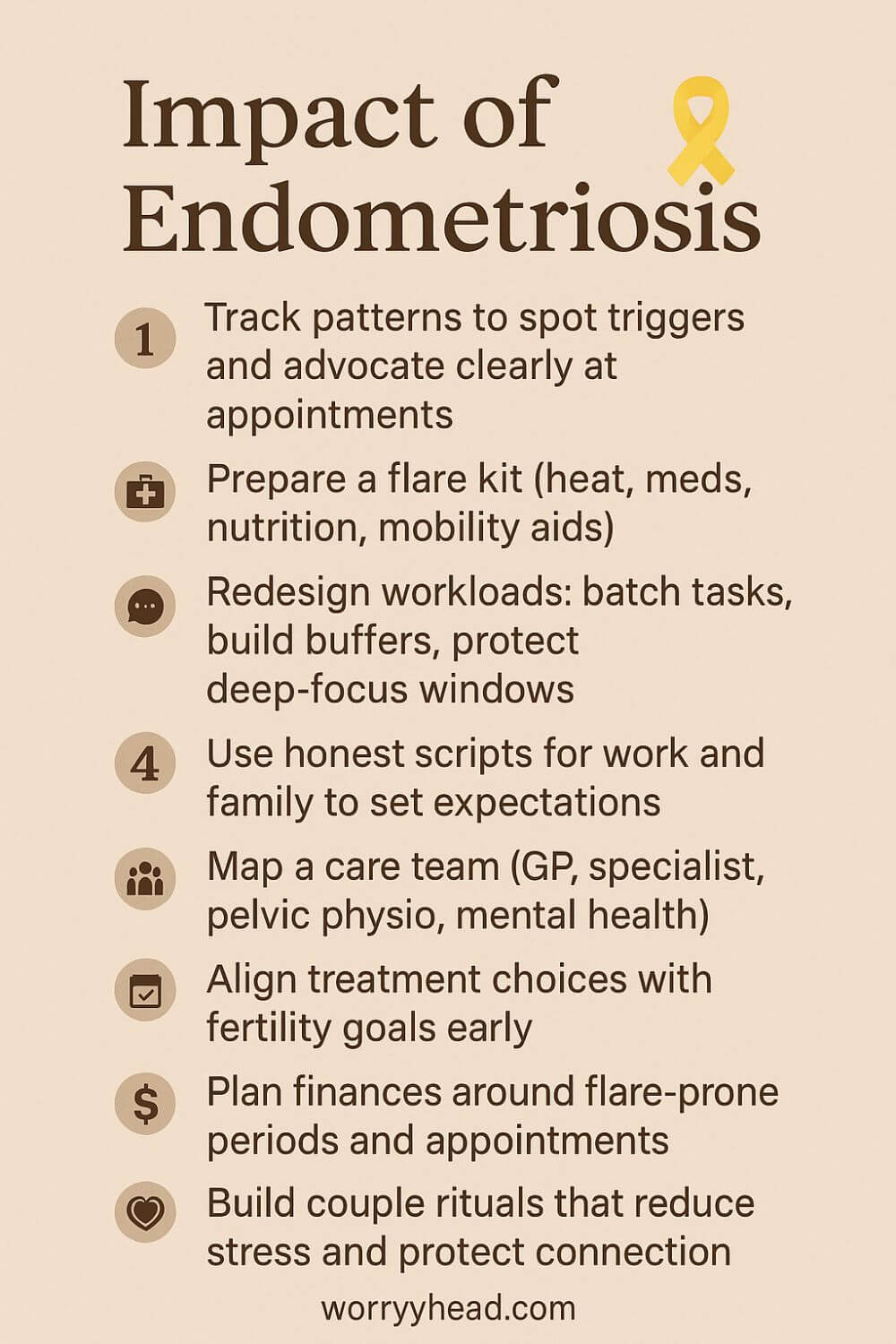
- Track patterns to spot triggers and advocate clearly at appointments
- Prepare a flare kit (heat, meds, nutrition, mobility aids)
- Redesign workloads: batch tasks, build buffers, protect deep-focus windows
- Use honest scripts for work and family to set expectations
- Map a care team (GP, specialist, pelvic physio, mental health)
- Align treatment choices with fertility goals early
- Plan finances around flare-prone periods and appointments
- Build rituals that reduce stress and protect the connection
Track Patterns to Spot Triggers
Start with a simple log you can keep during real life, not just perfect weeks. Note pain level, bleeding, sleep, food, stress, movement, sex, bowel or bladder changes, meds, and what helped. Patterns rarely jump out in a day. They whisper across cycles and seasons.
Every two weeks, review like a detective. Which days crash after poor sleep? Which meals bloat? Which meetings spike pain? Use this to craft tiny experiments: swap one food, shift one meeting time, add one recovery habit. We learned that late dinners and back-to-back calls were silent saboteurs.
Bring the pattern summary to appointments. It turns a foggy story into clear hypotheses and helps your team personalize care. Most of all, it gives you proof you are not imagining this. The body is speaking, and now you can translate.
Build and Use a Flare Kit
A flare kit is not defeated. It is dignity in a bag. Our lives by the door, and another copy lives in the car. Heat pad, TENS, prescribed meds, anti-nausea tabs, electrolytes, protein snacks, ginger tea bags, soft leggings, wipes, a small blanket, and a compact hot water bottle.
Add comfort tools you actually use, not what looks good online. Pelvic wand if guided by physio. Breathing prompts on a card. Noise-canceling earbuds for travel. A small notebook to capture what worked and what did not. Keep expiry dates taped on the inside.
Practice the kit when you are not flaring, so it becomes muscle memory. The goal is fewer panicked scrambles and more controlled responses. When a flare hits, reaching for readiness lowers fear, and lowering fear lowers pain perception. Control returns, inch by inch.
Redesign Workloads and Buffers
Pain punishes rigid schedules. We rebuilt work like scaffolding that can flex. Batch deep work into protected windows on lower-symptom days, then keep lighter admin for fragile days. Add buffers around meetings so there is time to stretch, snack, or simply breathe.
Negotiate outcomes instead of hours wherever possible. If you are your own boss, design theme days. If you have a manager, offer solutions: camera-off when needed, asynchronous updates, and earlier starts with earlier finishes. Document what this protects: reliability, quality, and retention.
Use calendar color codes for energy zones. Guard recovery after medical appointments as if it were a meeting with your future self. The aim is not laziness. It is sustainability. A kinder structure preserves the capacity you can spend on life, not just surviving work.
Honest Scripts for Boundaries
Most of us freeze when asked to explain invisible pain. Scripts help you stay calm and clear. Keep versions for boss, colleague, friend, and family. Short, factual, respectful. “I live with a chronic gynecological condition that causes unpredictable pain and fatigue. On bad days, I adjust tasks and communication to stay reliable.”
Offer the plan alongside the boundary. “If symptoms rise, I will message by 9 and shift to offline tasks. Here is how you can reach me for urgent items.” People respond to clarity. It trains others to trust your self-management.
Rehearse the words out loud so they feel like yours. Boundaries are not walls. They are doors that you choose when to open. Confidence grows each time you protect your body without apologizing for its needs.
Map Your Multidisciplinary Care Team
Endometriosis rarely yields to a single clinician. Map a village. A GP who coordinates, a specialist with up-to-date training, pelvic floor physio, pain medicine input, and mental health support. If heavy bleeding or bowel and bladder symptoms dominate, loop in those specialties early.
Write one shared summary you can hand to any new provider: key symptoms, prior imaging and surgeries, meds tried and effects, fertility goals, red flags, and what helps. This prevents the exhausting repetition that steals hope.
Schedule reviews on a cadence, not only in crisis. We learned that planned check-ins catch slow declines before they become avalanches. A team that communicates spares you from being the messenger while you are hurting.
Align Treatment with Fertility Goals
Every decision sits next to family plans, even if you are undecided. Name the horizon you are working with: trying soon, preserving options, or prioritizing pain control now. Ask how each option might touch ovarian reserve, anatomy, or timing.
If surgery is considered, discuss the surgeon’s experience with endometriosis specifically, not generic laparoscopy. Clarify aims: pain relief, fertility optimization, or both. When medications suppress ovulation, plan what that means for trying later and for symptom rebound.
Hold space for grief and hope to coexist. We learned to pace conversations, revisit choices, and bring questions in writing. Treatment aligned with values is not simply clinical. It is humane, and that lowers regret.
Plan Finances Around Flare Windows
Money stress magnifies pain. Build a budget that respects symptom variability. Forecast time off for appointments and likely flare clusters. Create a small emergency buffer for taxis, sick-day meals, and private physio when the wait list is too long.
Automate what you can on good days: prescriptions, insurance claims, and savings transfers. Track hidden costs so you can advocate at work or apply for support programs with clear data. Consider income diversification that tolerates flexible hours.
We found that planning for the dip made us braver about pursuing joy when capacity returned. Financial calm is not about austerity. It is about buying back peace.
Create Rituals for Connection
Illness strains intimacy, not just sex but closeness itself. Build rituals that protect the “us” from the disease. Tea and a ten-minute check-in after work. Gentle walks on low-pain evenings. A weekend breakfast where phones stay away and feelings are allowed.
Name the roles you each take during flares: who handles meals, messages, and medical notes. Gratitude is not corny when pain is loud. Say the small thank-yous out loud. It keeps resentment from taking root.
Plan tiny sparks of joy you can activate on short notice. A favorite film, a new playlist, a slow stretch on the living room floor. Love is not the cure, but it is powerful medicine for the parts of life the disease tries to steal.
Reframing the Impact of Endometriosis
Pain rewrites priorities, but it doesn’t erase identity; it forces us to choose carefully what truly matters. Over time, we learned to swap perfection for presence, speed for steadiness, and schedules for seasons that respect the body.
The hardest shift was admitting that “pushing through” was costing more than it gave. Rest stopped being the enemy of progress and became the condition for it.
On paper, treatments look linear, try this, then that, but real life is loops. Good weeks lull you into hope; a sudden flare humbles you back to first principles. We built anchors: predictable meals, movement that soothes rather than impresses, and days that finish a little earlier than ambition demands.
I used to measure love by fixing things. Now I measure it by how gently I hold the pieces while we wait for better days. Softness is not surrender; it’s a strategy.
When we started naming fears out loud, about work, about intimacy, about the future, the room felt lighter. Secrets are heavy; shared truth is strangely aerodynamic. That honesty made space for joy to return in smaller, sturdier forms.
Friends asked how they could help, and we finally told them. A lift to an appointment. A soup dropped at the door. Not advice, just presence. Community did not cure pain, but it kept us from feeling like we were disappearing.
We learned to celebrate “boring” days like holidays. No drama, just warmth, a tidy kitchen, and the quiet victory of nothing hurting too much. Those are the days that refill a life.
I still remember the night she cried because she laughed, because laughing didn’t hurt for once. I held that sound like a keepsake. This is what we live for: not perfect, but possible. The impact of endometriosis can be devastating, but it does not get the last word.
If you’re reading this in the middle of a hard spell, know that tenderness can coexist with strength. You can widen your margins without shrinking your dreams.
Our story isn’t heroic; it’s ordinary love practiced daily. That’s enough. And on the days it doesn’t feel like enough, we begin again, quietly, together.
Living with the Impact of Endometriosis
We rebuilt our days around honesty instead of heroics. On good mornings she leads, on fragile ones I do; the goal isn’t symmetry, it’s rhythm.
Work shifted from rigid hours to humane outputs. We protect deep-focus windows, plan buffer days after appointments, and treat rest like oxygen rather than a reward.
Pain tried to shrink our world, so we learned to travel differently. We choose apartments near pharmacies, map quiet cafés, and keep flare kits in every bag so spontaneity can survive alongside caution.
Intimacy became slower, kinder, and more conversational. We learned to read each other’s cues, to redefine closeness when touch isn’t possible, and to keep desire alive with patience instead of pressure.
Money conversations used to scare us; now they steady us. We budget for unpredictable weeks, stash a small “flare fund,” and celebrate boring months when the spreadsheet lands close to plan.
Friendships deepened when we stopped pretending. We give people practical ways to help, rides, meals, company, and release the rest without resentment.
I carry the heavy things on hard days and return them on better ones. She lets me protect without feeling powerless, and I let her lead without needing permission.
When fear spikes, we borrow tomorrow’s hope with tiny plans: a film night, a slow walk, a new recipe. Momentum returns in inches and stays longer when it’s humble.
Therapy gave us language; pelvic physio gave us tools; community gave us courage. The body may not always cooperate, but our team and our practices do.
Inside this ordinary life, we’ve found unexpected beauty: fewer apologies, more presence, and a love that measures success in quiet, repeatable moments. In one sentence: learning to live with the impact of endometriosis taught us to choose connection over perfection, and that choice keeps paying us back.
Final Word on the Impact of Endometriosis
There is a moment, usually quiet, when you realise that life cannot be put on hold until perfect health arrives. That is where our story settled: not in surrender, but in a gentler kind of ambition. We stopped measuring progress by how closely we resembled the past and started measuring it by how kindly we met the day we had.
The science taught us to respect biology, to expect variance across cycles, and to plan in seasons rather than in rigid weeks. The clinics and scans and second opinions were not a straight path, yet they gave us language. With language came better questions, with better questions came options, and with options came a sense of agency that pain had tried to steal.
For anyone trying to connect the dots between symptoms, relationships, work, and dreams, the impact of endometriosis is not only medical; it is logistical, economic, and deeply emotional.
Naming that footprint matters. It validates grief for plans that changed, but it also highlights where influence still lives, routines, boundaries, treatments, support, where small, repeatable daily choices restore control and rebuild confidence, even when pain persists.
Work changed because it had to. We learned to prioritise outcomes over optics, recovery over rushing, buffers over bravado. Rest turned from a guilty pleasure into a performance strategy. On difficult mornings, we swapped duties without scorekeeping; on steadier days, we chased goals with a new patience that paradoxically made us more reliable, not less.
At home, we rebuilt intimacy as a conversation, not a test. We learned that closeness can be held in a hand, a glance, a laugh saved for later. We celebrated the ordinary, tidy kitchens, a short walk, a film finished without pausing for tears—because ordinary is where a good life lives most of the time. Hope, it turns out, is cumulative; it grows by being noticed.
We also faced the numbers head-on: time, money, energy. Budgets gained a small line item for flare weeks. Calendars earned blank space. We prepared kits, scripts, and shared notes so that appointments stopped erasing entire days. The practical work was not glamorous, but it lowered panic and lifted control.
None of this makes illness noble. It simply makes room for dignity. And inside that room, love has more air. I hold the heavy things when she cannot; she leads when the ground is steady. We keep choosing each other, and that choice reframes everything, from the way we plan travel to the way we forgive delays. It is not a performance of toughness. It is a practice of tenderness.
If you are just beginning, start smaller than you think. Track patterns. Build your team. Tell one trusted person the truth. Protect sleep like a prescription. Put joy on the calendar before the month fills with obligations. Remember that adaptation is not the end of ambition. It is how ambition survives.
Above all, you are not alone. There is a community learning the same courage, one appointment, one conversation, one ordinary, beautiful day at a time.
You don’t have to pause your life while you wait for perfect health. Start smaller than you think, protect sleep, track patterns, ask better questions, and build a team that sees you. With practical tools and tender boundaries, hope becomes a habit, and ordinary days grow wide enough for love, work, and joy.
If this resonated, leave a comment below and grab your free chapter of “Endo-Tool: Endometriosis for Men,” which is our way to welcome you into a community where we share more freebies, big discounts, and practical love for the road ahead.


About Me
Hi, I’m Lucjan! The reason why I decided to create this blog was my beautiful wife, who experienced a lot of pain in life, but also the lack of information about endometriosis and fibromyalgia for men…
READ MOREImpact of Endometriosis FAQs
1) Why does diagnosis often take so long, and how can I speed it up?
Endometriosis symptoms overlap with other conditions, and imaging can miss superficial disease. You can shorten the path by keeping a symptom diary, bringing a one-page history (key symptoms, treatments tried, red flags), asking specifically for an endometriosis-savvy gynecology referral, and clarifying your goals (pain relief, fertility, both) at the start of each visit.
2) Does endometriosis always cause infertility?
No. Many people conceive naturally. Fertility can be affected by inflammation, adhesions, and ovarian reserve—depending on disease pattern and prior surgery. Optimise general health, treat pain appropriately, and discuss timing with a specialist; options include expectant management, surgery in selected cases, and assisted reproduction when needed. Align choices with your family plans early.
3) What treatments actually help with pain—and how do I choose?
Evidence-based options include NSAIDs, hormonal suppression (e.g., combined pills, progestins), GnRH-based therapies, and expert excision surgery for selected patients. Pelvic floor physiotherapy, pain-science–informed rehab, and mental-health support improve function. Choice depends on symptoms, side-effect tolerance, imaging/surgical history, and fertility goals. Revisit the plan regularly; what helps may change across seasons of life.
4) How do I manage work and disclosure without risking my job?
Shift from hours to outcomes, build buffer time after appointments, and create “flare-day” task lists. Use simple scripts: name the condition, state what adjustments maintain reliability (asynchronous updates, camera-off, flexible hours), and offer a clear escalation path. Track impact and accommodations so you can show that the plan protects performance, not excuses it.
5) I’m a partner—what’s the most helpful thing I can do?
Listen first, believe her pain, and ask what would help today—not in theory. Share logistics (meals, meds, notes), protect rest, and learn the condition so she doesn’t have to educate while hurting. Keep intimacy as a conversation, not a test. Most of all, be consistent: small acts, repeated, restore safety and make room for hope.
Impact of Endometriosis References
- WHO — Endometriosis fact sheet
- The Lancet — Endometriosis: addressing the roots of slow progress (2024)
- Endometriosis UK — Diagnosis survey report (March 2024) (PDF)
- University of York — Global average diagnostic delay ~6.6 years (Feb 2024)
- Systematic review — Prevalence, diagnostic delay and economic burden (2023)
- Longitudinal assessment — Work loss and salary impact (2020)
- Symptom impacts on daily functioning (2023)
- Quality of life review (2024)
- Cleveland Clinic — Endometriosis overview
- Guardian — Linzagolix approved for NHS use (May 2025)
- EClinicalMedicine — Hospitalisations and length of stays in women with endometriosis (2025) (PDF)
- Review — Lifelong impact and comorbid risks (2023)